Introduction
Obesity is one of the risk factors that contributes the most to the burden of disease in Portugal. It increases the risks of thromboembolic events, such as ischaemic heart disease (IHD), stroke, and venous thromboembolism (VTE) which is independent of age and smoking habits of the individual. About 32.1% of Portuguese woman between the ages 25 and 74 in 2015 were obese1.
In overweight and obese women without other cardiovascular risk factors or previous medical problems all methods of contraception are eligible2. However, the risk of VTE increases with increasing body mass index (BMI) and almost doubles when the BMI ≥ 35 kg/m2.2-7
For combined estrogen-progestin hormonal contraceptives (CHC), i.e., oral pill, transdermal patch, and vaginal ring, both hormonal components can impact the risk of thrombosis, but the greater risk comes from the estrogen component2-7.
For this reason, according to the most recent scientific evidence, the use of CHC in women with a BMI ≥ 35 kg/m2 is classified as category 3 meaning that the use of the method is not recommended unless another method is not available or accepted2,4-6. Obese women with a BMI ≥ 35 kg/m2 should preferably use non-hormonal or progestin-only methods of contraception2-5.
The family health team plays a central role in the surveillance of women included into the family planning (FP) program. It is essential to raise the awareness of health professionals to this issue, encouraging the establishment of health education strategies, streng-thening hygienic-dietary measures, evaluating the adequacy of the treatment and the patient’s adherence to the therapeutic plan.
This study aims to assess the contraceptive methods used in women with class 2 obesity or higher in nine Primary Healthcare Units (PHU) in northern Portugal.
Methods
Study Design, Setting, and Population
This multicentric, retrospective, observational, cross-sectional study included all women between 15 and 49 years old enrolled in FP program, with class 2 obesity or higher (BMI ≥35 kg/m2), from nine PHU from the Grouped Health Centers of Gaia and Espinho-Gaia in northern Portugal.
Data Sources
Data was obtained through MIM@UF® database and individual electronic medical record system, Sclínico®. The data extraction through MIM@UF® included the following: age; BMI; and FP enrollment status. We then extracted the following data through Sclínico®: BMI; contraception method; date of last appointment; and previous thromboembolic conditions (stroke, IHD, VTE) documented through diagnosis codes from the International Classification of Primary Care, 2nd edition (ICPC-2): K74, K75, K76, K90, K91, K93 and K94.
Participants
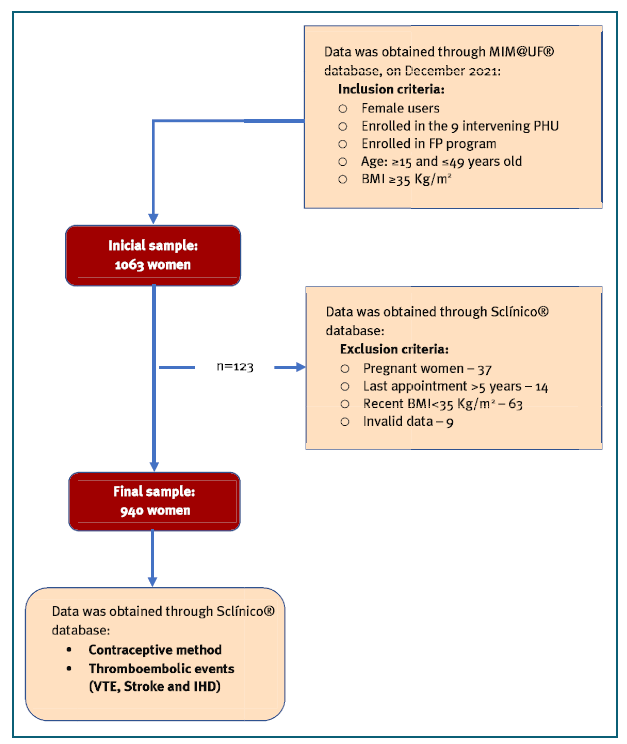
Participants were included if they fulfilled the following criteria in December 2021 in MIM@UF® database: Age: ≥ 15 and ≤ 49 years old; Enrolled in FP program; and BMI ≥ 35 kg/m2. We excluded women: who were pregnant; who had a more recent BMI measure < 35 in Sclínico®; who had not been to a medical appointment in the previous five years; who had invalid data (such as gross mistakes in BMI); and who were not enrolled in FP program in Sclínico®.
