Introduction
Primary malignancies of the vagina are rare, contributing to only 3% of malignancies of the female genital tract. Squamous cell carcinoma is the most common histological subtype. Sarcomas represent only 3,1% and leiomyossarcomas only a fraction of these, thus being extremely rare1), (2. Due to carcinogenic properties of ionizing radiation, the development of malignancies secondary to radiotherapy has become a rising problem among oncologic survivors, with an estimated incidence of 20%3.
Depending on their size and location, vaginal neoplasms may present as an asymptomatic vaginal mass, vaginal discharge or haemorrhage1), (4. Staging is based on the clinical findings but magnetic resonance imaging (MRI) has great value in determining local extension5. Leiomyosarcomas arise mainly from the smooth muscle and the diagnosis is confirmed histopathologically. (6 The primary treatment generally consists on tumour resection with adequate margins. The next ideal strategy has not yet been defined2.
Being a rare entity, there is lack of evidence-based information about leiomyossarcomas of the vagina. Therefore, it is essential to enrich the literature about these potentially aggressive malignancies that may be secondary to pelvic irradiation. We present a case of a leiomyosarcoma of the vagina in a female patient previously submitted to radiotherapy for an endometrial carcinoma.
Case report
A 65-year-old postmenopausal woman presented to the urgent care department with vaginal bleeding. Her past medical history was significant for a grade 3 mixed serous and clear cell carcinoma of the endometrium diagnosed 11 years earlier, which involved more than half of the myometrium without invading the serosa, corresponding to a stage IB in the FIGO (International Federation of Gynecology and Obstetrics) staging system and pT1cN0M0 in the TNM system. Surgical treatment consisted on total hysterectomy with bilateral oophorosalpingectomy, pelvic and lumboaortic lymphadenectomy and omentectomy. She underwent adjuvant chemotherapy, followed by vaginal brachytherapy (2800 cGy) and external pelvic radiotherapy (5040 cGy). She had no other relevant personal or familiar history.
On gynecological examination there was a palpable hard mass in the latero-posterior wall of the vagina of approximately 5 centimetres, condylomas around the vaginal introitus and local changes secondary to radiotherapy. Vaginal biopsy revealed a spindle-cell mesenchymal lesion with a pseudosarcomatous myofibroblastic proliferation.
Laboratory studies revealed a slight reduction in hemoglobin concentration (11.6 g/dl) and increase in creatinine (1.42 mg/dL). CA125 (cancer antigen 125) levels were within normal range (13 U/ml). Genetic testing wasn’t performed.
Pelvic MRI (Figure 1 A, B) showed a lobulated mass located posteriorly in the inferior third of the vagina, showing high signal intensity on T2-weighted images, slightly heterogeneous, measuring approximately 3.6 × 5 × 4.8 cm and demonstrating diffusion restriction. It invaded the anal canal, the elevator muscle of anus and contacted with the lower rectum. It had apparent fat cleavage plan with the urethra and bladder and there were no pelvic or lumbo-aortic lymphadenopathies. Thus, this lesion exhibited aggressive imaging features and favoured diagnostic hypothesis of sarcoma. No lung nodules were detected on chest Computed Tomography (CT) scan.
Given patient’s age and the possibility of urethral preservation, the multidisciplinary team agreed to offer tumour surgical resection. Extemporaneous histological examination revealed atypical spindle-cells proliferation with involvement of anterolateral right margin of the vagina. The patient was then submitted to abdominoperineal amputation of rectum with terminal colostomy, partial vaginectomy with preservation of anterior and left walls and right hemivulvectomy. Grossly, the tumour showed an ulcerated area in the posterior wall of the vagina and invasion of the anal canal and distal rectum (Figure 1 C, D). Histologically, it was composed of spindle shaped cells (Figure 1 E), some less cellular areas with marked fibrosis and extensive areas of coagulative necrosis with bacterial superinfection and fibrinoid necrosis of blood vessels, corresponding to areas of necrosis in about 20-25% of the tumour’s volume. When examined at high magnification, the spindle cells showed evidence of moderate atypia and intense mitotic activity (28/10 high-power field). Immunohistochemically, tumour showed strong and diffuse expression of vimentin, smooth muscle actin, caldesmon and CD99 (Figure 1 F-I). Based on histopathological results, the tumour was classified as a high grade leiomyosarcoma, with tumoral involvement of the vaginal margin.
