Introduction
Uterine sarcomas, are neoplasms of the mesenchymal tissue, correspond to 3 to 7% of uterine tumours and about 1% of neoplasms of the female genital tract. Due to their rarity and histological diversity, it is difficult to classify them, identify risk and prognostic factors, and to define a treatment1,2,3,4. Leiomyosarcomas correspond to the most frequent histological type (63%), and are associated with a high recurrence rate (53 to 71%) , even when diagnosed in early stages2. Treatment with tamoxifen is pointed out as a possible risk factor, although in many cases none risk factor is identified1,2.
Abnormal uterine bleeding, a palpable pelvic mass and/or pelvic pain are the most frequent clinical presentations and these can also be manifested in uterine leiomyomas, masking the diagnosis1,2,5. For this reason it is important to exclude the presence of a leiomyosarcoma when studying a polymyomatous uterus, especially if we are in the presence of a uterine tumour that grows after menopause2. Less often, they present with other manifestations, including hemoperitoneum (due to spontaneous rupture of the tumour), with only a few cases described in the literature5,6,7,8,9,10. The authors describe a case of a uterine leiomyosarcoma, with spontaneous rupture.
Clinical case
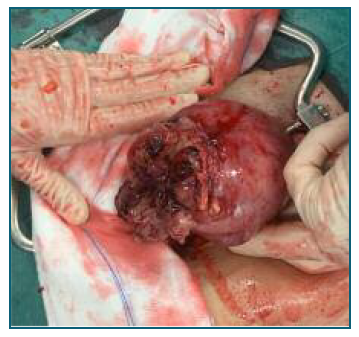
We present the case of a 50-year-old Caucasian woman admitted for elective surgery due to a rapidly growing uterine leiomyoma. From her background, she was a nulliparous woman, with non-medicated dyslipidaemia and a BMI of 19. She had no previous surgeries or smoking habits. Regarding family history, she has two paternal female cousins with breast carcinoma. In the history of the current disease, the patient mentioned irregular menstrual cycles with 5 months of evolution, which led her to go to the gynaecology emergency department for an abnormal uterine bleeding one and a half month before surgery. In this episode, a transvaginal ultrasound examination identified a polymyomatous uterus (the largest leiomyoma with 60*60 mm) and mild anaemia (Haemoglobin 10.5 g/dl), and she was medicated with desogestrel and oral iron. One week after going to the emergency department, the patient scheduled a private gynaecology appointment. In the office evaluation, the aforementioned leiomyoma had 77*86*96 mm in dimensions, a FIGO classification type 1-6, vascularization score 2 (Figure 1), but the patient didn’t present the previous examination and a subsequent reassessment was scheduled. A month later, due to maintaining the abnormal vaginal bleeding, she contacted her assistant gynaecologist who, upon reassessing, found an increase in the dimensions of the uterine mass, being urgently referred to the gynaecology oncology department and, after discussion in a multidisciplinary team, surgery was scheduled to the following week.
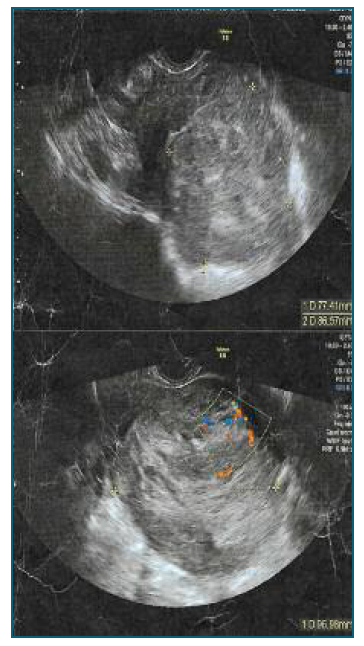
Figure 1 Ultrassound images of the tumour, with dimensions of 77*86*96 milimiters, and vascularization.
During the surgery, an enlarged uterus was observed with the presence of clots on the uterine fundus, adherence of small bowel loops to the left and adhesions of the sigmoid colon to the left uterine horn. After lysis of the adhesions, a rupture of the lesion was seen (occurred preoperatively), with the presence of coagulated content and material suggestive of myometrial tissue released in the pelvic cavity (Figure 2). Regarding the adnexa, the left ovary was atrophic and with adhesions to the colon, and the fimbriae of the right tube adhered to the ipsilateral utero-ovarian ligament, without other alterations. Surgery proceeded systematically with total hysterectomy and bilateral adnexectomy. After the closure of the vaginal vault, general surgery support was requested to evaluate the intestinal segments. Segmental resection of the small intestine was performed with a 55 GIA (5-6 centimetres from the proximal ileum) with latero-lateral mechanical anastomosis. Then an evaluation of the sigmoid colon was carried out, due to the presence of inflammatory/tumoral tissue involving some of the epiploic appendix but without direct invasion of the intestinal wall, it was decided to excise this tissue and send it for anatomopathological examination. All pieces were sent for anatomopathological study. After extensive cleaning of the cavity and review of the haemostasis, a drain was placed in the right iliac fossa and the abdominal wall was closed in layers.