Statistical Analysis
A descriptive analysis was conducted, using Microsoft Excel® 2007 and GraphPad Prism® software version 6.0. For categorical variables, absolute and relative frequencies were calculated. For quantitative variables, average and standard deviation were calculated.
Contraceptive method categorization was made according to Sclínico® classification, as follows: none, CHC, progestogen-only pill (POP), progestogen-only injectables (PInj), progestogen-only implant (PImp), levonorgestrel intrauterine system (LNG-IUS), copper intrauterine contraceptive device (Cu-IUCD), barrier methods, natural methods, permanent methods.
For analysis purposes and when considered adequate, some methods were aggregated in broader categories as follows: Cu-IUCD, barrier methods and natural methods were included in the non-hormonal methods (NHM); and POP, PInj, PImp and LNG-IUS were included in the progestogen-only (PO) methods.
BMI was both a quantitative and a categorical variable. When deemed appropriate, it was categorized according to obesity class: class 2 (BMI ≥ 35 kg/m2 and <40 kg/m2) and class 3 (BMI ≥ 40 kg/m2).
Previous thromboembolic conditions were aggregated in the following manner: K74, K75 and K76 were accounted as IHD; K90 and K91 were accounted as stroke; and K93 and K94 were accounted as VTE.
In women with previous thromboembolic conditions, we gathered information on the method being used at the time of the event and 6 months after it. In those with VTE events we further classified them into deep vein thrombosis (DVT) and superficial vein thrombosis (SVT) as found in their clinical records.
The collected data was stored in a password-protected, electronic database. The data are anonymous, with no association with name or any other data that unequivocally identifies the users or the healthcare unit. Therefore, the requirement for informed consent was waived.
The study was approved by the Clinical Councils and Executive Boards of the aforementioned Grouped Health Centers and by the Ethics Committee of Nor-thern Portugal’s Regional Health Administration (Reference CE/2021/99).
Results
Population characteristics
After filtering and application of inclusion and exclusion criteria, 940 women were selected (Graph 1). included population had a mean age of 36.8 ± 8.8 years, median 38, and a mean BMI of 39.2 ± 4.0 kg/m2. Of this sample, 68.6% (n=645) were classified as obesity class 2.
Contraceptive choice
Regarding the contraceptive method, at the time of the analysis, 36.2% (n=340) were using PO, 27.7% (n=260) were taking CHC, 12.8% (n=120) were with a NHM, 6.4% (n=60) were with permanent methods and 17.0% of women were not using any type of contraception (n=160).
In the PO group, the majority were with a POP (70.9% (n=241)), 14.7% (n=50) were with LNG-IUS, 13.8% (n= 47) were with PImp and 0.6% (n=2) were with PInj.
In the NHM group, 55.8% (n=67) were with barrier methods; 37.5% (n=45) were with Cu-IUCD and 6.7% (n=8) were with natural methods.
CHC vs progestogen-only
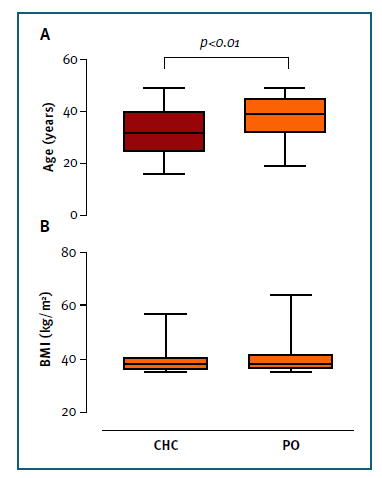
Women on CHC were significantly younger compared to women on PO (32.5 ± 8.7 years vs 37.7 ± 7.9 years; p<0.01) (Graph 2, panel A), but there are no significant differences in the BMI (Graph 2, panel B). It is important to notice that in both obesity classes the most chosen contraceptive method was PO. However, 28.4% and 26.1% for class 2 and 3 were taking CHC (Graph 3, panel A).
