Introduction
Procedures for facial rejuvenation through fat removal have been gaining ground in the last few years. There are several options for facial contour improvement and aesthetic recovery with variable degrees of invasiveness that upgrade the positioning and volume of cervical-facial tissues.1-4 Double chin lipectomy or liposuction is one possibility for patients with excesso subcutaneous fat in the neck and simultaneously with good skin elasticity. Aspiration cannulas remove fat from the submental region through surgical access and subcutaneous exploration, improving the mandibular contour delimitation.1,2
Correct therapy planning depends on evaluating hard and soft tissues, considering facial muscular anatomy, age, skin laxity, expectations, and medical history.5,6 Factors such as gravitational force, mental ptosis, excessive platysma, and robust digastric muscles may interfere in the procedural decision-making for fat removal.7 Moreover, the adipose tissue’s depth level must be identified to avoid poorly planned and harmful surgeries. Lipectomy is generally restricted to aspiration between the skin and the platysma surface. Other surgical excision options, such as the submental neck lift, are available when fat is in the subplatysmal region.8
The literature points out the subcutaneous hematoma as one of the possible complications after neck cosmetic surgery, with low recurrence and expandable in the first postoperative hours.1-3,8,9 The subcutaneous hematoma is a collection of bloody content in a neoformed cavity that may compress airways and promote the volumization of previously juxtaposed spaces.6 Although infrequent, infections and cervical tissues’ extensive ischemia may also occur parallel with this clinical condition.4,6
Treating hematomas involves surgical fascial spaces’ drainage, drain placement, pain control, and frequent patient monitoring. Correctly handling the condition depends on identifying affected layers and knowing the medical history and etiologies.3,10 It is essential to analyze for edema, dyspnea, pain, and active bleeding related to bruising, ensuring airway patency. Treatment resolution improves the adjacent tissues’ apposition, reduces the risk of ventilatory complications, and refines skin color.6,10,11
Case report
A 25-year-old Caucasian male patient attended the emergency room of our Oral and Maxillofacial Surgery Department 3 days after having done chin liposuction. He complained of decreased neck mobility, shortness of breath depending on head position, pain, and aesthetic damage. He denied underlying pathologies and reported that the procedure had aspirated a large and uncertain amount of fat in addition to breaking muscle fibers. In this consultation, the patient was lucid and oriented in time and space, ruddy, hydrated, anicteric, acyanotic, afebrile, and eupneic. Before the first consultation with our team, he had used a non-specific oral anticoagulant, amoxicillin, and paracetamol, as prescribed by the professional who performed the liposuction. He denied postoperative fluid leakage through the surgical wound.
On clinical examination, we observed a stiff neck swelling involving bilateral submandibular, submental, and superficial cervical fascia spaces, with diffuse violet foci, and a healing submental surgical wound permeated by two simple stitches (Figure 1). The patient also showed a slight limitation in mouth opening. Intraorally, there were no buccolingual swellings, mucosal changes, or foci of dental infection.

Figure 1 Patient on admission with limited cervical movement. A = front view demonstrates a globose, rubbery swelling in the submandibular, submental, and anterior cervical regions, with violet foci in its lower half bilaterally and darker and concentrated on the right anterior-cervical side; B = right lateral view demonstrates a concentrated violaceous extension of the swelling to the mastoid, right platysma, and right sternocleidomastoid muscles’ regions.
The medical report of a contrasted facial tomography (Figure 2) reported extensive densification of subcutaneous and myoadipose planes of the cervical and anterior regions, extending to the face. It also noted substantial edema with thickening of the right sternocleidomastoid muscle and no signs of trauma in bone structures. Hematologic tests revealed leukocytosis, neutrophilia, and altered C-reactive protein (Table 1).
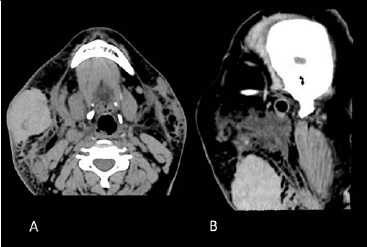
Figure 2 Tomography performed on admission through a soft-tissue window shows homogeneous collections in the cervical region with greater densification on the right side: A = axial section in the mandibular region; B = sagittal section.
Table 1 Laboratory data

