Introduction
Sublingual salivary glands are the smallest of the major salivary glands, located beneath the mucous membrane of the floor of the mouth. These glands can be afflicted by various pathological processes, mostly non-tumoral diseases. Neoplasms of the sublingual salivary glands are unusual, comprising about 1% of all epithelial salivary gland tumors.1
Moreover, metastatic disease to this gland is practically inexistent, with only one case reported in the literature.2 Metaplastic breast carcinoma (MpBC) is a heterogenous subtype of invasive breast carcinoma (IBC) with differentiation of neoplastic epithelium toward squamous or mesenchymal elements, including spindle, chondroid, and osseous cells.3
Most cases have a triple-negative phenotype, meaning a lack of expression of the estrogen receptor (ER), the progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2). MpBC accounts for less than 1% of IBCs and occurs mainly in postmenopausal women. It generally takes an aggressive course with a poor prognosis, with 50% of patients developing distant metastasis after primary breast surgery, commonly to the lungs and bones.4,5 We report the first case of a rare MpBC metastasis to the sublingual salivary gland.
Case report
A female in her 50s was referred to a Stomatology consultation presenting a swelling on the floor of the mouth (Figure 1), causing masticatory and swallowing discomfort. The mass had been growing for the last month since it was initially detected. The patient had a medical history of breast carcinoma diagnosed three years before. At the time, she already had metastatic disease at mediastinal lymph nodes and multiple metastatic nodules located in the lungs, liver, bone, and brain.
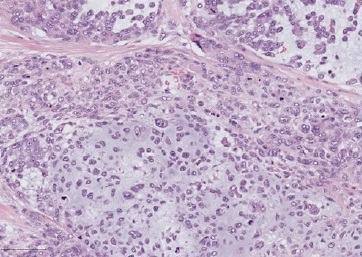
On physical evaluation, a painless 1.2-cm firm nodule was palpable sublingually, leading to the presumptive diagnosis of sialolithiasis. The mass was removed and submitted to pathological examination. Grossly, the lesion was firm and grayish with irregular borders (Figure 2). Histopathology showed a malignant lesion comprising neoplastic epithelial cells arranged in small nests with a large central area of chondroid matrix (Figure 3). The epithelial cells were large, with hyperchromatic and pleomorphic nuclei presenting a high mitotic rate (Figure 4). At the edge of the fragment, salivary parenchyma exhibiting ductal ectasia with scant inflammatory cells was identified.
On immunohistochemistry, the carcinomatous cells expressed cytokeratins AE1/AE3 and CK7.

Figure 2 The surgical specimen: an irregular round mass with a greyish surface and a 1.20-cm diameter
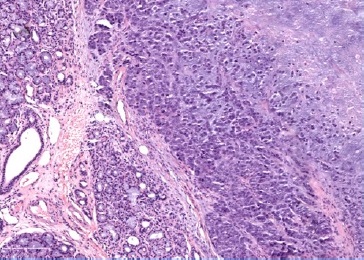
Figure 3 Periphery of the sublingual lesion, showing sublingual parenchyma (left), and tumor with chondroid matrix (right), HE
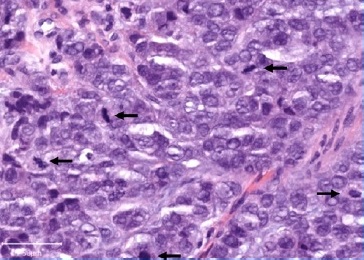
Figure 4 High magnification of the tumoral cells showing high-grade cytological features and several mitoses (arrows), HE
Further investigation of the patient’s medical history revealed that the primary tumor was a HER2-positive MpBC with chondroid differentiation (Figure 5) and positive axillary nodal involvement. She had neoadjuvant treatment (pertuzumab + trastuzumab + docetaxel) followed by modified radical mastectomy with axillary lymph node dissection. The patient then started radiotherapy, adjuvant chemotherapy, and trastuzumab, but the neoplasia progressed under treatment, with disseminated organ metastases.
The slides from the breast carcinoma were reviewed for morphological and immunohistochemistry comparison with the salivary gland tumor. Both showed negativity for GATA 3, ER, and PR. HER2 was negative in the salivary-gland-located tumor. Based solely on histology, we would have pondered primary salivary tumors with chondroid differentiation. From those, pleomorphic adenoma (PA) is a diagnosis to consider, as it is the most common neoplasia of the salivary glands, although uncommon in the sublingual glands. However, the tumor’s histopathological features conflicted with this hypothesis, particularly the marked nuclear pleomorphism. Moreover, the clinical presentation as a rapidly growing mass was incompatible with the PA diagnosis.
