Introduction
Guided implant surgery uses reverse engineering methods and can provide greater accuracy in implant installation than freehand surgery, except for regions with good bone volume and easy access, where both methods lead to similar results.1,2Therefore, guided implant surgery is particularly useful for regions with low bone volume, reduced interproximal space, or complex anatomical structures. However, it has the disadvantage of hindering bone tissue irrigation during osteotomy compared to the freehand technique because the surgical template on the teeth or alveolar crest and the metal sleeves that guide the drill act as physical obstacles for the irrigation solution to reach the drilling site in depth.3-5
Maintaining cellular activity around the implant is mandatory for the early osseointegration process.6 However, the difficulty of obtaining adequate irrigation in guided implant drilling may increase the local temperature because of the low thermal diffusion of the bone, generating sequelae or even impairing osseointegration due to thermal injury.7 A systematic review8 reported a wide temperature range of 28.4 to 64.4°C, reflecting the great heterogeneity among studies on guided surgery, such as different types of bone or substitute specimens, drilling parameters, and thermal measurement methods.
Previous studies used different irrigation protocols, varying in volume,9 temperature,10,11and source (external, internal, or both) of the irrigating solution.12-15 Although the procedures using local irrigation seem to control the heat production generated by bone drilling to some extent,7 the literature still does not have conclusive evidence on the most effective protocol of local irrigation during guided implant drilling.
This in vitro study aimed to compare the effect of four external irrigation protocols, based on clinical practice, differing in temperature, irrigation source, and volume of saline cooling solution, to control the bone temperature rise during bone drilling in guided implant surgery. The null hypothesis was that bone temperature during drilling is controlled equallywith different external irrigation protocols.
Material and methods
Bovine ribs were cut to obtain ten bone specimens. The sample size calculation indicated the need for nine perforations per group, and an additional specimen was prepared to increase the statistical power. All ribs were removed from the same animal, weighing around 450-500 kg (alive), and were obtained from a local store. The bovine rib was chosen due to its thermal conductivity16,17 and cortical density,18 similar to the human mandible.19 The ribs were stripped, cleaned, rinsed with hydrogen peroxide and saline solutions, and cut to obtain ten bone specimens of 8-cm length, 4-cm height, and 2-cm thickness. Then, the bone specimens were fixed in stone plaster bases (Durone IV Salmon, Dentsply Sirona, York, PA, USA) through the epiphysis, keeping the diaphyses on the sides, and stored in a physiological saline solution at 0ºC.
Each bone specimen was scanned using cone-beam computerized tomography to produce a DICOM file (Digital Imaging and Communications in Medicine) that was then segmented in a virtual planning software (coDiagnostiX, Dental Wings Inc., Straumann, Basel, Switzerland). The bone sites to be drilled were selected in the segmented images to choose the metal sleeve required for each implant perforation.
In the virtual planning software, an implant (Bone Level Tapered Roxolid® SLActive® implant, Straumann, Basel, Switzerland) of 3.3-mm diameter and 10-mm length was selected, as well as the required drill, drilling location, and guide sleeve.
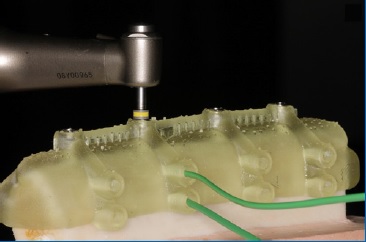
The stainless-steel drill was the Twist Drill PRO (Straumann, Basel, Switzerland), of 2.8-mm diameter and 20-mm length, and the respective sleeve was the Guided Surgery T-Sleeve (Straumann, Basel, Switzerland), of 2.8-mm diameter and 6-mm heigh, positioned at 4 mm from the bone crest (H4). A stop-point for the drill was created in the template based on the sum of the sleeve height and its distance from the boné crest, establishing a depth of 10 mm for all drilling procedures (Figure 1).