In the postoperative period, when questioned, the patient reported a sudden and intense pain about an hour before surgery, requiring analgesia, which probably corresponded to the moment of rupture. Hospitalization was uneventful, with discharge on the sixth postoperative day, medicated with low molecular weight heparin for thromboprophylaxis, oral iron and painkillers.
The anatomopathological study of the uterus identified 3 nodules. The largest, with dimensions of 6.5*6 cm, in the microscopic study showed a fusocellular neoplasm with moderate atypia, multifocal areas of marked atypia, necrosis and a mitotic index greater than 10 per 10 fields of high magnification, characteristics suggestive of uterine leiomyosarcoma, with serosa involvement. Regarding the immunocytochemical study: CD 10 negative; CD34 negative; Caldesmon Positive; Desmin Positive; HMB45 Negative; Oestrogen receptors positive; Progesterone receptors positive; and SMA positive. The left utero-ovarian ligament, the serosa of the sigmoid colon and the biopsy of the pelvic peritoneum showed involvement by the previously described neoplasm. Regarding the pathological staging, it was a pT3a tumour (8th edition AJCC) and a FIGO IIIA staging.
Two weeks after the surgery, in a multidisciplinary team appointment, given the anatomopathological result and the imaging study showing signs of tumoral lesion in the splenic angle of the colon and implants at the pelvic level, the patient was proposed for a new surgery. Thus, four weeks after the initial surgery, the patient underwent on an exploratory laparoscopy, which was converted into laparotomy after evaluation of the cavity and possibility of excision of lesions, followed by a left hemicolectomy, with high anterior resection of the rectum, enterectomy, omentectomy, peritoneal biopsies and excision of a node in the vaginal vault. The anatomopathological study showed, in the left hemicolectomy specimen, anterior resection of the rectum and enterectomy, several nodules with signs of leiomyosarcoma, the largest with 15 mm.
In a new multidisciplinary team appointment, it was decided to start chemotherapy (gemcitabine and docetaxel). After 14 months since the first surgery, the patient presents clinical and imaging progression of the disease, maintaining cycles of chemotherapy, with different combinations of drugs through this time.
Discussion
Uterine leiomyosarcomas are rare and aggressive neoplasms5,7,9,11. Prognosis is based on FIGO staging for this type of tumour, mitotic count and tumour size10. The five-year survival rate in leiomyosarcomas varies between 15-25%, being associated with a high risk of recurrence and metastasis, with hematogenous dissemination being the main route2,3,4.
When a uterine mass is suspected, the first-line study should be a transvaginal ultrasound with Doppler evaluation, which can be complemented with a pelvic magnetic resonance1. However, the diagnosis is histological. The mitotic index is an important parameter to establish the diagnosis and prognosis1,2,10,12.
As mentioned, uterine tumours most often present with abnormal uterine bleeding, a rapidly growing mass or compressive symptoms, spontaneous rupture is an atypical and rare presentation1,8,9,10. In the literature only a few cases of uterine sarcomas with hemoperitoneum as an initial finding, due to tumour rupture, are described5,6,7,8,9,10. A possible mechanism described for this rupture is the degenerative changes, tissue infarction and tumor necrosis7,13,14. In the present case, the rupture occurred in the hospital shortly before surgery, hence the initial finding was not a hemoperitoneum. This presentation, being atypical, cannot be used as a prognostic marker9.
The treatment of these tumours is surgical and they are usually associated with a poor prognosis, especially if there is tumour dissemination in the pelvic cavity1,7,15. Hysterectomy with or without adnexal preservation in early cases has good results in the survival of these patients1,4,15. The role of chemotherapy and its possible benefit in leiomyosarcomas isn’t fully established, but since they are tumours with a poor prognosis, it is often associated in their treatment, either for therapeutic or palliative effects3,4,15. Adjuvant pelvic radiotherapy and pelvic lymphadenectomy showed no effect on survival and are not indicated4. Therefore, palliative care should be called early, especially if disseminated disease is present15.
Uterine leiomyosarcomas present a clinical challenge, either for being infrequent, for their aggressiveness, and because there is no consensual therapeutic algorithm, so a multidisciplinary approach should be mandatory. This atypical manifestation, although rare, should be taken into account in women with hemoperitoneum and suspected uterine mass.
Authors’ contributions
Carlos Macedo: Conceptualization, Writing - original draft, Writing - review & editing
Rita Leiria Gomes: Writing - review & editing
Filipa Abreu Santos: Conceptualization, Writing - review & editing, Resources
Hugo Gaspar: Writing - review & editing, Resources
Manuel Pontes: Writing - review & editing, Resources