a×106 cells. b×103 cells. Hb = hemoglobin; Ht = hematocrit; MCV = mean corpuscular volume; MCH = mean corpuscular hemoglobin; MCHC = mean corpuscular hemoglobin concentration; RDW = red-cell distribution width; A = hospital admission; B = 3rd day; C = 15th day; D = 30th day; E = 10th month; = arithmetic average from A to E; s = sample standard deviation from A to E; RV = reference values; Variation (%) = reduction or increase from A to E
Our team reached a diagnostic hypothesis of subcutaneous hematoma in facial and neck spaces. The patient was admitted for intravenous medication and surgical schedule. Given the important clinical and laboratory changes, the hospital prescribed ketoprofen 100 mg, hydrocortisone 250 mg, and dipyrone 1 g applied at regular intervals.
The swelling showed gradual clinical improvement, becoming more circumscribed and reduced. Thus, local characteristics were more favorable for drainage, given the deepened and extensive aspect in the admission that became more superficial during hospitalization. On the third day of hospitalization, bilateral diffusion of the violaceous areas to the clavicular region and reduced swelling stiffness were noticed.
Besides hospitalization, we opted for aspiration puncture and surgical drainage of fascial spaces associated with the placement of drains through the previous surgical wound. After local anesthesia with prilocaine 3% (Prilonest 3%™ 1.7 ml - DFL S.A; Rio de Janeiro, Brazil), a 10 ml syringe with a 21 G needle in diameter and 30 mm in length collected 7 ml of dark red contente compatible with blood (Figure 3). Afterward, an incision through the surgical wound, divulsion by planes with Metzenbaum scissors, and placement of two Penrose drains were performed. A large viscous amount of dark red blood was removed from the submandibular, submental, and cervical spaces (Figure 4). The immediate postoperative period revealed an important reduction in the volume of facial and cervical planes (Figure 5). No adverse effects or post-surgical complications were noted.

Figure 4 Surgical drainage of fascial spaces demonstrates dark-red collection compatible with blood flowing through the surgical wound region.

Figure 5 Immediate postoperative period of surgical drainage of fascial spaces with the placement of Penrose drains: there is a greater extension of the violaceous color and a substantial decrease in volume compared to the admission.
The patient was discharged from the hospital with substantial but partial recovery of the extraoral swelling and laboratory parameters, subjective perception of respiratory improvement, and reduced local sensitivity. At discharge, considering the persistence of residual edema, he was prescribed ibuprofen 300 mg orally every 6 hours, plus dipyrone 1 g orally every 6 hours; the last one just in case of pain. At the first follow-up visit after 7 days, the patient presented decreased swelling and reduced violaceous foci (Figure 6) and reported slight daily extravasation of blood content since drainage. He denied dyspnea, dysphagia, fever, or other signs of postoperative infection. During the 7-day follow-up, a new face and neck tomography showed blurring of the adipose planes with bilateral subcutaneous emphysema (Figure 7). Leukocytosis persisted in the 15-day follow-up visit and was corrected in the 30-day follow-up visit.

Figure 6 Patient at the first follow-up visit after drainage: volume increase in involution; better facial symmetry; better apposition of the submandibular, submental, and anterior cervical tissues; violet foci bilaterally concentrated; improvement in cervical movement reported. A = front view; B = right side view

Figure 7 Soft-tissue window tomography at the 15-day follow-up visit demonstrates signs of residual emphysema and substantial reduction of homogeneous foci compared to the admission tomography. A = axial view; B = sagittal view
In the subsequent follow-up visits, a more favorable aspect of the neck tissues’ apposition was noticed, with facial symmetry, surgery wound under repair, and edema regression (Figure 8). The patient showed total remission of blood foci in the neck (Figure 9) and clavicular region and satisfactory laboratory parameters improvement only at the 30-day follow-up visit. At the 10-month follow-up visit, the patient had no significant differences, remaining stable and without complaints. CT sections (Figure 10) and clinical pictures (Figure 11) illustrate the patient’s final follow-up. The laboratory variables collected were grouped and analyzed by descriptive statistics, considering relationships between the first day and the 10-month follow-up and percentage variations of each parameter (Table 1).

