Introduction
Asperger syndrome (AS) is a mild neurodevelopmental disorder that belongs to autism-spectrum disorders (ASD). It manifests itself through changes in social interaction, communication, and behavior.1,2Individuals with AS have common characteristics, identified according to three specific functional domains known as the Wing Triad: social relationships capacity, communication skills, and mental and behavioral flexibility.1,3
Individuals with AS have unique characteristics (impaired social interaction, communication difficulties, repetitive behaviors, and interests) that can negatively affect the individual’s daily oral care.4 While some authors claim that these individuals’ oral hygiene status is similar to healthy individuals, others state that individuals with developmental disabilities have an increased prevalence of oral diseases, such as dental caries and periodontal diseases.5 The reported reasons for the oral hygiene deficit are reduced dexterity, decreased learning capacity, sensory problems, nutritional deficiencies, increased affinity for sweets, and atypical eating habits.6
Moreover, because these individuals are very sensitive to loud noises, bright lights, different smells, and the presence of instruments in the oral cavity, dental appointments can become challenging.7,8
This syndrome’s characteristics may favor the absence of adequate oral health habits, creating favorable conditions for etiological factors that lead to oral diseases. The absence of adequate treatment and follow-up favors oral disease progression and oral health status degradation, consequently decreasing these individuals’ quality of life and general health.
The existing literature in this area is still quite inconclusive and insufficient, so this study aims to evaluate the oral health status of this population and identify factors that may influence it. Moreover, by identifying the main oral problems and characteristics of individuals with AS, it will be possible to suggest improvements to promote their well-being and the success of dental treatments.
Material and Methods
This community-based, cross-sectional study was carried out at the Portuguese Association of Asperger’s Syndrome (APSA), Lisbon. All APSA members were invited to participate (n=50), but only 23 individuals with AS met the following inclusion criteria: having AS, being 18 years or older, and reading and signing the informed consent. All sexes, ethnicities, and social levels were included.
The Ethics Committee at the Faculty of Dental Medicine of the University of Lisbon (FMDUL) approved the study protocol, and the international standards of the Helsinki Declaration regarding people with special needs were followed. After approval by the APSA management, informed consent was obtained from each individual. Total confidentiality and anonymity of the data collected were guaranteed.
After the signed consent, the study was divided into two stages: the questionnaire application and the evaluation of the dental, gingival, and oral hygiene status. The questionnaire used for data collection was adapted from two previous works and applied by interview.9,10It consists of 20 multiple-choice questions divided into three sections: a) sociodemographic data, pathologies, and medication; b) oral health, dental history, oral hygiene habits, and behavioral conditions; c) eating habits. The facial validation of the questionnaire was obtained through its application to five patients of the special needs clinic at the Faculty of Dental Medicine of the University of Lisbon.
An oral examination was conducted to assess the dental, gingival, and oral hygiene status based on the following parameters: the decayed-missing-filled index (DMFT),11 the gingival index (GI),12 and the simplified oral hygiene index (OHIS), which comprises the combined debris index (DI) and calculus index (CI).13 The observations took place at the institution, in a room with natural light and using only an intraoral mirror and a CPI probe. They were made by a single examiner (the first author), who was trained and submitted to an intra-observer calibration every five observations. The kappa value for caries diagnosis was 0.92.
Data were treated using the statistical software “Statistical Package for the Social Sciences” (IBM SPSS Statistics Base version 26.0). After verifying the non-normality of the variables with the Kolmogorov-Smirnov test, the Mann-Whitney and the Kruskal-Wallis tests were used to test associations between variables, considering a significance level of 0.05. The variables’ descriptive analysis was done by calculating absolute and relative frequencies. For numerical variables, central location measures (mean) and dispersion measures (standard deviation, minimum, and maximum) were also calculated.
Results
Of the 23 individuals with AS, 18 (78.3%) were male. Ages ranged between 19 and 41 years old, and the average age was 26.7 (± 5.18) years. In addition to AS, 12 (51.6%) participants had mental and behavioral disorders, such as depression and/or anxiety, and three (12.9%) had respiratory diseases. Only eight (34.8%) had no associated pathology. In the group, 15 (65.2%) participants were taking medication.
