Introduction
The orbit is a support structure of soft tissues in this region of the face and consists of lacrimal, sphenoid, ethmoid, zygomatic, maxillary, palatine, and frontal bones.1 In the medial-anterior wall of the orbit, the lacrimal bone delimits the lacrimal fossa. The upper part of this fossa lodges the lacrimal sac, and the lower part, the nasolacrimal duct. The nasolacrimal ducts have 12 to 18 mm of extension and are responsible for draining tears to the inferior nasal meatus.2
Treating traumatic injuries involving fractures of the maxillofacial and orbital regions is already a recurrent practice for oral and maxillofacial surgeons. Most patients with these lesions have epiphora, recurrent episodes of conjunctivitis, and mucoceles due to lacrimal sac and/or nasolacrimal duct involvement.3 Furthermore, besides trauma, reconstructive surgeries in this region may cause considerable damage to the lacrimal system.4
Dacryocystitis is an infection of the lacrimal sac, usually caused by blockage of the duct that carries tears from the lacrimal sac to the nose. This blockage can occur secondary to a tear duct malformation, injury, eye infection, or trauma.5 Few studies4-6have described dacryocystitis caused by mechanical obstruction of the nasolacrimal duct by a foreign body. However, there are no reports of obstruction in individuals submitted to osteosynthesis with plates and screws for the treatment of zygomatic-orbital complex fractures. The fixation methods used for fractures of the middle third of the face are diverse and depend on the complexity of the fractured segments.5 Therefore, dacryocystitis is a possible postoperative complication due to the nasolacrimal duct’s proximity to the fracture site, especially in Le Fort I cases. The nasolacrimal duct may be damaged during superior repositioning by Le Fort I osteotomy and inferior turbinectomy. The damage to the nasolacrimal duct occasionally causes permanent obstruction or recurrent dacryocystitis.7,8
Previous studies have shown that vertical and sagittal skeletal patterns directly influence the anatomy of bone structures.
However, to the best of our knowledge, no study has evaluated the relationship of these skeletal patterns with the lacrimal duct anatomy. The aim of this study was to evaluate the dimensions of the nasolacrimal duct and the thickness of the adjacent maxillary bone by multislice computed tomography (MSCT) in individuals with different skeletal patterns and analyze which groups of individuals would have a greater predisposition to injuries during the fixation of infraorbital fractures.
Material and Methods
This research was approved by the local Ethics Committee. MSCT images of 92 individuals (184 sides), taken for orthognathic surgery planning, were obtained from an image bank and studied. In this sample, 55 (59.78%) were females and 37 (40.22%) were males. The mean age was 32 years. The images were acquired with a 64-channel multislice tomograph (Light Speed VCT, GE Healthcare Bio-Sciences, Piscataway, NJ, USA) using the following acquisition protocol: 120 kV, 200 mA, voxel 0.6 mm, and field of view (FOV) of 32 cm (full face).
The inclusion criteria were MSCT images with a full-face FOV of patients older than 18 years. Tomographies showing signs suggestive of facial trauma or fracture, severe facial asymmetries, and patients with a history of facial surgery, suggestive signs of maxillary tumors, syndromes, and cleft lip/ palate were excluded. The images were analyzed by a properly calibrated observer on a 27-inch iMac, 2560 x 1440 (Apple, Inc., Cupertino, CA, USA) using the Osirix v.3.9.3 software (Pixemeo, Geneva, Switzerland).
First, the images were adjusted to ensure a parallel Frankfort horizontal plane in order to obtain a standardized head position. The frontozygomatic sutures were used as a reference for the frontal view, and the orbital inferior margin and Porion landmark for the lateral view. The orbital floors were then aligned. The measurements were made from the location of the lacrimomaxillary suture, which was used as the reference for the midpoint measured when the axial section image showed the suture in linear format. The thickness of the maxillary bone adjacent to the nasolacrimal duct and the largest diameters of the nasolacrimal duct were then measured at this point and 2 mm above and below it. The lateromedial and anteroposterior diameters of the nasolacrimal duct were also measured (Figure 1). For intraobserver reproducibility, 25% of the sample was re-evaluated after 30 days.

