Introduction
The tongue is an organ that performs important functions for the human body. It is responsible for tasting, swallowing, and phonation and acts directly on the development of the facial skeleton, occlusion, and anteroposterior growth of the alveolar process.1
Macroglossia is an anatomical abnormality of multiple etiology related to an unusually large volume of the tongue, which can cause dento-musculoskeletal deformities and instability of orthodontic-surgical treatment, besides favoring the appearance of chewing, speech, and breathing disorders.2,3
The most common causes of macroglossia are idiopathic muscle hypertrophy, lymphatic or venous malformation, neurofibromatosis, congenital hypothyroidism, Beckwith-Wiedemann syndrome, and chromosomal changes such as Down syndrome.1,4
Classification of macroglossia is not consensual in the literature. Wolford et al.2 classify it as real when there is excessive growth of the organ and relative (pseudo-macroglossia) when the oral cavity space is insufficient for its accommodation.
Due to the lack of an effective method for sizing the tongue, the diagnosis of macroglossia is generally based on subjective criteria.5 Observation of signs and symptoms such as morphology and lingual protrusion, dyslalia, dento-skeletal and/or respiratory changes, anterior open bite,2,6,7difficulty swallowing, and bite marks on the lingual margins help the diagnosis.1,5,6Beyond these clinical findings, cephalometric aspects such as dentoalveolar protrusion, excessive angulation of anterior teeth, increased goniac angle, and inclination of mandibular and occlusal planes can also be observed.2,6
The appropriate treatment for macroglossia is not yet clear, especially for the relative type. Although orthognathic surgery alone can enlarge the space of the oral cavity, the consequente space gain may be insufficient to adequately accommodate the tongue in some cases of macroglossia. Therefore, it is consensual that the indication of glossectomy for treating macroglossia is based on the clinical criteria already mentioned,2,5-7 especially respiratory and functional changes.7 Surgical tongue reduction in these cases improves aesthetics and function, in addition to facilitating the correction of associated dento-skeletal changes.3,4
This study reports a case of relative macroglossia and dentofacial deformity with obstructive sleep apnea syndrome (OSAS) whose treatment was partial glossectomy, using the technique described by Egyedi-Obwegeser,8 concomitant to orthognathic surgery.
Case report
A 48-year-old Caucasian female patient attended the Service of Oral and Maxillofacial Surgery at the Clinical Hospital of the Federal University of Uberlândia (HC-UFU) to assess the need for orthognathic surgery. During anamnesis, the patient reported functional and aesthetic complaints related to breathing difficulty and discomfort with tongue dimensions, which made teeth fitting impossible. Also, she had a medical diagnosis of OSAS. Clinical and radiographic examination (Figure 1) revealed a skeleton deformity (maxillary deficiency/ atresia) with narrowing of the upper airways, chronic interposition of the tongue between resting dental arches, mild lingual fibrosis, and lateral grooves resulting from recurrent chewing trauma, besides malocclusion with anterior open bite and superior interincisal diastema. The association of signs and symptoms led to the diagnosis of relative macroglossia.

Figure 1 Pre-orthodontic images: (A) Frontal aspect, (B) Facial profile, and (C) Smile showing the anteroposterior deficiency of the maxilla; (D-F) Intrabuccal aspect showing class III malocclusion, anterior open bite, and superior interincisal diastema; (G) Panoramic radiographs; (H) lateral teleradiograph showing skeletal deformity and anteroposterior narrowing of the upper airway
The treatment plan included orthognathic surgery concomitant with partial glossectomy. Orthodontic preparation was performed to enable facial deformity correction by orthognathic surgery. A new, trans-surgical evaluation of the macroglossia was scheduled for the moment after bone repositioning. The surgical technique included advancement and Y-maxillary segmentation for anteroposterior and transversal maxilla correction, in addition to advancement genioplasty using the basilar horizontal osteotomy technique. After osteotomy fixation and release of the maxillomandibular block, difficulty in accommodating the tongue within the oral cavity was confirmed even with the gain of space provided by orthognathic surgery. Thus, a partial glossectomy was performed with an incision in the midline, according to the technique described by Egyedi-Obwegeser,8 and suture in planes with absorbable thread (Figure 2). No complications were observed during the postoperative period.