According to the Anatomical Therapeutic Code classification, most drugs were for the central nervous system, in 11 (47.8%) participants. The reported side effects were vomiting (n=12; 52.2%), xerostomia (n=9; 39.1%), and taste alterations (n=4; 17.4%).
Regarding self-perceived oral health, 12 (52.2%) participants rated it as “good” or “very good,” seven (30.4%) as “reasonable,” and four (17.4%) as “weak.” As for the brushing frequency, 14 (60.8%) participants brushed two or more times a day, seven (30.4%) once a day, and two (8.7%) rarely. All were autonomous in brushing, but six (26.1%) needed a reminder to do it. All respondents used toothpaste, 10 (43%) mouthwash, four (17.2%) dental floss, and three (12.9%) an electric toothbrush.
Most (n = 20; 87%) reported previous dental treatments, all in private clinics. The most frequent reason for oral health appointments was dental caries treatment (n=13; 56.7%), followed by scaling (n=10; 43.5%) and orthodontic treatments (n=8; 34.8%). Only eight (34.8%) attended regularly for oral health check-ups. The last oral health appointment was three or more years ago for 10 (43.4%) participants and took place in the last year for nine (39.1%).
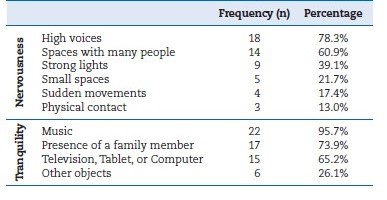
During oral appointments, the main condition that caused nervousness in the group was “loud voices” (n=18; 78.3%). In contrast, “music” (n=22; 95.7%) enhanced tranquility. Most respondentes (n=15; 65.2%) preferred that, during the appointment, all treatment procedures were explained calmly, using audiovisual means. None required physical restraint, sedation, or general anesthesia to perform treatments (Table 1).
Regarding sugary food consumption, eight (34.8%) participants consumed it occasionally, eight (34.8%) every week, and seven (30.4%) every day. Soft drinks were consumed every week by four (17.4%) respondents and every day by another four (17.4%). Food was given as a reward for “good behavior” for 10 (43%) of the participants, and sugary foods were used in three (12.9%) of these cases.
An average of 30.09 (± 1.83) teeth were present. The average DMFT was 2.65 (±2.81) [0;9], and 65.2% of the individuals were free from active caries. Most participants (n=20; 87%) had not lost any teeth from caries, and almost half (n=11; 47.8%) had no teeth filled. Decay affected mostly third molars (n=9; 69.2%), and the most filled teeth were the first molars (n=24; 53.3%).
The participants with lower DMFT were those who needed a reminder to brush, those who recently had an oral appointment, those who used dental floss and an electric brush daily, and those who took non-xerostomia medication. However, the relationships between DMFT and any of the variables analyzed were not statistically significant (Table 2). Five (21.5%) of the participants showed signs of bruxism, one (4.3%) had extrinsic stains, and one (4.3%) had microdontia.
Table 2 Descriptive characteristics and relations between the decayed-missing-filled (DMFT) index and its componentes with the daily habits
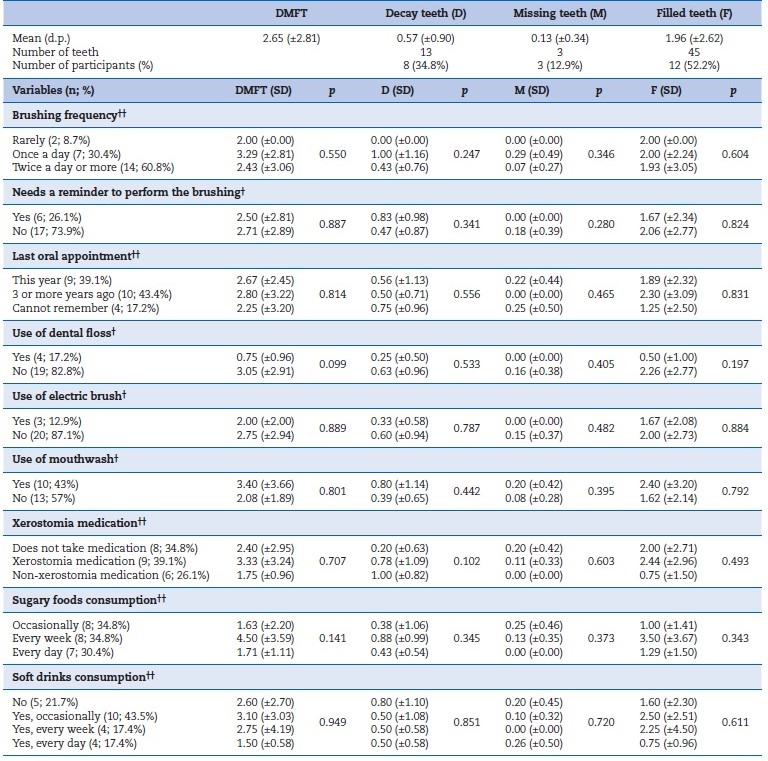
The data were analyzed according to the non-parametric tests Mann-Whitney (†) and Kruskal-Wallis (††), at a significance level of p < 0.05. SD, standard deviation.
