Introduction
In the last decades, the risk of tooth loss among the elderly has increased, mainly due to worldwide demographic growth and higher average life expectancy.1-5Despite the development of fixed rehabilitations, removable dentures are still valid treatments for partial and total edentulism. Besides restoring the masticatory and phonetic functions and aesthetics,6 removable dentures are easy to produce and maintain and have adequate mechanical and biological properties.7,8
Due to its availability and cost, polymethylmethacrylate (PMMA) is the polymer resin most commonly used to produce removable denture bases through the conventional method.9,10
However, PMMA is affected by polymerization shrinkage and the oral biodegradation processes that allow bacterial colonization and release of residual monomers with allergic potential into the oral cavity. Thus, there is a need to develop new materials and techniques that facilitate and increase denture’s production quality.
In recent years, technological advances have allowed using digital methods, including computer-aided design (CAD) and computer-aided manufacturing (CAM), to produce denture bases.11,12The final product is achieved either through the additive method, which consists of three-dimensional (3D) printing, or the subtractive method, by milling a block of previously cured material.13 Both methods allow storing information in a digital reusable source and decrease waste from and time for production.14
The additive method is based on light-cured resins with lower allergenic potential than PMMA-based resins.14-16 However, scientific evidence regarding 3D printed resins’ physical and mechanical properties shows they are related to the incremental production mode, as the binding of constituents within each layer is stronger than the binding between layers.17-19This technique leads to lower core cohesion, which can promote the propagation of failures and fractures in the material.20,21
Stress resistance at the interface with prosthetic teeth or reline resins is a relevant property for denture base resins. The relining procedure usually aims to restore the adaptation of a denture to the reabsorbed supporting mucosa. It consists of filling the denture base internally with a new acrylic resin to promote its longevity and avoid producing a new denture.22-26 Reduced bond strength may result from poor mechanical properties and interface leakage, associated with crack formation, pigmentation, and penetration by oral fluids and microorganisms.27
Other factors contributing to bond failure between the two materials are chemical composition, the reline resin’s thickness, and the oral environment’s thermal and chemical stress.28 These oral biodegradation processes are based on changes in temperature, pH, and chemical substances in the surrounding environment that, due to the acrylic resin’s porous matrix structure, have the potential to change its physical and mechanical properties.14,29,30
The bond strength of CAD/CAM resins to reline resins still needs to be further investigated. Thus, the main objective of this study was to evaluate the bond strength of digitally and conventionally produced denture base acrylic resins to reline resins after being submitted to a physical-chemical aging process.
The following hypotheses were established: 1) There is no difference in bond strength between relined denture base resins after physical-chemical aging; 2) The reline resin does not affect the bond strength of each denture base resin after physical-chemical aging.
Material and methods
A power analysis based on a pilot study was performed to estimate the sample size (n=10) required to provide statistical significance (α=0.05) at 80% power and an effect size of 0.25.29
Three denture base resins were selected: two light-cured resins of different chemical compositions suitable for 3D printing - V-Print Dentbase (VOCO GmbH, Germany) and Denture 3D+ (NextDent BV, The Netherlands); and a heat-cured resin for conventional production - Probase Hot, (Ivoclar Vivadent AG, Liechtenstein), used as the control. The reline resins selected were two self-cured hard acrylic resins: Ufi Gel Hard C (VOCO GmbH, Germany), suitable for chairside relining, and Probase Cold (Ivoclar Vivadent AG, Liechtenstein), used for laboratory relining (Table 1).