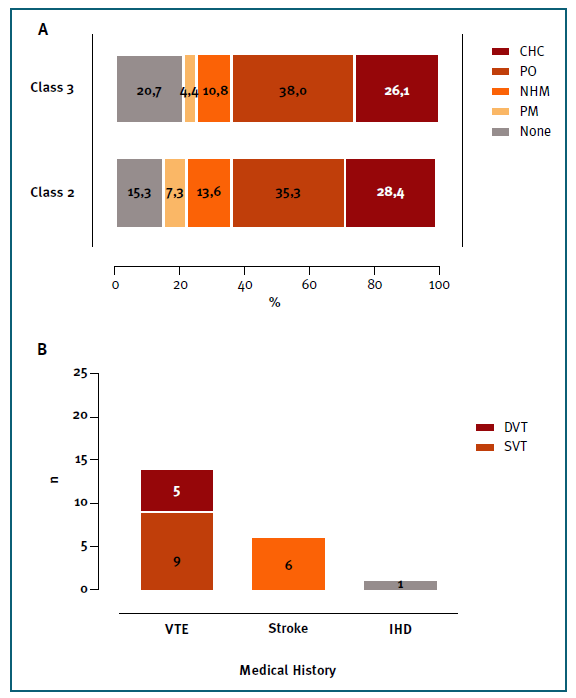
Graph 3 Panel A - Distribution of contraceptive method by class of obesity; Panel B - Thromboembolic .events in women with BMI ≥ 35 Kg/m2. CHC - combined hormonal contraception; PO - progestogen-only; NHM - non-hormonal methods; PM - Permanent Methods; DVT - Deep Vein Thrombosis; SVT - Superficial Vein Thrombosis; VTE - Venous Thromboembolism; IHD - ischaemic heart disease.
Thromboembolic Events
Twenty-one women had a thromboembolic event (2.2%): 14 (1.5%) were VTE (nine (0.9%) were SVT and five (0.6%) DVT), six (0.6%) were strokes and one (0.1%) acute myocardial infarction (AMI) (Graph 3, panel B).
The mean age of women with thromboembolic events is 41.6±6.8 years, with a median of 44 years. The mean BMI is 39.1±4.0 kg/m2.
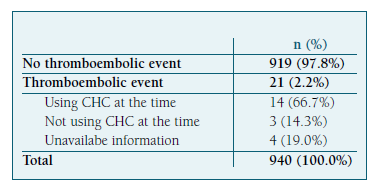
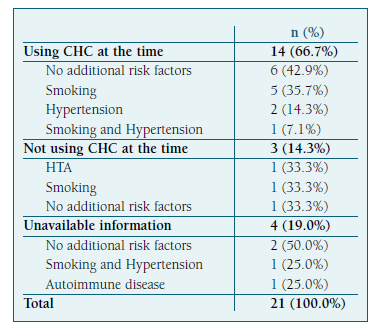
Fourteen women (66.7%) were taking CHC at the time of the event (eight SVT, three DVT and three strokes) (Table I). Of this group, eight (57.1%) kept CHC six months after the event and three (21.4%) maintained it to date.
Currently, of the 21 women who had thromboembolic events, 12 are on PO, five with NHM (Cu-IUCD and barrier method), three with CHC and one with a permanent method.
There are no data regarding the contraceptive me-thod at the time of the event for four women and regarding the change of method in one woman.