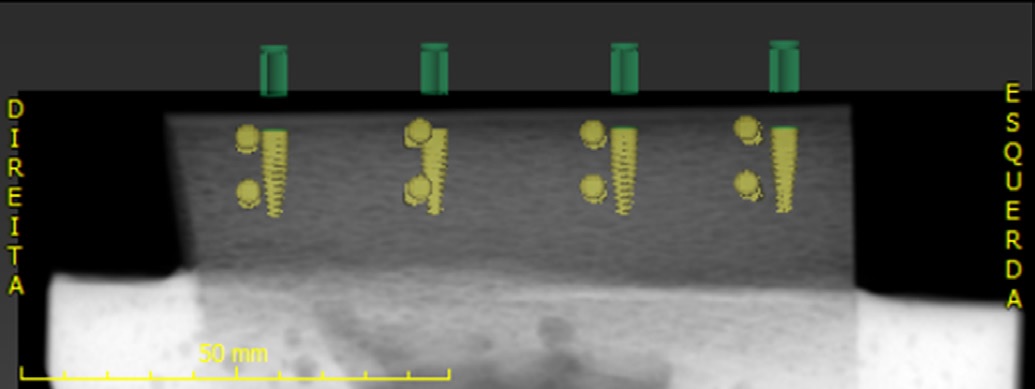
Figure 1 Virtual planning of the sleeves’ height in the software. The 20-mm-long drill was supported on the metal sleeve to guarantee a 10-mm drilling depth.
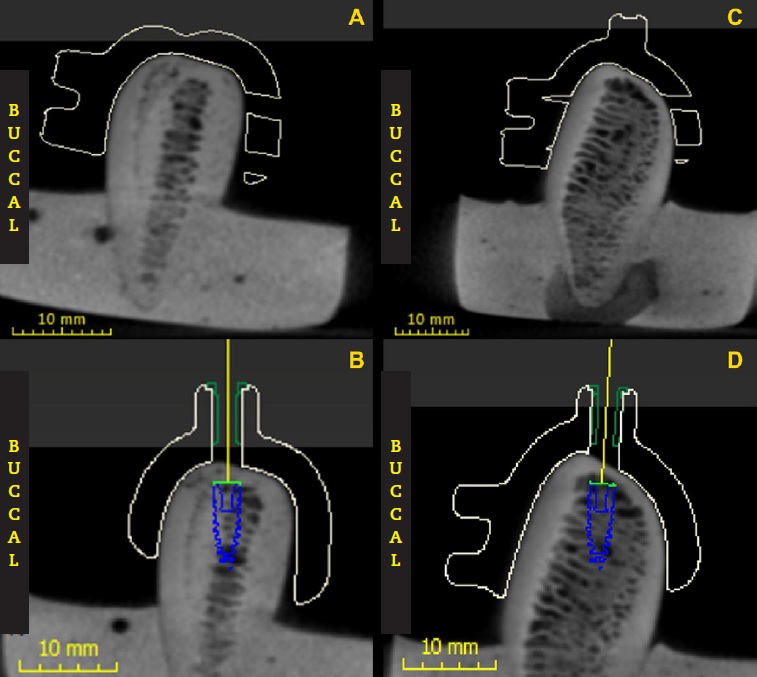
In the virtual planning software, two small 2-mm-long tubular extensions were designed next to each future perforation, one at the apical region and one at the cervical region (Figure 2). Corresponding tubular holes were made in the boné specimens to allow the insertion of thermocouples at a distance of 1 mm from the drilling area.
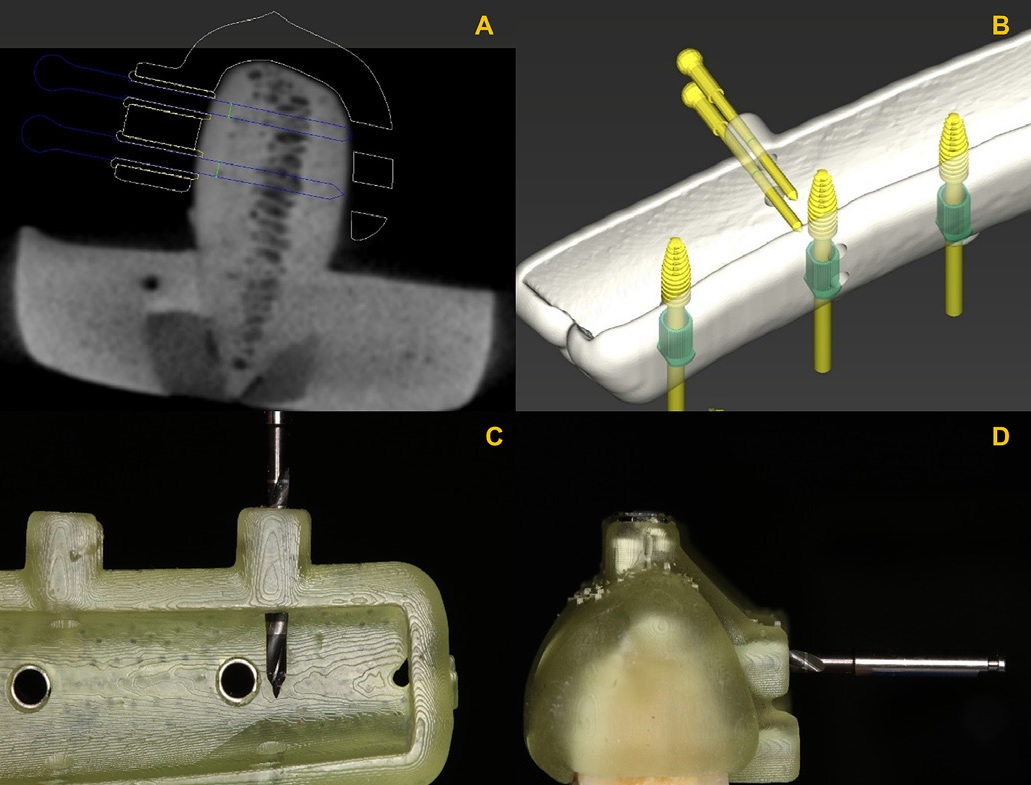
Figure 2 Virtual planning of the lateral perforation of the guides so that the thermocouple was positioned at 1 mm from the region to be drilled (A and B). Measurement and drilling according to the virtual planning to create the lateral holes for the thermocouples (C and D).