The average GI was 1.06 (±0.36), and eight (34.4%) participants presented gingival recessions. According to the GI classes, 12 (52.2%) corresponded to “good” and 11 (47.8%) to “reasonable.” Participants who brushed their teeth two or more times a day and used dental floss daily had a lower GI. However, the relationships between GI and the variables analyzed were not statistically significant (Table 3).
Table 3 Descriptive characteristics and relations between the gingival index (GI) and the daily habits
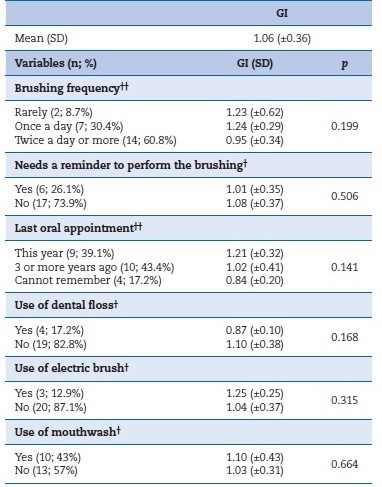
The data were analyzed according to the non-parametric tests Mann-Whitney (†) and Kruskal-Wallis (††), at a significance level of p < 0.05.
SD - standard deviation.
The mean OHIS was 2.08 (± 0.73) (DI = 0.99 (± 0.46) and CI = 1.09 (±0.42)). Considering the OHIS classes, 19 (82.6%) corresponded to “reasonable,” two (8.7%) to “good,” and two (8.7%) to “weak.” The participants who brushed their teeth more frequently, those who were reminded to brush, and those who used dental floss and an electric brush daily had lower OHIS and DI, despite no statistical significance. Those who had a recent oral health appointment had a lower CI (p=0.021), as well as those who brushed their teeth more frequently (p=0.038) (Table 4).
Table 4 Descriptive characteristics and relations between the simplified oral hygiene index (OHIS) and its componentswith the daily habits
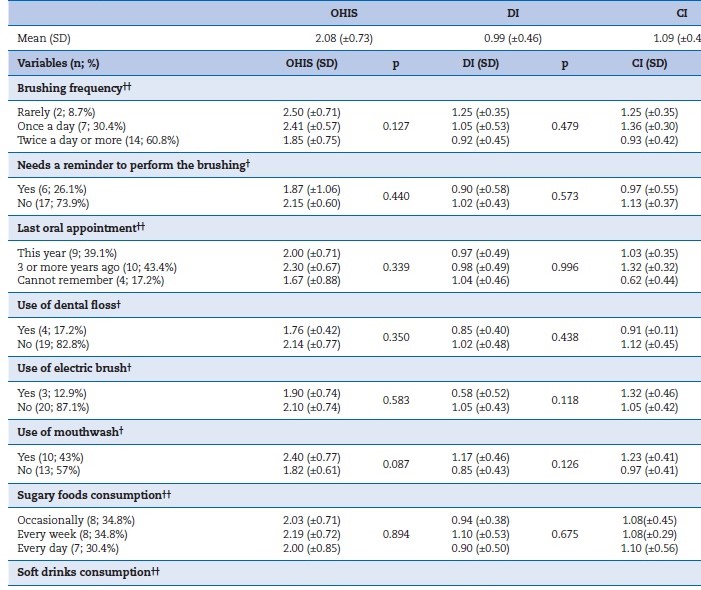
*Statistically significa nt; the data were analyzed according to the non-parametric tests Mann-Whitney (†) and Kruskal-Wallis (††), at a significance level of p < 0.05.