Of the 21 women with a thromboembolic history, nine (42.9%) have no additional thromboembolic risk factors other than obesity, six (28.6%) are smokers, three (14.3%) are hypertensive, two (9.5%) have more than one risk factor (thrombophilia and smoking, hypertension and smoking) and one (4.8%) has autoimmune disease (Table II).
Discussion
The results obtained in this study are a wake-up call for the medical community. The data show that 27,7% of the obese women are still on CHC. PO methods are the main contraceptive method (36,2%) in the presented sample, with POP representing the majority.
Other authors have already addressed the prescription of contraceptives to obese women. A study carried out in Sweden, which included 371 obese women, concluded that the most frequently prescribed method to obese women was POP (44%) followed by CHC (21%). However, when specifically assessing contraception prescriptions in the group of women with class 2 and 3 obesity (n=107), they found that the most prescribed contraceptive was POP (56,1%), followed by Cu-IUCD and PInj (each 12,1%), PImp (11,2%) and LNG-IUS (4,7%). Only 2,8% used CHC. This is in stark contrast with our findings, which should make us look for strategies for more adequate prescription patterns.8 This might be because the use of POP is far more common in Sweden than in other parts of the world.8
On the other hand, 17% of the obese women used no contraception method which is in line with Western European (23,2%) and American (20,5%) prevalence found in previous studies9,10. A study of the National Survey of Family Growth in the United States reported that roughly half of the women in reproductive age willing to start a birth control method were overweight or obese, however the included population of obese women reported less use of systemic hormonal methods and demonstrated that contraceptive use varies with BMI status11.
In the study carried out in the United States, the main reasons for not using birth control were “didn’t really mind if they got pregnant”, “worried about the side effects of birth control” and “do not think they can get pregnant”10.
After extensive review, we could not find comparable data from Portuguese studies. However, 6% of sexually active Portuguese women do not use any contraceptive method12. As our study did not collect data regarding sexual activity, comparisons cannot be made.
It would be interesting to research the reasons behind such choices in the obese population and to ascertain if these would be different from the non-obese population.
More studies are needed to investigate the prescription of contraceptives, the adherence to treatment, and possible side effects of these methods among women with obesity in Portugal.
When we analysed the number of thromboembolic events in the sample, 21 (2.2%) had a thromboembolic event, with nearly 67% taking CHC at the time it occurred. Nowadays, 21% still take CHC. Having a thromboembolic event is an absolute contraindication/category 4 for CHC. Whether this is a result of clinicians’ passivity to alter methods according to different needs and circumstances over time or women’s desire to maintain the same type of contraception is not known.
Since there are some unavailable data on the use of CHC at the time of the event, we can not calculate the relative risk of VTE in our sample, but, according to the literature there is a 10-fold higher risk of VTE compared to non-obese nonusers13.
The absolute risk of VTE is an important consideration, particularly because among healthy women of reproductive age, VTE is considered a rare event (2-4 events per 10 000 women per year)4. The use of CHC increases the absolute risk to 4.5 to 14.5 per 10 000 woman-years14. While both CHC use and obesity increase risk for VTE, given the wide range of baseline estimates and heterogeneity in the magnitude of effect of CHC’s and obesity both independently and jointly, it is not possible to estimate absolute risk of VTE among women with both of these risk factors. A review of recent cross-sectional studies strongly suggests a dose-response relationship between BMI and VTE risk as well a possible interaction between BMI and CHC-use, making it likely that the absolute risk of VTE is further elevated in obese CHC-users and continues to increase with increasing BMI14.
In addition, the women enrolled in our study had several known non-modifiable and modifiable VTE risk factors that are identified by the Practice Committee of the American Society for Reproductive Medicine as responsible for increasing the risk of thrombotic events in the setting of CHC use: tobacco use, age (>35 years), obesity, and the presence of hereditary thrombophilias13. These facts possibly explain the higher than expected prevalence of VTE in our sample.