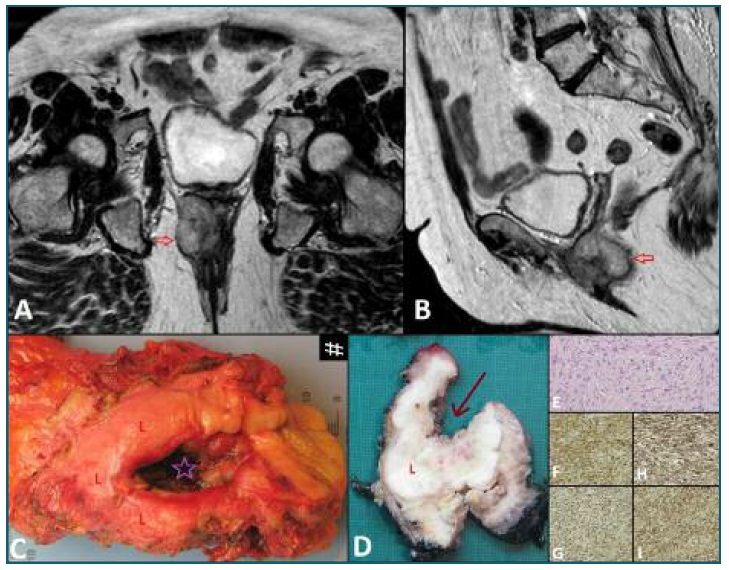
Figure 1 Pelvic T2-weighted coronal (A) and sagittal (B) MR images showing a lobulated mass (arrow) with high signal intensity located posteriorly in the inferior third of the vagina and invading the anal canal. Gross specimen (C,D) showing the lesion (L) with an ulcerated area (star in C, arrow in D) in the posterior wall of the vagina. At high magnification, the lesion is composed of fascicles of spindle shaped cells (E, H&Estain X 200) with expression of smooth muscle actin (F, X 100),Vimentin (G, X 100), caldesmon (H, X 100) and CD99 (I, X 100),
After surgery the patient was discharged and underwent adjuvant chemotherapy with Doxorubicin. Revaluation pelvic MRI two months after surgery revealed no signs of recurrence or residual disease. Four months later, one moth after chemotherapy ended, a Positron Emission Tomography - Computed Tomography (PET-CT) scan showed areas of increase uptake of 18F-FDG (fluorodeoxyglucose) in the presacral region (Figure 2 A), suggestive of active disease (peritoneal implants) and also in multiple lung nodules. Subsequent pelvic MRI confirmed the presence of two nodules anterior to the sacrococcygeal transition measuring 27 × 19 mm and 25 × 13 mm, and another one adjacent to posterolateral wall of the bladder with 14 × 10 mm, all of them showing restricted diffusion, suggestive of tumour recurrence (Figure 2 B-E). Given the pelvic recurrence and lung metastasis, patient resumed chemotherapy - Gemtacitabine and Docetaxel - with dose reduction after the first cycle due to pancytopenia and deterioration of liver and kidney function. After 3 cycles of chemotherapy PET-CT scan revealed increase in the number, size and metabolic activity of the previously described lesions. She underwent 4 cycles of another chemotherapy - Trabectedin. Soon after, she was admitted for diarrhoea with dehydration and reduction of urinary output. An abdominal ultrasound revealed two hypoechoic liver nodules consistent with metastasis and right hydronephrosis. A percutaneous nephrostomy was performed. A month later a head CT was performed due to altered state of consciousness, left hemiparesis and epileptic episode, revealing multiple brain metastasis. She passed away soon after being admitted in a palliate care unit.
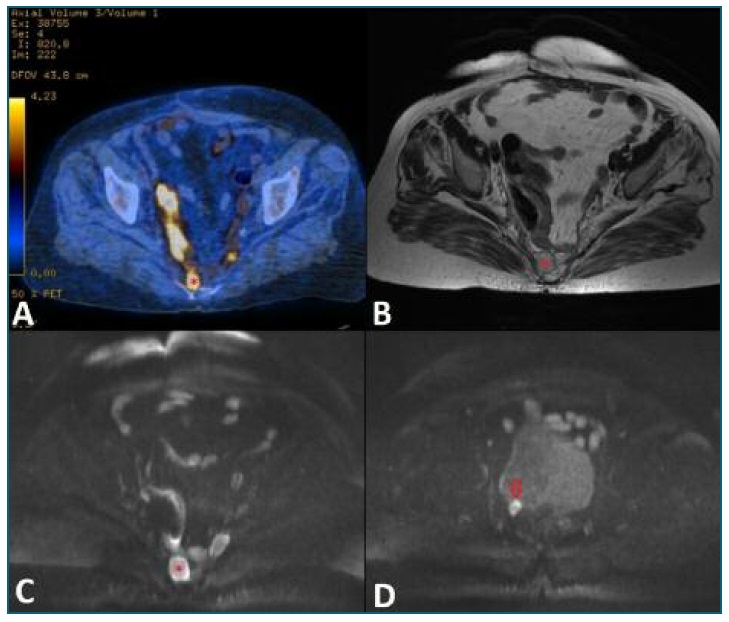
Figure 2 PET-CT scan (A) showing areas of increased uptake of FDG-F18 in the presacral region suggestive of active disease (*). On T2-weighted axial MR image (B) the nodule is hypointense (*) and exhibit significant restriction of diffusion on diffusion-weighted axial MR image (C), suggestive of tumour recurrence. Similar lesions were detected adjacent to posterolateral wall of the bladder (arrow at D).