After the virtual planning, the designed template guides were prototyped using a 3D printer (P30 Rapid Shape, Straumann, Basel, Switzerland) in autoclavable poly(methyl methacrylate) resin (P pro Surgical Guide Clear, Straumann, Basel, Switzerland). The metal sleeves were positioned on the guide at their predetermined sites. The surgical guide had a precise fit on each specimen without requiring fixing screws.
For the irrigation methods, four irrigation protocols were tested, differing in temperature, volume, and irrigation source of the saline cooling solution:
- Control group (CG): external irrigation using a 10-ml syringe with 25ºC saline solution;
- Group 1 (G1): external irrigation using a 10-ml syringe with 10ºC saline solution;
- Group 2 (G2): combined irrigation using a handpiece and a 10-ml syringe with 25ºC saline solution; and
- Group 3 (G3): combined irrigation using a handpiece and a 10-ml syringe with 10ºC saline solution.
The irrigation speed was set at 0.5cc/s.
The temperature was measured with a digital thermometer (MT-455A, Minipa, São Paulo, SP, Brazil) connected to two K-type thermocouples (Cromel / Alumel, Minipa, São Paulo, SP, Brazil). One thermal sensor was positioned at the apical region and the other at the cervical region of each bone specimen to record both temperatures simultaneously. The bone hole for each thermocouple was perforated individually using the template to align the sensor with the specific point of interest.
The bone specimens were immersed in a water bath at 35ºC until reaching approximately that temperature to simulate body temperature. After the end of each osteotomy, the bone specimen was stored in the water bath until reaching approximately 35ºC again before the next drilling test. Bone drilling was performed by the same operator, who had board certification in Implantology, in a room with a controlled temperature of 25ºC.
Forty osteotomies were drilled to a depth of 10 mm in tem bone specimens so that each specimen received four perforations, i.e., one perforation per group (CG, G1, G2, G3). Two new drills (Motor Surgic Pro, NSK Nakanishi, Tokyo, Japan) were used for a maximum of 20 perforations each.19,20The drilling was carried out alternately between the specimens and the experimental groups according to a previously established drilling sequence. The drilling speed was 800 rpm for all perforations, following the manufacturer’s recommendations.
During each test, the display of the thermal device was filmed with a high-definition camera (Galaxy Note 10, Samsung, Seoul, South Corea) to record the initial temperature of the specimen before drilling (T0), the maximum temperature (Tmax), the minimum temperature (Tmin), and drilling time during osteotomy in the cervical and apical regions (Figure 3). The operator was not blinded to the control and experimental groups, but another investigator was responsible for the irrigation protocol during the surgical procedure.
Two variables were created to indicate temperature changes during bone drilling: temperature variation (var = Tmax - T0) and temperature amplitude (amp = Tmax - Tmin). These factos were computed separately for the cervical (C) and apical (A) bone regions: varC, varA, ampC, and ampA.
The data were analyzed using a randomized block one-way ANOVA to compare the effect of each factor. Pearson’s correlation coefficients were used to analyze the association between drilling time and temperature changes. All tests considered a significance level of 5%.
Results
A total of 40 osteotomies were performed. Table 1 shows the descriptive statistics of the experimental groups for temperature changes and drilling time. The average initial temperatures were 34.9°C and 36.7°C, and the maximum temperatures were 42°C and 44°C for the cervical and apical areas, respectively.
Table 1 Descriptive statistics of temperature changes (in Celsius degrees) and drilling time (in seconds) at cervical and apical regions for the four study groups (n =10).