Figure 1 Axial slice showing the lacrimomaxillary suture (white arrow) and the measurements of the nasolacrimal duct diameters (white line), as well as the thickness of the maxillary bone (black line)
The sagittal skeletal pattern was determined in the tomographic images according to the classification of Steiner9 based on the ANB angle (angle formed by the A point, nasion, and B point), which defines the sagittal relationship of the jaws. The ANB angle was measured to classify the sagittal skeletal pattern as Class I (0° to 4.5°), Class II (> 4.5°), and Class III (< 0°). Twenty-eight (30.4%) individuals were classified as Class I, 45 (48.9%) as Class II, and 19 (20.7%) as Class III. The vertical skeletal pattern was established according to the classification of Riedel,10 and divided based on the SN.GoGn angle into mesocephalic (27° to 37°), brachycephalic (< 27°), and dolichocephalic (> 37°). Forty-one (44.6%) individuals were classified as mesocephalic,17 (18.5%) as brachycephalic, and 34 (36.9%) as dolichocephalic.
Data were analyzed using the Minitab® software release 14.20 (State College, PA, USA). The intraclass correlation coeficiente (ICC) was applied to evaluate intraobserver reproducibility according to the Koo and Li criteria:11poor reliability at <0.5, moderate reliability between 0.5 and 0.75, good reliability between 0.75 and 0.9, and excellent reliability at >0.90. The maxillary bone and nasolacrimal duct measurements were analyzed by one-way ANOVA with Tukey’s post-hoc test. The significance level was set at 5%.
Results
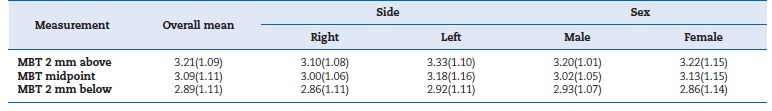
The ICC values for all measurements showed good intraobserver reproducibility (0.84-0.89). Table 1 summarizes maxillary bone thickness measurements according to side and sex.
The maxillary bone thickness was highest at 2 mm above the midpoint (3.21 mm). No statistically significant diferences were observed between sides or sexes (p>0.05).
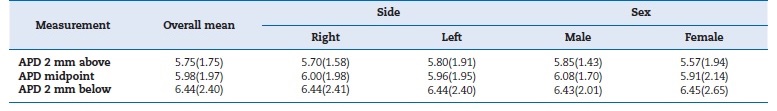
The anteroposterior and mediolateral diameters of the nasolacrimal duct were highest at 2 mm below the midpoint (6.44 mm and 4.14 mm, respectively). There were no significant diferences between sides or sexes (p>0.05) (Tables 2 and 3). Females had a narrower duct, with a significant difference at the midpoint (p=0.026) and 2 mm above it (p=0.025) (Table 3).
Table 3 Mean (standard deviation) lateromedial diameter (LMD) of the nasolacrimal duct.
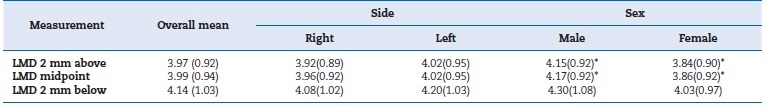
*Significant difference (p<0.05)
Analysis of the sagittal skeletal pattern (Table 4) showed greater maxillary bone thickness in Class II individuals compared to Class I individuals, with a significant difference at the midpoint (p=0.027) and 2 mm above it (p=0.012). There were no significant differences when Class III individuals were compared to Class I and II (p>0.05). No significant differences were observed in the anteroposterior diameter of the nasolacrimal duct between the different sagittal skeletal patterns (p>0.05), which was slightly higher in Class III individuals. The lateromedial diameter of the duct 2 mm below the midpoint was significantly lower in Class I compared to Class III individuals (p=0.019) (Table 4).