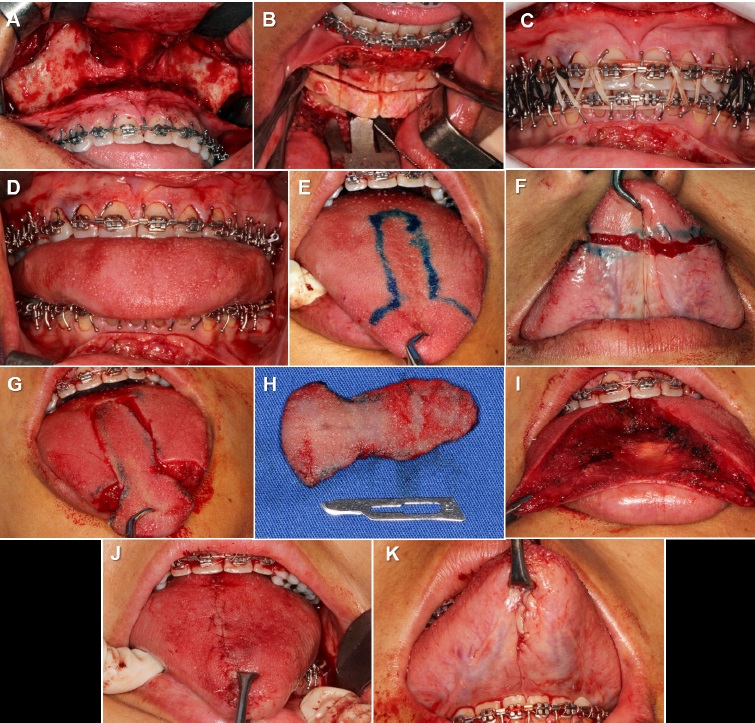
Figure 2 Surgical procedure: (A) Maxillary exposure; (B) Advance genioplasty; (C) Transoperative final occlusion; (D) Trans-surgical reevaluation of macroglossia after maxillomandibular block release; (E) Incision demarcation; (F) Incision of the apex and lingual belly; (G) Incision of the dorsum and lingual apex; (H) Excised portion of the tongue; (I) Lingual aspect after excision; (J) Final aspect of the lingual dorsum; (K) Final aspect of the lingual belly
The patient was referred to speech therapy. At the 3-month postoperative follow-up, adequate lingual positioning and satisfactory occlusion were observed (Figure 3). After this period, the patient had persistent difficulty with the phonation of the letter “R”. Therefore, lingual frenectomy was performed after 6 months of follow-up to further facilitate tongue movement and phonation. After a 16-month follow-up, the patient presented facial harmony, occlusal stability, preserved lingual and phonetic function, mild paresthesia, and dysgeusia only at the lingual apex. There was also an increase in the space of the upper airways (Figure 4). Furthermore, the OSAS complaints were resolved, and the masticatory function and facial aesthetics improved.
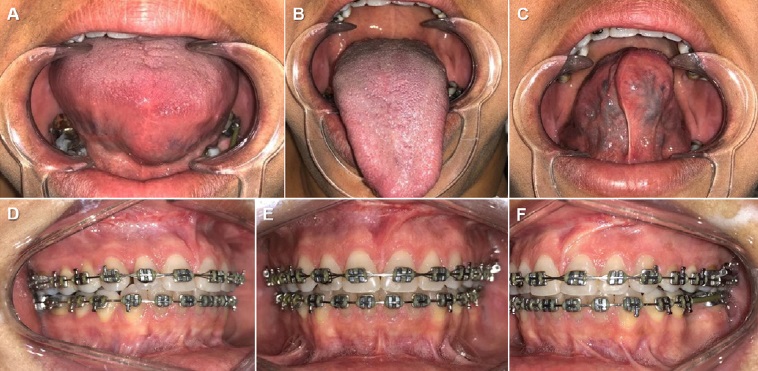
Figure 3 Three-month follow-up: (A) Lingual aspect at rest; (B) Protruding lingual aspect; (C) Aspect of the lingual belly; (D) Right side occlusion; (E) Frontal occlusion; (F) Left side occlusion
Discussion and conclusions
Macroglossia is an uncommon condition in adults, and early intervention in childhood through partial glossectomy combined with orthodontic treatment can act as a preventive measure to avoid tongue influence on the development of dental malocclusions.4 Correct diagnosis is challenging for surgeons due to the lack of well-established criteria and direct measurement techniques that point to normality or pathological increase of the organ.5
Several authors have pointed out clinical and cephalometric characteristics as signs and symptoms of macroglossia.