Table 1 Characteristics of the material (composition, ratio, curing method, manufacturer, lot number, and expiration date)
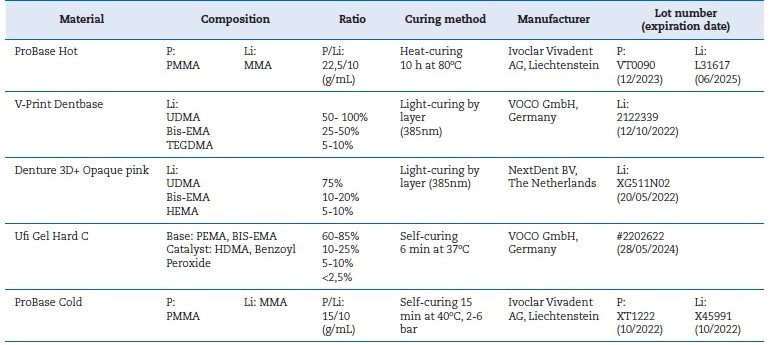
P - Powder; Li - Liquid; PMMA - polymethylmethacrylate; MMA - methyl methacrylate; UDMA - urethane dimethacrylate; bis-EMA - ethoxylated bisphenol-A dimethacrylate; TEGMA - triethylene glycol dimethacrylate; HEMA - hydroxyethyl methacrylate; PEMA - polyethylmethacrylate; HDMA - 1,6-hexanediol dimethacrylate
A total of 60 parallelepiped-shaped (10×10×3.3 mm) specimens of denture base acrylic resins (20 of each resin) were prepared. The printed specimens were designed with 3D Sprint CAD software (3D Systems, USA), producing a standard tessellation language (STL) file. Before printing, the NextDent Denture 3D+ liquid formulation was manually shaken for 5 min and further agitated for 1 h with the LC-3D Mixer machine (NextDent BV, 3D Systems, The Netherlands). The Denture 3D+ specimens were locally printed using 50-μm layers on a Next-Dent 5100 3D Printer (NextDent BV, 3D Systems, The Netherlands).
After production, the specimens were removed, submitted to an ultrasonic bath, and cleaned with isopropanol for 3 min and ethanol (>90%) for 2 min to remove excesses. Finally, the specimens were dried and placed in the LC-3DPrint Box (NextDent BV, 3D Systems, The Netherlands) for 30 min of additional photopolymerization.
The V-Print Dentbase denture base specimens were printed on a W2P Solflex 650 printer (W2P Engineering GmbH, Austria), by the manufacturer (VOCO Gmb, Germany), with a layer thickness of 50 μm. Specimens were cleaned with isopropanol (2+2 min), and the post-processing treatment was executed in the Otoflash G171 device (NK-Optik GmbH, Germany) with two cycles of 2000 flashes.
The heat-cured Probase Hot denture base acrylic resins were produced by a conventional flasking technique, according to the manufacturer’s instructions (Table 1).
To simulate three months of denture usage in the oral cavity, the specimens were subjected to 2500 cycles of termal fluctuations between 5ºC and 55ºC, with 20 s of dwell time, in a thermocycling machine (Refri 200-E, Aralab, Portugal). Then, they were ground with a P600 grain disc (Struers, Denmark) under constant cooling in a polishing machine (DAP-U, Struers, Denmark) to maximize the bond to the reline resin.
Each resin’s denture base specimens were then randomly divided into two groups of reline resins: Ufi Gel Hard C (VOCO GmbH, Germany) and Probase Cold (Ivoclar Vivadent AG, Liechtenstein).
A 5-mm diameter bonding area was defined by positioning a perforated adhesive tape (Glossy White Adhesive Film EA, Xerox) in the center of the specimen, impregnated with a specific adhesive in the case of Ufi Gel Hard C and with monomer liquid in the case of Probase Cold, as recommended by the manufacturers. Then, a silicon mold with a circular hole (5-mm internal diameter × 3-mm height) was placed on the adhesive tape and filled with acrylic reline resin (Figure 1). Each acrylic reline resin was mixed and applied according to the manufacturer’s instructions (Table 1). Direct relining materials were cured at 37ºC to simulate the oral cavity temperature. A pressure device (Ivomat, Ivoclar Vivadent, Liechtenstein) was used to maintain the indirect relining material under 40ºC and 2-4 bar for 15 min.