To our knowledge this is the first multicentric study describing the contraceptive methods used by women of reproductive age with class 2 or class 3 obesity in the Primary Health Care setting in Portugal. Women between 15 and 54 years-old are enrolled in the FP program but in the current study we adopted the World Health Organization definition of women of reproductive age which includes females between 15 and 4915.
By using the ICPC-2 classification to retrieve the thromboembolic events and the SClínico® own codification to collect contraceptive methods we guaranteed a straightforward methodology that could be easily replicated in future studies.
A limitation of our study relates to data extraction, as we found sporadic unmatching data between the two used databases, ultimately leading to selection bias. Hence, we excluded some women that were first retrieved through the MIM@UF® database and were found to have more updated information in Sclínico® (e.g. BMI was under 35 kg/m2). Likewise, we might have unknowingly excluded women that had inclusion criteria. This can be attributed to the fact that the data on MIM@UF® has a delay of a few months, while in Sclínico® it is possible to retrieve it manually over time. Furthermore, the population is subject to the bias of Primary Health Care users and may not reflect the general Portuguese population.
The exclusion of women lacking or having outdated records in Sclínico® regarding the contraceptive me-thods, leads to further selection bias.
To define thromboembolic events we selected the diagnostic codes (K74, K75, K76, K90, K91, K93 and K94) included in the ICPC-2 and screened for the individuals with documented events. Notwithstanding, due to a partly subjective nature of the codification process, related to medical staff difficulties, mistakes or omissions in selecting the appropriate diagnosis codes, caution is needed when interpreting data’s magnitude and accuracy.
We also found failures to record the type of contraceptive method at the time of the thromboembolic event and after 6 months. The reason for discontinuing the methods was also not recorded.
Future studies may be performed and include more centres to compare our results with other PHU in Portugal. It would also be interesting to explore the exact type of estrogen containing method used. A cohort prospective study would help to clarify the relationship between women using a CHC method and thrombotic events.
Conclusion
By analysing records of nine PHU this study has shown that the most commonly prescribed contraceptive me-thod in women with class 2 and 3 obesity was PO me-thods. Surprisingly, many women in this group were prescribed CHC despite most clinical guidelines.
We also found a higher than expected prevalence of thromboembolic events reported.
We regard continuous learning essential when providing healthcare, so that professionals can recognize women at risk and propose appropriate method changes.
Our study draws attention to the need to contradict a possible existing attitude towards clinicians’ therapeutic inertia, raising the awareness about the importance of adequate prescription routines according to current guidelines on contraception. It also reaffirms the need for appropriate medical records that can guarantee high-quality studies. Moreover, empowering women with knowledge is paramount to maximize a good and healthy life.
Author contributions
Conceptualization and Study Design: Ana Catarina Araújo, Ana Isabel Silva, Carla Cardoso, Catarina Baía, Daniela Saraiva, Eduarda Alves, Leonardo Napoleão, Luís Lira, Pedro Sonié, Sara Albuquerque, Teresa Rebello Andrade
Data collection: Ana Carolina Costa, Ana Vidal, Eduardo Almeida, Filipe Santos, Inês Rodrigues, Joana Silva, João Louçano, Mariana Cruz, Mariana Horta, Marta Perro Neves, Paulo Graça, Raquel Borges, Sara Leite, Sara Teixeira
Formal analysis: Catarina Baía, Eduarda Alves, Luís Lira, João Louçano, Mariana Horta
Writing - original draft: Daniela Saraiva, Filipe Santos, Inês Rodrigues, Joana Silva, Leonardo Napoleão, Sara Leite, Teresa Rebello Andrade
Writing - review: Ana Catarina Araújo, Ana Carolina Costa, Ana Isabel Silva, Ana Vidal, Carla Cardoso, Eduardo Almeida, Leonardo Napoleão, Mariana Cruz, Marta Perro Neves, Paulo Graça, Pedro Sonié, Sara Albuquerque, Raquel Borges, Sara Teixeira