However, these data are subjective, creating difficulties in treatment indication.2,5,7 Therefore, the indication of partial glossectomy as a form of treatment for macroglossia (true or relative) is controversial. Even so, it is consensual that the decision to treat the patient with macroglossia using the partial glossectomy technique should be based on lingual mobility, position, and function, reported symptoms, respiratory changes, speech intelligibility, presence of skeletal anterior open bite, interference on the stability of orthodontic or ortho-surgical treatment, problems with swallowing, and recurrent tongue trauma.2,5,6,7
Surgical treatment of macroglossia aims to reduce tongue dimensions through partial excision of the organ. Several partial glossectomy techniques have been described to preserve lingual sensory capacity and mobility.1,5The main complications associated with partial tongue excision are excessive bleeding, airway obstruction due to edema, dysgeusia, hypomotility, dehiscence, dyslalia, and parestesia of the tongue apex.7,8The technique advocated by Egyedi-Obwegeser8 - “keyhole” - has been used more than the other techniques due to the satisfactory results in reducing the total volume of the tongue. This technique recommends incisions in the anterior and median region of the tongue, allowing a reduction in tongue length and width2,4,8and preserving the neurovascular bundle since the lingual artery and the lingual and hypoglossal nerves have a lateral path.7
It is also worth highlighting that this technique preserves the circumvallated and fungiform papillae, maintaining taste functions.7
Wolford & Cottrell2 described three treatment options for macroglossia diagnosis in patients with facial deformity: (A) Phase 1: orthognathic surgery, Phase 2: partial glossectomy; (B) Phase 1: partial glossectomy, Phase 2: orthognathic surgery; and (C) perform orthognathic surgery and partial glossectomy at the same surgical time. In treatment option A, ortho-surgical treatment can be initially indicated alone in phase 1, and then, in case of occlusal instability and recurrence, partial glossectomy must be performed in phase 2. Treatment option B offers some advantages, such as less concern with the airways and absence of intermaxillary fixation, as glossectomy and orthognathic surgery would not be simultaneous. In addition, the pre-surgical orthodontic preparation is more predictable due to greater tongue stability in the oral cavity after glossectomy in phase 1.2
Some authors favor orthognathic surgery and glossectomy in a single step (treatment option C) because the absence of postoperative intermaxillary fixation makes airway management more accessible.2,3,6Simultaneous surgery has the benefits of reducing the amount of general anesthesia and the possibility of post-surgical recurrence.3,6 However, some cases in the literature have reported opting for the two surgical stages due to concerns about airway obstruction secondary to tongue edema and postoperative bleeding;3,7 those complications were not observed in the present report.
Macroglossia is an unusual anatomical alteration that can lead to dysphagia and OSAS because tongue movement plays a critical role in speech, swallowing, and breathing.2,3Currently, there is insufficient evidence to indicate glossectomy as an isolated procedure specifically for treating OSAS9 because patients with sleep apnea often have a profile II pattern with less airway volume. However, there are interesting results from treating sleep apnea by orthognathic surgery associated with partial glossectomy in adult patients.2,9 In these situations, maxillomandibular advancement and lingual volume reduction effectively treat respiratory disorders. In the present case, treatment with orthognathic surgery and advancement genioplasty associated with partial glossectomy increased airway space, as seen in the postoperative lateral teleradiograph.
The individual’s ability to produce and use articulatory patterns for communication is related to satisfactory occlusion and muscular mobility of the tongue. In this sense, partial glossectomy could result in posture and lingual function changes.
However, this has not been confirmed in the literature. A recently published systematic review on the subject found no significant differences in the medium term regarding the adaptation of dentofacial structures and language function after glossectomy.10 Still, supporting speech therapy is essential after orthognathic surgery and glossectomy.11 It aims to help reestablish normal tongue mobility and word articulation, effectively improving speech intelligibility in the postoperative period.
When properly indicated and performed, partial glossectomy allows the correction of lingual morphology, preserving its functions. Orthognathic surgery and partial glossectomy using the Egyedi-Obwegeser technique, at the same surgical moment, is a satisfactory approach to correct functional and aesthetic changes, improving the quality of life of patients with dentofacial deformity, OSAS, and relative macroglossia.
