Figure 1 Relining procedure using a silicon mold with the 5x3-mm hole positioned above the bonding área of the denture base specimens, delimited by the white perforated adhesive tape
All the relined specimens were then submitted to a physical aging process through thermal fluctuations, followed by a chemical aging process through pH fluctuations. The physical aging process consisted of 1000 cycles of thermal fluctuations (corresponding to approximately one month in the oral cavity) by immerging the specimens for 20 s in 5ºC and 55ºC baths, with 5 s of dwell time, in a thermocycling machine (Refri 200-E, Aralab, Portugal). For the chemical aging process, the specimens were immersed in artificial saliva at 37ºC under constant 300-rpm agitation in the equipment (Memmert, Germany),25 where they were exposed to pH fluctuation cycles of 8 h at pH=3 and 16 h at pH=7 for 28 days; the samples were washed with distilled water and dried with absorbent paper between each cycle.
The relined specimens were then integrated into Watanabe plates with type IV plaster and tested to shear bond strength (SBS) in a universal testing machine (Instron model 4502, Instron Ltd, USA) using a cell load of 1 kN, at a speed of 1 mm/min, until the separation of the resins. The surfaces of the denture resins were examined using a stereomicroscope (EMZ-8TR, Meiji Techno Co, Japan), and two independent observers classified failure mode into three categories: adhesive, cohesive, or mixed.12
A descriptive analysis of the SBS and failure mode values was carried out. The Shapiro-Wilk test showed a normal distribution (p>0.05), but the Levene test did not prove the homogeneity of the variance (p=0.003). Thus, the Kruskal-Wallis non-parametric test was used. Parametric t-tests were used to compare the reline resins in each denture base resin since normality and homogeneity of variance in the sample distribution were verified for each denture base resin (p>0.05). The significance level was set at 5%.
Results
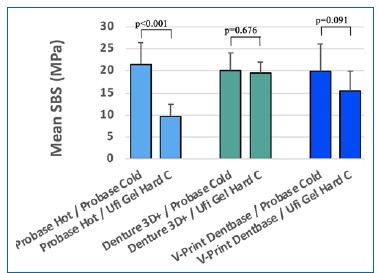
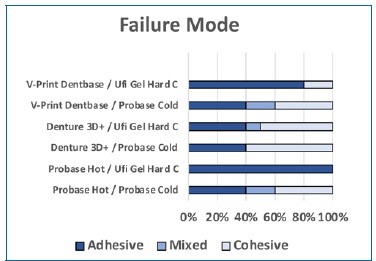
The SBS values were 8.9 ± 2.80 MPa for the combination Probase Hot + Ufi Gel Hard C and 21.5 ± 5.00 MPa for Probase Hot + Probase Cold. There were no statistically significant (p=0.07) differences in SBS between denture base resins (Figure 2). The individual denture base resin evaluation revealed no statistically significant differences in the printed specimens of Denture 3D+ (p=0.67) and V-Print Dentbase (p=0.90). Regarding Probase Hot specimens, the combination with Probase Cold obtained higher bond strength (p<0.001) (21.5 ± 5.0 MPa) than with Ufi Gel Hard C (8.9 ± 2.80 MPa) (Figure 3). Failure modes were predominantly adhesive in specimens of Probase Hot and V-Print Dentbase combined with Ufi Gel Hard C, while the Denture 3D+ specimens had mainly cohesive failures (Figure 4).
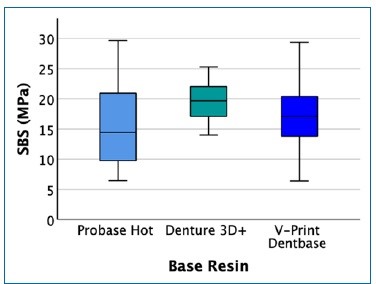
Figure 2. Box plots of shear bond strength (MPa) for denture base acrylic resins (n=8). Differences between resins were not statistically significant (p>0.05)
Discussion
The present in vitro study aimed to compare the bond strength of two printed denture base resins (Denture 3D+ and V-Print Dentbase) and one conventionally produced resin (Probase Hot) to two reline resins (Probase Cold and Ufi Gel Hard C) after being submitted to aging processes. No differences in bond strength were found between the three denture base resins and between the reline resins in each printed resin.