Regarding the different vertical skeletal patterns (Table 5), dolichocephalic individuals had greater maxillary bone thickness at the midpoint (p=0.014) and 2 mm below it (p=0.005) compared to brachycephalic individuals. In addition, the maxillary bone thickness was greater at 2 mm below the midpoint in the mesocephalic group compared to dolichocephalic individuals (p=0.04). In addition, the anteroposterior and mediolateral diameters of the nasolacrimal duct were similar in the different skeletal patterns and regions and highest in dolichocephalic individuals. However, no significant differences were found (p<0.05).
Table 4 Mean (standard deviation) maxillary boné thickness (MBT), anteroposterior diameter (APD), and lateromedial (LMD) diameter of the nasolacrimal duct in different sagittal skeletal patterns.
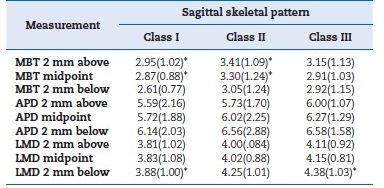
*Significant difference (p<0.05)
Discussion
The nasolacrimal region is frequently ignored or unobserved in clinical management and should be evaluated pre-surgically.
Previous studies have shown that vertical and sagittal skeletal patterns directly influence the anatomy of bone structures such as the pterygomaxillary region,12 mandibular symphysis,13 cortical and alveolar bone,14,15and calvarial structure.16 Based on the tomographic measurements, our study showed that the different skeletal patterns may have an influence on the anatomic measurements of the nasolacrimal duct as well as on the thickness of the adjacent maxillary bone, which is important during Le Fort osteotomies or in cases of naso-ortho-ethmoid fractures.5,6,17
This retrospective study used a convenience sample to investigate differences in bone availability at the nasolacrimal region among skeletal patterns. A large FOV was necessary and justified for orthodontic/surgical planning. Cone-beam computed tomography (CBCT) emits a lower radiation dose than MSCT.18 However, orthognathic patients with jaw deformities are traditionally referred to radiology departments for na MDCT skull scan for treatment planning. This preoperative scan enables surgeons to carry out facial measurements to evaluate the deformity and guides the design and fabrication of the surgical splints that will be used during surgery.19 In addition, according to Gaia et al.,20 linear measurements obtained from MSCT (0.6-mm resolution) and CBCT (0.25-mm resolution) images were considered precise and accurate. Furthermore, a common critique of CBCT is that it cannot accurately measure soft tissue. With regard to orthognathic surgery, soft-tissue measurements and predictions are essential for preoperative analysis and treatment planning.21
The nasolacrimal duct plays a key role in the continuous drainage of lacrimal secretions; however, facial fractures or surgical reconstructions may impede this drainage. Some studies showed that 5 to 21% of open reconstructions of naso-ortho-ethmoid fractures result in lacrimal duct obstruction,8 requiring reconstructive surgeries of the lacrimal system.
Therefore, this study evaluated the thickness of the maxillary bone adjacent to the nasolacrimal duct and nasolacrimal duct diameters to provide greater safety in reconstructive surgical procedures after facial fractures. Our findings suggest that brachycephalic and Class I individuals are more likely to develop postoperative complications such as dacryocystitis by mechanical obstruction of the lacrimal duct.
The tomographic images were analyzed in the three planes, and axial slices provided the most accurate measures of the diameter of the nasolacrimal duct.22,23 The findings regarding the anatomy of the nasolacrimal duct between males and females are still conflicting. Some studies24-26 reported a greater lacrimal duct length and diameter in males than females, while others23,27,28 found no significant differences between sexes. In our study, only the lateromedial diameter of the nasolacrimal duct at the midpoint and 2 mm above it was significantly higher in males than females.