For the malignant counterpart, carcinoma ex-adenoma pleomorphic (CExAP), we would need to have histological evidence or clinical history of a previous PA, which we had not.
Given the patient’s medical record and information on the primary breast tumor’s histological type, we diagnosed metastatic breast carcinoma in the sublingual salivary gland. Immunohistochemistry does not help distinguish this entity from PA and CExAP, which are usually ER and PR negative, with variable GATA3 expression.6,7
On the follow-up Stomatology appointment, the patient reported improvement from the discomfort associated with mouthfloor tumefaction. She will continue her oncology follow-up care.
Discussion and conclusions
Tumors in sublingual salivary glands are rare, comprising less than 1% of all salivary gland tumors.8,9Clinically, they form masses on the floor of the mouth and can be misdiagnosed as other more common diseases in that location, such as ranula, chronic sialadenitis, or sialolithiasis, as happened to our patient.
About 90% of the tumors arising in the sublingual salivary glands are malignant, the most common histological types being adenoid cystic carcinoma, followed by mucoepidermoid carcinoma. Together they account for approximately 70% of malignant sublingual gland tumors.10,11 Of the rarer benign tumors, PA is the most frequently encountered neoplasia.11
Metastatic spreading to the salivary glands is uncommon and occurs predominantly in the parotid gland. As this major gland has lymph nodes within, secondary parotid malignancies can either occur as lymph node metastases or by infiltration of the parotid parenchyma. Head and neck tumors make up two-thirds of the metastases, while infraclavicular primary tumors are less likely to spread to the parotid.12 These distant metastases derive from numerous primary sites, including about 30 cases of metastasis from breast carcinomas,13-20and are thought to reach the parotid through the thoracic duct or paraspinal venous plexus.18
The other major salivary glands - submandibular and sublingual glands - are much less frequently affected by secondary tumors. Different from the scenario described to the parotid, the head and neck neoplasias are unlikely to metastasize to those glands, and its involvement occurs through extension from the primary tumor or a locally involved lymph node. Secondary involvement of the submandibular gland from infraclavicular primary sites is uncommon. Reported in the medical literature are isolated case reports or small case series, including a few cases originating from primary breast carcinomas.19,21-27To our knowledge, only one other case reports secondary deposits in the sublingual gland, after a primary renal clear cell carcinoma.2
In our case, the primary tumor was a rare MpBC with chondroid differentiation. This particular histological subtype of breast carcinoma is rare,28 and, as far as we know, has never been reported to spread to any salivary gland. The high incidence of distant metastases and low nodal involvement rates suggests that the hematogenous route plays an essential role in its dissemination.29 In our case, the patient had both lymph node metastasis and extensive hematogenous dissemination to the lung, liver, bone, and brain at the sublingual metastatic diagnosis.
On pathological examination, the chondroid matrix on the secondary lesion brought diagnostic complexity to the case, as we needed to consider primary salivary tumors with chondroid differentiation as possible diagnoses. Morphology and the clinical setting were crucial to achieving the diagnosis.
Immunohistochemistry did not help distinguish primary from metastatic tumors and showed discordance regarding HER2 status between primary and secondary lesions. The sublingual salivary metastasis showed no HER2 expression on immunohistochemistry, while the primary breast tumor was an exceedingly rare HER2-positive MpBC. Phenotype discordance is considered a frequent event during breast cancer progression.
In particular, HER2 discordance in breast tumors has been reported in up to 15% of cases, mainly transforming from HER2-positive status in the primary tumor to HER2-negative status at metastasis/recurrence sites.30,31 This conversion is attributed to intratumor heterogeneity and changes in the molecular profile during tumor progression, spontaneously, or following the selection pressure on tumoral clones inflicted by the treatments,32 such as anti-HER2 drugs used in the patient treatment regime.
To the best of our knowledge, this is the first report on MpBC metastasis to the sublingual gland. The diagnosis of this highly unusual case is challenging, both at the clinical and pathological level, considering the rarity of the primary tumor and the peculiarity of the metastatic disease location.