Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.14 no.2 Coimbra jun. 2020
CASE REPORT/CASO CLÍNICO
Mesonephric hyperplasia can cause abnormal papanicolaou smears: a case report
Hiperplasia mesonéfrica pode causar alterações na citologia cervical: descrição de um caso clínico
Isabel Pedrosa1, Filipa Alpendre2, Rita Sousa3, Sofia Raposo Dinis4, Paulo Figueiredo5
Instituto Português de Oncologia Francisco Gentil Coimbra
Centro Hospitalar do Baixo Vouga, Aveiro, Portugal
Centro Hospitalar Lisboa Central, Portugal
1 Interna de Formação Específica de Ginecologia e Obstetrícia, Centro Hospitalar do Baixo Vouga, Aveiro, Portugal
2 Interna de Formação Específica de Ginecologia e Obstetrícia, Centro Hospitalar Lisboa Central, Portugal
3 Mestrado em Ginecologia Oncológica, Faculdade de Medicina da Universidade de Coimbra, 2010. Grau de consultor em Ginecologia/ Obstetrícia, 2016. Subespecialista em Ginecologia Oncológica, 2017. Instituto Português de Oncologia - Francisco Gentil, Coimbra, Portugal
4 Assistente Hospitalar em Ginecologia, Instituto Português de Oncologia Francisco Gentil Coimbra
5 Diretor do Serviço de Anatomia Patológica do Instituto Português de Oncologia - Francisco Gentil, Coimbra, Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Mesonephric hyperplasia (MH) is a very rare condition. There are few cases in the literature. Mesonephric remnants (MR) or MH can be a rare source of abnormal Papanicolaou smears. The most common, often difficult, in the differential diagnosis of MH is mesonephric carcinoma that has a poor prognosis.
We report a case of a 29-years-old with a routine Papanicolaou smear reported as atypical glandular cells. The patient underwent to a loop electrosurgical excision procedure and because it is a benign condition and a strong desire to preserve fertility, we opted for clinical surveillance.
Keywords: Hyperplasia; Mesonephric; Papanicolaou smears; Mesonephric carcinoma.
Introduction
Embryologically, mesonephric ducts (Wolffian duct) are intimately related to Mullerian ducts and normal formation of Mullerian duct is dependent on the presence of mesonephric ducts1. In female fetus, in the absence of anti-Mullerian hormone, mesonephric ducts regress, and the Mullerian structures persist and develop into fallopian tubes, uterus, cervix, and upper third of vagina1. Vestigial mesonephric ducts are embryological remnants which are seen predominantly in the paraovarian region (epoophoron and paroophoron) and deep in the cervical stroma in the lateral walls2. Remnants of these ducts may persist typically along the lateral walls of the cervix, vagina, adnexa and uterine corpus. These mesonephric epithelia may expand into hyperplasic proliferations and rarely turn into neoplasms3. In a study of cervical mesonephric rests and derived lesions, Ferry and Scully4 described four cervical mesonephric carcinomas (MCA) (three of them had been previously reported) and underlined the importance of distinguishing them from mesonephric hyperplasia (MH) and other cervical carcinomas of Müllerian nature, such as clear cell adenocarcinoma and adenoma malignum (minimal deviation adenocarcinoma)5.
Mesonephric remnants (MR) or MH are usually incidental findings, and the literature has focused on differentiating these lesions from other glandular lesions on histologic examination6. MR or MH are not generally recognized as a potential source of abnormal Papanicolaou (Pap) smears6. False positive rate for cervical-vaginal smears called highgrade epithelial lesion is approximately 10%7. In such cases, complete excision is required to exclude associated MCA and other conditions3. If coexisting carcinoma is not identified, the prognosis is excellent with no further treatment necessary3.
We present a case of MH with abnormal cells on screeening Papanicolaou smears with prior approval by Ethics Committee of Instituto Português de Ginecologia Francisco Gentil de Coimbra and with request of informed consent from the respective patient.
Case description
A 29-years-old, gravida 1 para 1, had a routine Papanicolaou smear with Atypical Glandular Cells, without excluded neoplasia. The Pap smear showed small clusters of glandular cells with nuclear hyperchromasia and cuboidal shape rather than tall columnar. The cytoplasm were varied from scant to abundant.