Individuals with fractures of the naso-orbito-ethmoidal complex are more likely to develop dacryocystitis or epífora as postoperative complications.28,29 According to Garg et al.,30 the risk of developing obstructive symptoms in the lacrimal system after fractures of the naso-orbito-ethmoidal complex is approximately 10%. In addition, the authors identified five different fracture patterns that increase the risk of developing obstruction of the lacrimal system. The presence of bone fragments in the lacrimal duct or lacrimal sac, lacrimal crest avulsion, severe duct compression, and displacement of the nasomaxillary pillar were significantly associated with the development of dacryocystitis and/or epiphora.30
Our study showed that the maxillary bone is thinner at 2 mm above the midpoint, suggesting a higher risk of obstruction of the nasolacrimal duct during the fixation of orbital bone fractures due to the proximity of this duct to the screws.
This higher risk of duct obstruction should be considered because the maxillary bone is less thick the farther it is from the orbit.
There are several types and shapes of osteosynthesis materials, including plates and screws. Variable screw sizes are available, which are chosen according to the thickness of the cortical bone to be fixed. The 4-mm long screw is the smallest of bone fixation systems. Regardless of the individual skeletal pattern, in this study, the maxillary bone thickness was less than 4 mm, indicating that the osteosynthesis screws are longer than the thickness of the maxillary bone. Therefore, obstruction (total or partial) of the lumen of the nasolacrimal duct may occur. Small differences in the diameter of the bony nasolacrimal canal may cause obstruction by influencing tear flow.23,26 During surgical planning, preoperative anatomical analysis of the nasolacrimal system is necessary to allow modifying the plate position and screw dimension according to its anatomy, thus avoiding the aforementioned complications.
Regarding the vertical skeletal pattern, brachycephalic individuals have a lower maxillary bone thickness at the lowest point compared to dolicho- and mesocephalic individuals. This characteristic may be associated with an increased risk of postoperative complications, such as maxillary sinus invasion and sinusitis, in these patients. In orthognathic surgery, brachycephalic patients have the smallest maxillary bone;31 thus, surgeons must be aware of the position of the fixation material in order to prevent possible dacryocystitis.
The nasolacrimal duct had greater anteroposterior and lateromedial diameters as it approached the inferior nasal meatus.
This widening of the nasolacrimal duct was also seen in individuals with different sagittal skeletal patterns. Class II and III individuals had a larger nasolacrimal duct than Class I. Individuals with different vertical patterns showed a narrow nasolacrimal duct in the anteroposterior diameter, especially at 2 mm above the midpoint. The lateromedial diameter was only lower in mesocephalic individuals, while brachycephalic and dolichocephalic individuals had similar values at the midpoint and 2 mm above it.
Direct trauma to the nasolacrimal duct resulting from fractured bone segments or the presence of the fixation screw used for the management of naso-orbito-ethmoidal complex fractures can cause dacryocystitis. A change in the direction of screw insertion may minimize this risk, but clinical studies are needed. Virtual surgical planning has evolved substantially over the last decades. During Le Fort I osteotomy and repositioning of the maxillary complex, two types of injury may be inflicted on different anatomical regions of the nasolacrimal apparatus. Injury may be caused by instrumentation and a close approximation of screws to the nasolacrimal apparatus or direct transection of the canal via the osteotomy line.17
Therefore, we emphasize the need to verify the nasolacrimal canal anatomy. Cutting guides and customized titanium plates might help prevent injury to this structure.
The fact that this was a cross-sectional radiological study using a convenience CT sample is a limitation. In addition, we did not evaluate the anatomy of the nasolacrimal duct throughout its extension (only in the superior position - 2 mm above it and below the lacrimomaxillary suture). Lastly, we used an image database of patients who would undergo orthognathic surgery, limiting the sample size. Further studies using larger samples for each facial pattern are needed. Additionally, the nasolacrimal duct should be assessed in diferente regions. Clinical studies are needed to evaluate the association of dacryocystitis with the anatomy of the nasolacrimal region.
Conclusions
In conclusion, the results of our study showed similar anteroposterior and lateromedial dimensions of the nasolacrimal duct in individuals with different skeletal patterns. However, brachycephalic Class I individuals have lower maxillary boné thickness adjacent to the nasolacrimal duct, requiring caution during the fixation of infraorbital fractures.