DI, debris index; CI, calculus index; SD, standard deviation.
Discussion
This study aimed to evaluate the oral health status of individuals with AS and identify potentially influential factors in order to help determine their main oral problems/characteristics and suggest improvements to promote these individuals’ well-being in the appointment and their treatment success.
The predominance of the male sex in the sample (78.3%) reflects the higher incidence of AS in this sex.14 Most of the sample (51.6%) had additional mental and/or behavioral disorders corresponding to psychiatric diseases such as anxiety and depression. A 2011 study of participants with ASD (including AS) reported that 72.5% had at least one psychiatric diagnosis.15 Depression is one of the most diagnosed disorders in patients with AS,16 as well as anxiety.17 These findings agree with this study, where 41% and 56% of the participants had those conditions, respectively. Most participants took medication, which is coherent with a 2014 study.18 The medication is intended to treat these disorders and corresponds to antidepressants, antipsychotics, and anxiolytics, among others, as the literature shows.19 The reported side effects were vomiting and xerostomia, also prevalent elsewhere.18 These have consequences for the oral cavity: recurrent vomiting causes erosion and dental sensitivity, which can potentiate the appearance of dental caries and periodontal disease.20
Regarding oral hygiene care, most participants brushed their teeth twice or more daily (60.8%), and 8.7% rarely brushed. Conversely, a study of individuals with and without ASD found higher percentages of “rarely” in both: 36.5% and 62.2%, respectively.9 Although our study figures are better, they are still below the recommended twice-a-day brushing for all. When comparing these figures with data from a national study of the Portuguese population, the percentage of individuals who brushed their teeth twice or more daily was higher (age group 18 years - 78.1%; age group 35-44 years - 74.3%).21
About one-fifth of the sample flossed their teeth daily, which is considered a low percentage, although higher than the national study results (age group 18 - 6.4%; age group 35-44 - 14.8%).21 Despite the low percentage of users (12.9%), using an electric toothbrush can be a practical option because it does not require as much manual dexterity as the traditional one.
Concerning eating habits, about 30% of the sample consumed sugary foods daily. This consumption in ASD individuals is problematic because of their higher risk of dental caries due to their preference for soft and sweet foods, their habit of keeping foods in their mouth longer, and their difficulty in achieving good oral hygiene.22 Although 43% of this study’s participants were rewarded for good behavior with food, Onol and Kırzıoğlu9 observed higher percentages (73.8%).
Regarding access to dental treatments, most participants (87%) had already performed dental treatments, and the percentagem was well above that recorded in a group with ASD.9 Moreover, even though in this study all treatments were in private clinics, in another study, only 14% of the participants with ASD were treated in that type of clinic.9 However, only 34.8% visited oral health professionals for preventive reasons, which is similar to a national study’s results for the 18-year age group (37%) and higher than the 35-44-year age group (17.8%).21 These data show that most of the sample only visited an oral health professional for treatment purposes, missing the opportunity to prevent oral diseases with less expensive and easier treatments and suffering less pain, which is particularly important for this group of patients.
In matters of behavior in dental appointments, the conditions that cause nervousness and those that promote tranquility reported in this study coincided with those observed by Onol and Kırzıoğlu.9 None of the participants had needed physical restriction or general anesthesia yet, contrary to what was observed by other researchers.9
Previous studies showed that a sensorially adapted dental environment reduced anxiety and increased cooperation in individuals with ASD.7,23Dentists/dental hygienists should explain the procedures and materials to be used since the tactile, auditory, and sensory hypersensitivity of patients with AS can lead to unpredictable reactions.24 In fact, one of the most effective approaches to reducing anxiety is to increase the patient’s control by informing them about the type of sensations they may experience.25Also, when visual pedagogy is used in children with ASD, their ability to cooperate during the appointment is greater.26 However, ultrasonic scaling should be avoided because the equipment’s noises and vibrations can cause hypersensitivity reactions.