Prior medical and gynecological history was unremarkable. All previous Papanicolaou tests had been normal. Colposcopic examination revealed no changes. Human Papiloma Virus (HPV) teste was positive to 18 type. Endocervical curettage was normal.
Gynecological ultrasound and nuclear magnetic resonance revealed no abnormalities. The serum concentration of tumor markers was within normal range.
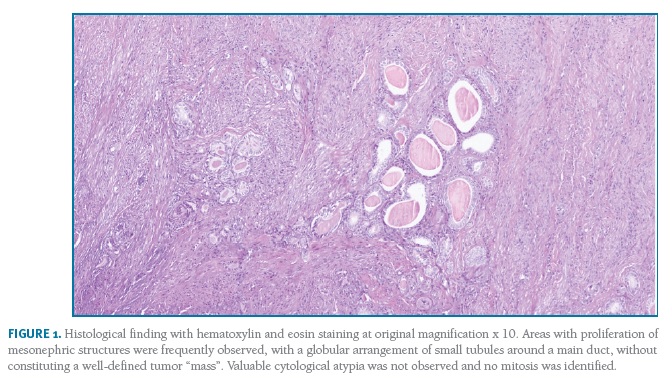
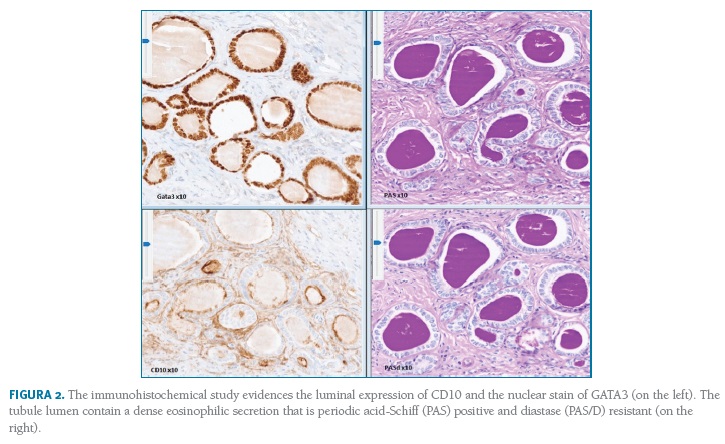
The patient underwent to a loop electrosurgical excision procedure with a piece with 33x12mm of base and 22x11mm of height. Histology showed a cervical uterine lesion that was 5 mm from the endocervix margin and 10 mm from the exocervix margin. Areas with proliferation of mesonephric structures were also frequently observed, with a globular arrangement of small tubules around a main duct, without constituting a well-defined tumor “mass”. The tubule lumen contain a dense eosinophilic secretion periodic acid-Schiff (PAS) positive (Figure 1 and 2). Valuable cytological atypia was not observed and no mitosis was identified. The proliferative index was less than 5%. The immunohistochemical study evidences apical and luminal expression of CD10 and the nuclear stain of GATA3. (Figure 2). These characteristics and the remaining evaluation were compatible with the final diagnosis of MH.
(clique para ampliar ! click to enlarge)
(clique para ampliar ! click to enlarge)
Because it is a benign condition and a strong desire to preserve fertility, we opted for clinical surveillance with cervical cytology and colposcopy every 6 months.
After 2 year of surveillance, the patient remains asymptomatic, without cervical lesions and maintains her reproductive status.
Discussion
MH, much like MR, is usually encountered as an incidental finding and may be associated with abnormal Papanicolaou smear. However, rarely may form a clinically evident mass.9 Mesonephric adenocarcinoma is believed to arise from benign MR or MH located in the lateral walls of the uterine cervix.1 They are uncommon in other sites of the gynecologic tract, and exceptionally rare in the uterine corpus1. So far, only 30 cases of uterine mesonephric adenocarcinoma have been reported in the literature, as a result, the etiology, clinical behavior, choice of treatment, and histogenesis are still unclear1.