Discussion
Late neoplasms secondary to radiotherapy may arise in patients treated for uterine cancer, given their longer survival. (7), (8 The estimated rate of radiation-related sarcomas ranges from 0.03 to 0.8%. Its incidence tend to correlate with total radiation dose, with most series reporting doses of 1600 to 11200 cGy. The total dose received by our patient was 7840 cGy. They arise most commonly after radiation therapy for breast cancer, followed by lymphomas. Those in gynecologic tract are relatively rare9.
Distinguishing between a radiation-induced and a primary sarcoma can be difficult. Some authors consider them post-radiation if they arise inside the irradiated field after a latent period of at least 3 years, with different histology from the primary lesion3), (11. In the present case a leiomyosarcoma of the vagina was diagnosed 11 years after pelvic irradiation of endometrial cancer.
Most vaginal sarcomas are asymptomatic. Others present with swelling near the introitus, which may disturb urination, defecation or sexual intercourse. Vaginal hemorrhage (as experienced by our patient) and discharge are late signs. (10 At physical examination most patients present with palpable lumps covered with normal vaginal mucosa and in patients with advanced tumours brittle exophytic polyps or necrotic vaginal masses may me palpated6.
Differential diagnosis of vaginal swelling include vaginal cysts, benign and malignant primary neoplasms such as squamous cell carcinoma (the most common histological subtype of vaginal malignancies), adenocarcinoma and sarcoma, as well as metastasis5), (10.
Leiomyosarcomas are difficult to diagnose preoperatively. They develop more frequently on the anterior wall of the vagina and those malignant are more common on the posterior wall4), (6. The case described was consistent with this tendency, arising from the posterior wall and turning out to be malignant.
The limited reports about leiomyosarcomas of the vagina suggest that they may have imaging features similar to leiomyosarcomas elsewhere. These include ill-defined irregular heterogeneous and locally infiltrative masses with areas of necrosis and hemorrhage in the vagina, exhibiting intermediate to high signal intensity on T2-weighted images and low to intermediate signal intensity on T1-weighted images, showing early peripheral enhancement with gadolinium with progressive heterogeneous fill-in on delayed images or diffusely heterogeneous enhancement owing to the presence of areas of necrosis or hemorrhage5.
Diagnosis is usually confirmed histologically. Leiomyosarcoma stains for epithelial antigens (cytokeratin and epithelial membrane antigen) and muscle elements (muscle actin and desmin), differentiating it from undifferentiated epithelial tumors or other sarcomas. (2), (12 The 2 most common histologic subtypes of radiation associated sarcoma are angiosarcoma (mainly in the breast) and unclassified sarcoma. Several genetic changes have been associated to the their pathogenesis and hopefully effective therapeutic agents will eventually become available based on future knowledge in this area13), (14. Our patient had no genetic studies.
Treatment of sarcomas of the vagina depends on patient’s age and health status, location and size of the tumour, need of maintenance of vaginal function and stage of the disease. Given the scarcity of evidence-based data, treatment of leiomyossarcomas of the vagina is frequently extrapolated from squamous cell carcinomas1), (10. Due to its high rate of recurrence and great potential of hematogenous spread, it is frequently indicated radiotherapy and/or chemotherapy after surgery, especially in patients with metastasis, invaded margins and risk factors for early recurrence, including tumours with 3 cm or more, irregular contour, cellular atypia, high mitotic activity and poorly differentiation15.
Tumour staging has the greatest impact on prognosis. MRI may help in determining primary tumour size and local extension. PET-CT may play a role in identification of metastasis, specially in advanced stages1. Globally, 37% of vaginal cancers are diagnosed at stage II and 37% at stages III or IV. Sarcomas have an even worse prognosis and frequently patients are not candidates to surgical treatment due to the advanced stage of the disease1. The present case illustrates the expected reserved prognosis of these malignancies.
Conclusions
Leiomyosarcomas of the vagina are extremely rare aggressive malignancies that may be induced by pelvic radiotherapy, appearing years latter with imaging features indistinguishable from those sporadic. Given the lack of data published about them, there are no standardized therapeutic recommendations. We present a case of a rare sarcoma of the vagina developed 11 years after postoperative pelvic radiation therapy, with poor outcome, motivating the need of further studies regarding its treatment.