For patients with AS, it is beneficial that the clinic’s environment is calm. The presence of many people in the office and a higher tone of voice should be avoided because these factors increased nervousness in 60.9% and 78.3% of participants, respectively. The presence of a family member and background music helps maintain tranquility and relaxation in 73.95% and 95.7% of the participants, respectively. These patients prefer having the treatment procedures explained to them in advance, using visual pedagogy if possible. The “tell, show, do” technique can be appropriate to the characteristics and needs of these patients. These measures avoid unpredictable reactions and increase their cooperation.
During the contact with this group, the researcher noticed that the toothpaste taste could cause discomfort and even lead to choking during brushing. With this in mind, oral health professionals should opt for toothpaste with neutral flavors so brushing can be comfortable and not cause anxiety.
Although there are many articles about ASD and oral health, the literature regarding only AS and oral health status is weak. Thus, all comparisons below are made with literature involving individuals with ASD or otherwise healthy individuals.
AS does not comprise any typical intra or extraoral change.5,27,28However, more than one-fifth of the sample underanalysis (21.5%) showed signs of bruxism, which has been reported as a sleep pr oblem experienced by individuals with ASD.29 Further investigations should be conducted to analyze whether this may be a condition associated with these patients.
The high mean number of teeth in this study indicates that not many were lost, and the absence of dental and gingival changes in more than half (52.2%) of the sample aligns with the literature5,27,28 The DMFT of 2.65 (±2.81) obtained corresponds to a low prevalence of dental caries, according to the WHO.30 Higher values were recorded for individuals with ASD but lower in individuals without ASD in several studies.9,31-33
The same studies reported higher values for components D and M but lower for component F.9,31 All values regarding DMFT and its components were lower than the national average (age groups 18 and 35-44 years), except the component F (in the 18-year age group).21 This suggests that these participants are concerned about treating decayed teeth and maintaining good oral health. Most participants (65.2%) were free of active caries, a value much higher than that recorded by other authors (31.9%).34 The prevalence of caries lesions in molars coincides with Naidoo and Singh’s findings.31
Although there was no statistically significant relation, the participants who needed a reminder to brush their teeth had a lower DMFT, as well as those who had an oral appointment, demonstrating that family can play an important role in helping maintain oral health. Although participants taking medication had a higher DMFT, the relation was not significant, as in previous studies.34
The GI in this study was 1.06 (±0.36), corresponding to mild gingival inflammation, a slight color change, and no bleeding upon probing.12 A mild gingival inflammation without bleeding upon probing was found in most participants. Previous studies found higher values in individuals with ASD and healthy individuals.9,35 This finding demonstrates that these individuals can make a reasonable plaque control. Individuals with gingival recessions were observed, contrary to Khatib et al.’s findings,35 and those may be due to trauma caused by brushing teeth with too much force.
Although with no significant relation, participants who brushed their teeth more frequently and those who used dental floss daily had a lower GI. The lack of manual dexterity may hinder brushing and dental floss use and further contribute to the differences in GI values between participants.33
On average, participants had plaque and calculus up to one-third of the tooth surface, which is reasonable.13 Like the GI, these values were lower than plaque index values recorded for individuals with ASD and healthy individuals in the same studies.9,35 Our findings suggest that these individuals have a good brushing frequency and can perform it effectively, although with room for improvement.
Those who brushed their teeth more frequently had a lower CI, as well as those who had a recent oral health appointment. Again, these results can be justified by the group’s concer about oral health care. The small sample size could contribute to the lack of statistically significant results, preventing the generalization of results and the use of multivariate analysis and only allowing the identification of univariate factors for oral health risks. Given the few studies with an AS population, it is essential to conduct larger studies to determine the oral health needs of this group.
Conclusions
The AS individuals had a low prevalence of dental caries, a gingival state with moderate inflammation, and a reasonable oral hygiene state. Although several factors can influence these individuals’ oral health, they can obtain good results if good oral hygiene habits are maintained, namely tooth brushing and flossing. Further research should be conducted to confirm these results. It is essential that oral health professionals become familiar with the characteristics and manifestations of AS and the resources that can be used to optimize the patient’s cooperation and the success of treatments.