Figure 8 Patient after 15 days of surgical drainage: clearer involution of the initial condition. A = front view; B = right side view

Figure 9 Patient after 30 days of surgical drainage in front view: satisfactory involution of the initial condition with normal colored skin; complete healing of the surgical access

Figure 10 Soft-tissue window tomography in the 10-month follow-up demonstrates satisfactory tissue apposition. A = axial view; B = sagittal view
Discussion and conclusions
The search for aesthetics and facial rejuvenation with safe and less invasive techniques has increased lately.1 There are numerous procedures for correcting excess fat on the face, but the indication must be precise and focused on the patient’s physical and systemic characteristics.2,3,5 Attempting to remove excess subcutaneous fat in an untimely and poorly planned way may lead to harmful facial changes and substantial risks, such as those observed in our case report.2,8,12
The Federal Council of Medicine of Brazil established na ideal general limit of 7% of body weight for liposuction using an infiltrative technique focused on the abdominal region.13
We understand that this limit for double chin aspiration in clinical practice is much smaller given the neck’s small dimension compared to the abdomen. The literature states that chin liposuction’s amount of aspiration varies according to the fat disposition in the patient and that a thin layer of submental fat should be preserved after the procedure.12 However, we did not find papers discussing the safety limit for submental fat removal, even though complications are reported.1-3,6,9
The literature has contraindicated the use of anticoagulants concomitantly with lipoplasty procedures in patients with a clear history of hypercoagulability diseases, such as deep vein thrombosis, or in whom a low-risk stratification is achieved.14,15 Our patient reported using anticoagulants prescribed by the professional who performed the lipectomy, but the hematologic exams performed in the first appointment did not reveal coagulogram changes.
On admission, leukocytosis with neutrophilia and increased C-reactive protein demonstrated an important inflammatory condition to be corrected, besides the required control of the hematoma’s anatomical expansion and maintenance of air patency. Comparing the day of hospitalization with the 10-month follow-up visit, leukocytes, neutrophils, platelets, and C-reactive protein decreased by 40.7%, 57.2%, 13.1%, and 47.1%, respectively. The laboratory improvement was compatible and concomitant with the patient’s clinical recovery, demonstrating the effectiveness of the proposed treatment.
According to the literature, a thin layer of subcutaneous fat must be left in place during liposuction to avoid unsightly adhesions and prevent damage to the subdermal plexos,12 and subplatysmal fat should not be removed by aspiration.2 Our team believes that the probable rupture of vascularized structures in the superficial cervical fascia and right sternocleidomastoid region, the platysmal involvement, and the patient not having used compression devices or having undergone mechanical lymphatic drainage may explain the formed hematoma.
Thus, the alterations in the admission imaging report and the lack of compliance with those postoperative recommendations12 justify the extensive bruise. The drainage content’s color, quantity, and viscosity revealed excessive blood in ectopic space, increasing the difficulty for biological absorption or final coagulation. There was a significant improvement in imaging aspects in the follow-up, with the cervical-facial tissues more adequately positioned.
Hematomas due to cosmetic neck surgery are considered rare in the investigated literature, and their treatment and other related complications are poorly explored.1-3,8,9 We did not find previous case reports of extensive subcutaneous hematoma due to lipectomy or well-established bruise control protocols for situations like the present one. Nevertheless, one study shows that drains positively influence bruising control in rhytidectomy cases, despite not reducing general complication rates.16 Besides, the literature supports the control of expanding hematomas with surgical drainage and drain placement.2,8
The in-hospital pharmacological choice of hydrocortisone took into account the anti-inflammatory potency of glucocorticoids, which inhibit the production of prostaglandins and leukotrienes and reduce phospholipase secretion, besides decreasing leukocyte migration, consequently helping reduce cardinal pro-inflammatory signs.17 We combined ketoprofen to potentiate the anti-inflammatory action through diferente ways of inflammatory inhibition. The drugs chosen also contributed to pain control. The intravenous route of administration is beneficial by avoiding first-pass metabolism, thus having faster action and maximum bioavailability compared to the conventional oral route.18
Intravenous therapy associated with surgical drainage provided resolution of the condition, although a one-month follow-up was required to observe the complete remission of signs and symptoms. The patient tolerated well the proposed treatment and was satisfied with the aesthetic-functional improvement achieved. This case report’s restricted follow-up is a limitation, but the rarity of the condition observed and its treatment description justify this publication.
Planning for double chin liposuction requires a well-founded physical and systemic assessment of the patient besides understanding the correct procedure indications.3,8 There are limitations in neck aspiration, and the probable incorrect planning and trans-surgical management in the lipectomy performed in the present case led to the extensive condition observed. 2,12 Subcutaneous bruises pose significant risks to the patient, such as airway compromise and necrosis.8 Controlling such hematomas requires clinical, imaging, and laboratory analysis for correct intra-hospital planning, as well as surgical evacuation and drain placement, considering that it can be na actual life-threatening emergency.2,3 The treatment used by our team consisted of intravenous medication, surgical drainage, and follow-up. It led to a good outcome for the patient, was effective, prevented hematoma expansion, ensured air patency, and restored function, aesthetics, and quality of life.

