MH presence has been described in women ranging from 21 to 81 years4,9. Generally asymptomatic, they have been implicated in vaginal or postcoital bleeding on rare occasions9. Looking at cases of MH reported in the literature, an abnormal cervical smear has been noted in about 40% of the cases and histologically proven coexistent squamous cervical CIN or endocervical adenocarcinoma has been found in up to 35% of the cases10. Ferry and Scully9 studied 45 cases with MR and MH, 22 of which were referred for abnormal cervical smears or dysplasia. Cytological descriptions of cells noted in mesonephric hyperplasia have not been described in any detail6. Among the cases describe in literature6,9,10 the cytologic features of the mesonephric cells varied. Abnormal cells tend to cluster but not so tight as those characteristically seen in endometrial cells6. They are mostly cuboidal with nuclear hyperchromasia6,9,10. The cytoplasm varies from scant to abundant in amount and basophilic to orangeophilic in color6. The differential diagnosis of adenocarcinoma in situ on Pap smears includes benign glandular conditions6. In histologic specimens, MR and MH, which has an infiltrative pattern, are sometimes confused with cervical adenocarcinoma.6 Various nonendocervical glandular lesions enter the histologic differential diagnosis of MR including endometriosis and entrapped fallopian tube epithelium in posthysterectomy patients6. The lack of cilia, a retiform or lobular arrangement of rounded tubules, and densely eosinophilic luminal secretions support a mesonephric origin6. In this case we report a patient with 29-years-old, asymptomatic and referred to our appointment with a Papanicolaou smear reported as atypical glandular cells. The abnormal cells tended to cluster, with mostly cuboidal shape and nuclear hyperchromasia. Dense groups, cilia, pseudostratification and feathering were not seen.
Histologically, MH is usually located deep in the cervical stroma but occasionally are identified immediately subjacent to endocervical or squamous mucosa3. It’s composed by clusters or linear arrays of small to medium-sized tubules lined by bland cuboidal cells with scant cytoplasm lacking ciliation, mucin, or squamous differentiation3. The tubule lumens often contain a densely eosinophilic secretion that is periodic acid-Schiff (PAS) positive9. The nuclei in MH remnants are uniform3. Variations of MH include lobular, diffuse hyperplasia and ductal type. The histological features of MH are similar to MR, but tubules and/or ducts are present in greater abundance and are typically larger than 6 mm3. Immunohistochemically, mesonephric derived epithelia have a unique staining pattern allowing distinction from endocervical to endometrial epithelium3. CD10 typically highlights the apical (luminal) aspect of the cells and GATA3 and PAX8 are also frequently positive11,12,17. Both p16 and p53 are negative or weak patchy in benign MR13. In present case, hystology showed areas with proliferation of mesonephric structures, with globular arrangement of small tubules around a main duct, without constituting a well-defined tumor “mass”. The tubule lumen contain a dense eosinophilic secretion that is periodic acid-Schiff (PAS) positive as described in literature. Cytological atypia was not observed and no mitosis was identified. The proliferative index was less than 5%. These features suggested a benign condition. The avaliation was complemented with immunohistochemical study. It showed CD10 with typical apical and luminal expression and nuclear stain of GATA3. P16 was negative. These characteristics and the remaining evaluation were compatible with the final diagnosis of MH.
The most common, often difficult, in the differential diagnosis of MH is MCA. MCA affects patients of all age groups, ranging from 24 to 81-years-old1. Clinical course is characterized by multiple recurrences, pelvic metastases, and bad long-term survival14. Etiology and precursor lesions remain unclear and optimal regimen and efficacy of the treatment are largely unknown14. In general, MCA presents as a clinically evident mass; however, as mentioned previously, MH may also rarely present as a mass3. Additionally, some MCA may be discovered incidentally, or occur as small foci within MH3. For this reason, complete sampling of MH is important to exclude MCA. A diagnosis of MCA should be considered when confluent growth is present; i.e., tubules are ‘back to back’ with little to no intervening stroma3. Other morphological findings worrisome for carcinoma include complex architecture, solid or spindled growth, more than mild cytological atypia, and conspicuous mitoses3. Another important consideration is endometrial adenocarcinoma with invasion of the cervical stroma, which tends to demonstrate more haphazard growth, but can be quite bland with little or no stromal reaction15,16. Evidence of mucinous or squamous differentiation is also helpful to confirm the diagnosis of endometrioid adenocarcinoma3.
Conclusion
MR and MH are a rare and benign condition. These conditions can be a source of abnormal cervical cytology. Hystology in surgical specimen is fundamental for the exclusion of an equally rare, but more serious, with poor prognosis, such as MCA.