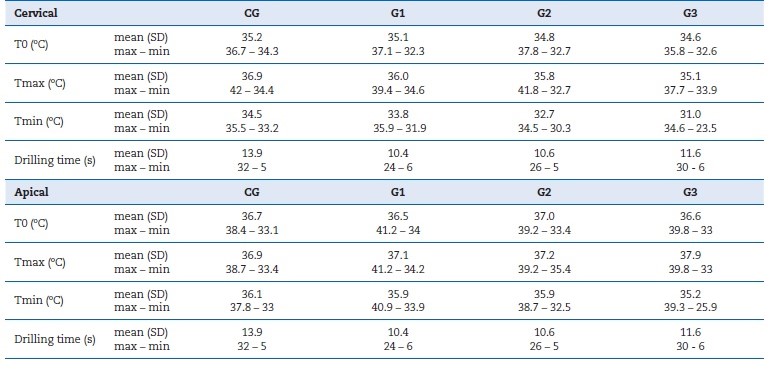
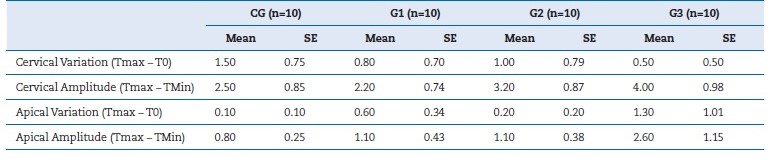
Table 2 shows the comparison of temperature changes among the experimental groups. There was no statistically significant difference among groups, but factor varC showed a trend (p=0.066). The block effect was significant due to the difference between bone specimens (diferente ribs).
Table 2 Means and standard error (SE) of cervical variation, cervical amplitude, apical variation, and apical amplitude (in Celsius degrees) for the four study groups.
Most experimental groups had a positive association between drilling time and bone temperature (Table 3). Bone specimens 1 and 10 (ribs with cortical bone visually thicker) required longer drilling time (between 16 and 32 seconds) and reached the highest values of varC (increased local temperature).
Table 3 Correlations between drilling time and temperature variation by group (n = 10) and total sample (n = 40).
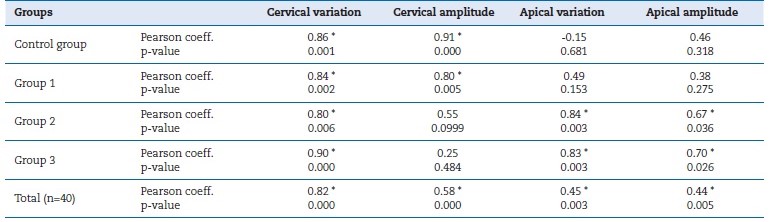
* Statistically significant at the confidence level of 0.05 (2-tailed).
However, they also had high ampC values (decreased local temperature). Specimens (ribs) 5 and 7 had the shortest drilling times (between 5 and 8 seconds), and both showed no increase in temperature beyond the initial temperature. There was only a reduction in temperature from local irrigation (specimen 5 = mean of 2.0°C for ampC and 0.7°C for ampA; specimen 7 = mean of 1.5°C for ampC and 0.4°C for ampA). Specimen (rib) 1 had the longest drilling times (CG = 32 s, G1 = 24 s, G2 = 26 s, and G3 = 30 s) and the largest temperature variation and amplitude (mean varC = 7.0°C; mean ampC = 7.7°C; mean varA = 4.0°C; and mean ampA = 5.0°C). This specimen had the most amount of cervical cortical bone in the sample, and the perforations were very close to the vestibular cortical plate (Figure 4).
Discussion
This study showed that all tested irrigation protocols effectively controlled bone temperature during bone drilling through guided implant surgery. No experimental group showed better cooling potential than the others due to variations in temperature, volume, or irrigation source of the cooling saline solution. Therefore, the null hypothesis was not rejected. The analysis was done separately for the cervical and apical bone sites due to their distinct characteristics of drilling and irrigation. Moreover, none of the osteotomies reached the previously suggested critical biological temperature of 47°C.21
Regarding the temperature of the cooling solution, the present results are similar to those of a previous study using infrared thermography, which found no significant decrease in bone temperature with saline solution at 3°C or 20°C.10 In contrast, a study11using an electric thermocouple showed statistically significant differences among irrigation solutions at 10°C, 15°C, and 20°C for osteotomies with 1.8-mm depth, which were mostly in cortical bone. However, the smaller bone thickness could result in lower thermal increase values and reduced drilling time.22
The present study tested two external irrigation sources commonly used in clinical practice, i.e., disposable syringes and the handpiece itself, and found no difference in termal changes for either of these protocols. Strbac et al.23 found that the combined (external and internal) irrigation provided a greater reduction in bone temperature than the external irrigation alone, but it was not superior to the internal irrigation. A study13 using internal irrigation also presented similar conclusions. However, both studies simulated freehand surgery and not guided implant drilling. Benington et al.12 concluded that no evidence justified using internal irrigation (the most expensive method) since external irrigation effectively reduces bone temperature during drilling.