However, Probase Hot relined with Probase Cold resulted in higher SBS values than when relined with Ufi Gel Hard C. Most studies evaluating acrylic resins’ properties are conducted under controlled laboratory conditions without simulating the oral cavity environment.20-22 Nevertheless, oral biomaterials are commonly exposed to temperature changes (from daily exposure to food and drinks consumed at diferente temperatures) and pH fluctuations (from saliva componentes and food and drink ingestion) that can affect their physical and biomechanical properties.24,25,31Temperature variations may exceed the thermal expansion coefficient, originating mechanical tensions that can reduce core mechanical properties and adhesion to other materials.32 Accordingly, the presente study simulated one month of oral biodegradation using two aging procedures before testing: physical aging based on 1000 cycles of thermal variations and chemical aging based on 28 days of cycles of pH variations.24,25,31
Dentures’ success depends not only on the denture base properties but also on their bond strength to a reline resin, as poor adhesion may cause microcracks and microfractures that may decrease denture strength.33 The present study evaluated shear bond strength because the stress at the interface between a denture base and reline resins is essentially of shear type.34
The present study found no statistically significant diferences between different relined denture base resins after physical and chemical aging; thus, the first null hypothesis was confirmed. Changing the denture base resin’s composition does not seem to affect the adhesion properties.34 Nevertheless, the Denture 3D+ printed resin tended to have high values of shear bond strength, probably due to including the hydroxyethyl methacrylate (HEMA) monomer, known to provide a high bond strength.20
The bond strength between the base and the reline resins must be as strong as the core of the denture base resins; thus, it depends on reline resins’ chemical composition and their monomer’s penetration and diffusion on the denture base resins.31 In the present study, the bond strength of relined Probase Hot specimens was higher with Probase Cold reline resin than with Ufi Gel Hard C resin. These results may derive from Probase
Cold and Probase Hot having the same chemical composition, based on PMMA polymer and methyl methacrylate (MMA) monomer.29 The diffusion and penetration of the lowmolecular- weight monomer MMA from the reline resin into the denture base resin form an interpenetrating polymer network, contributing to higher bond strength.31 The mean value of shear bond stress was lower when using Ufi Gel Hard C, probably because this resin has a high-molecular-weight dimethacrylate monomer - 1,6-HDMA,25,31 which hinders the dissolution of the PMMA-containing denture base resin’s surface, causing less penetration on the denture base resin.31 This fact may be corroborated by the predominance of adhesive failures observed in combinations of Ufi Gel Hard C with Probase Hot and V-Print Dentbase resins.
Given the results obtained, the second null hypothesis, which argues that the reline resin does not affect the bond strength to the denture base, is rejected since specimens of Probase Hot rebased with Probase Cold obtained higher bond strength values than with Ufi Gel Hard C.
An adhesive failure mode may indicate that the bond strength between resins is weaker than the reline material’s strength, which is advantageous in the case of temporary relining.34 Specimens manufactured with Denture 3D+ showed a predominance of cohesive failures, supporting the tendency towards high adhesion values mentioned above.
One limitation of this study is the adhesive interface’s reduced diameter compared to the interface resulting from na existing denture relining. Another limitation is the need to carry out the tests in a salivary environment, more similar to what happens in the oral cavity.
The growing use of CAD-CAM technology demands more research on 3D printing, namely to study the bond strength of prostheses manufactured by the additive method to acrylic teeth and their subjection to biodegradation and cyclic forces, simulating chewing.