REFERENCES
1. Zhang L, Cai Z, Ambelil M, Conyers J, Zhu H. Mesonephric Adenocarcinoma of the Uterine Corpus: Report of 2 cases and review of the literature. Int J Gynecol Pathol. 2018; 38(3): 224-229. [ Links ]
2. McFarland M, Quick CM, McCluggage WG. Hormone receptor-negative, thyroid transcription factor 1-positive uterine and ovarian adenocarcinomas: report of a series of mesonephric-like adenocarcinomas. Histopathology. 2016; 68: 1013-1020. [ Links ]
3. Howitt BE, Nucci MR. Mesonephric Proliferations of the Female Genital Tract. Pathology. 2018; 50(2): 141-150. [ Links ]
4. Ferry JA, Scully RE. Mesonephric remnants, hyperplasia, and neoplasia in the uterine cervix: a study of 49 cases. Am J Surg Pathol. 1990; 14: 1100-1111. [ Links ]
5. Bagué S, Rodríguez IM, Prat J. Malignant mesonephric tumors of female genital tract: a clinicopathologic study of 9 cases. Am J Surg Pathol. 2004; 28(5): 601-607. [ Links ]
6. Welsh T, Fu YS, Chan J, Brundage HA, Rutgers JL. Mesonephric remnants or hyperplasia can cause abnormal pap smears: a study of three cases. Int J Gynecol. 2003; 22(2): 121-126. [ Links ]
7. DeMay RM. The Art and Science of Cytopathology. 2nd edition. Chicago: ASCP Press, 1996:138-143. [ Links ]
8. Bibbo M. Comprehensive Cytopathology. Philadelphia: W.B. Saunders Co., 1991:199. [ Links ]
9. Jones MA, Andrews J, Tarraza HM. Mesonephric remnant hyperplasia of the cervix: a clinicopathologic analysis of 14 cases. Gynaecol Oncol. 1993; 49:41-47. [ Links ]
10. Hejmadi RK, Gearty JC, Wadell C, Ganesan R. Mesonephric hyperplasia can cause abnormal cervical smears: report of three cases with review of literature. Cytopathology. 2005; 16:240-243. [ Links ]
11. Ordi J, Nogales FF, Palacin A, et al. Mesonephric adenocarcinoma of the uterine corpus: CD10 expression as evidence of mesonephric differentiation. Am J Surg Pathol. 2001; 25:1540-1545. [ Links ]
12. McCluggage WG, Oliva E, Herrington CS, et al. CD10 and calretinin staining of endocervical glandular lesions, endocervical stroma and endometrioid adenocarcinomas of the uterine corpus: CD10 positivity is characteristic of, but not specific for, mesonephric lesions and is not specific for endometrial stroma. Histopathology.2003; 43:144-150. [ Links ]
13. Cina SJ, Richardson MS, Austin RM, et al. Immunohistochemical staining for Ki-67 antigen, carcinoembryonic antigen, and p53 in the differential diagnosis of glandular lesions of the cervix. Mod Pathol. 1997; 10:176-180. [ Links ]
14. Dierickx A, Göker M, Braems G, et al. Mesonephric adenocarcinoma of the cervix: case report and literature review. Gynecol Oncol Rep. 2016; 17:7-11. [ Links ]
15. Tambouret R, Clement PB, Young RH. Endometrial endometrioid adenocarcinoma with a deceptive pattern of spread to the uterine cervix: a manifestation of stage IIb endometrial carcinoma liable to be misinterpreted as an independent carcinoma or a benign lesion. Am J Surg Pathol. 2003; 27:1080-1088. [ Links ]
16. Kalyanasundaram K, Ganesan R, Perunovic B, et al. Diffusely infiltrating endometrial carcinomas with no stromal response: report of a series, including cases with cervical and ovarian involvement and emphasis on the potential for misdiagnosis. Int J Surg Pathol. 2010; 18:138-143. [ Links ]
17. Goyal A, Masand RP, Roma AA. Value of PAX-8 and SF-1 immunohistochemistry in the distinction between female adnexal tumor of probable Wolffian origin and its mimics. Int J Gynecol Pathol. 2016; 35:167-175. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Sofia Sousa Pedrosa
Centro Hospitalar do Baixo Vouga EPE
Aveiro, Portugal
E-Mail: sofias_pedrosa@hotmail.com
Recebido em: 23/02/2020. Aceite para publicação: 20/04/2020