Other studies20,24,25also reported that external irrigation is safe for maintaining the bone temperature below the critical temperature for thermal injury. As for the volume of the irrigation solution, Sindel et al.9 reinforced the importance of external irrigation to control the bone temperature during implant drilling and found no difference in supplying saline solution at 12 or 30 mL/min externally, using the handpiece. Since an exaggerated increase in the saline volume during surgery can impair the surgical field visibility, keeping the minimum volume necessary for adequate bone cooling is important.
The temperature was recorded in both the cervical and the apical regions of the implant osteotomy to measure the temperature changes during drilling in cortical and cancellous bone, respectively. The cervical region has harder bone tissue and, consequently, is more susceptible to heat production by surgical implant drilling.26,27 Conversely, the internal bone may be less irrigated during osteotomy because of the cooling solution’s limited access.
The available thermal devices still have methodological limitations in measuring and mapping the heat dissipation around the bone, particularly in deep sites such as the apical implant region. Electric thermocouples are widely used in studies on bone thermal changes during drilling, but the resulting intraosseous measurements may not be directly comparable with those of other devices. Harder et al.28 compared intraosseous temperature during implant drilling using the electric thermocouple and the thermographic camera, and both devices showed the same temperature variation, although the thermography detected higher values than the thermocouple. The thermographic camera allows measuring a thermal profile synchronous to the drilling15 but only in the most superficial bone or a transparent material simulating bone tissue. Although thermography may be more accurate for detecting bone temperature, the electric thermocouple captures the same temperature variation but with lower values.
Nevertheless, detecting temperature variation should be the most important factor in assessing irrigation protocols for adequate local bone cooling.
As expected, there was a positive association between drilling time and temperature changes in the bone. Although local irrigation can control the temperature rise, there is no confirmation that irrigation reaches all points of the drilling site simultaneously, i.e., there may be some areas with higher temperatures than others. However, greater control during the implant osteotomy can prevent the drill from being in contact with the bone any longer, reducing the risk of excessive heat production. The literature still lacks solid evidence about the association between cortical bone thickness and temperature increase. It would be useful to estimate the required osteotomy time according to the amount of cortical bone to control the local temperature during implant surgery.
The present study showed an average temperature amplitude (Tmax - Tmin) of 3.0ºC in the cervical region. Specimens 5 and 10 had very different drilling times (6.3 s and 20.5 s, respectively) while maintaining a decrease of 1.97ºC and 1.90ºC, respectively, below the initial temperature (mean cervical T0 = 34.9ºC). These findings suggest that thicker cortical bone would lead to a longer drilling time and, consequently, to an increase in local temperature. Simultaneously, a longer drilling time also means a longer contact time of the bone with the irrigation solution, which could maintain a thermal balance. Thus, both an increase and decrease in temperature can occur during osteotomy depending on many clinical and technical factors, which should be explored in the future.
One of this in vitro study’s limitations is simplifying clinical conditions, which was necessary to standardize the experimente and control potential confounders. Surgical guides were fabricated the same way they would be for in vivo studies to replicate the clinical practice. However, the lack of soft tissues around the bone surface can generate variations in heat dissipation, local irrigation access to the drilling site, and temperature detection. Although only two drills were used for the 40 perforations, the wear of the drill did not influence temperature variations.20,29As the temperature rise during guided implant surgery is multifactorial, other factors such as boné cortical thickness, drill characteristics, drilling time, and drilling speed should be further investigated using a standardized methodology.
In summary, considering the limitations of a laboratory study, local external irrigation effectively controlled the bone temperature, regardless of the volume, irrigation source, and temperature of the saline solution. In all four tested groups, the bone temperature remained between 23.5ºC and 42.0ºC in the cervical and apical regions, which is clinically acceptable.
Conclusions
According to the methodology used, the results suggest that: - The four external irrigation methods tested were equally effective in controlling the rise in temperature during guided implant drilling, both in the cervical and apical bone regions. - Longer drillings caused a greater increase in bone temperature changes, but local irrigation controlled any potential hyperthermia.