Introduction
Temporomandibular joint (TMJ) ankylosis is still one of the main therapeutic challenges in oral and maxillofacial surgery. According to the age and time of ankylosis, patients have diferente levels of local and systemic involvement. Frequent clinical signs are difficulty opening the mouth, facial asymmetry, mandibular micrognathia, and major changes in the occlusal plane.1
Basically, ankylosis is characterized by an anatomical-functionalalteration that occurs by bone or fibrous fusion between the temporal articular fossa and the mandibular condyle, resulting in an extremely limiting condition for the patient.2
Trauma is one of the main causal factors of TMJ ankylosis, followed by ear infections such as otitis, rheumatoid arthritis, ankylosing spondylitis, scleroderma, TMJ tumors, radiation, congenital deformities, postoperative TMJ surgeries, complications in orthognathic surgery, and use of bisphosphonates; however, it can also be idiopathic.3 Condylar fractures are among the facial fractures that most commonly cause ankylosis.
They are considered one of the most complex fractures of the mandible, given their unique joint anatomy and the disagreements regarding the appropriate surgical or conservative treatment. Due to the TMJ’s peculiar characteristics, diseases such as post-traumatic ankylosis are highly likely to arise after condylar trauma.4
TMJ ankylosis can be classified according to its location as intra or extra-articular, to the tissue involved as fibrous, bone, or mixed, and to the degree of fusion as complete or incomplete. Its diagnosis is primarily clinical, but complementary exams are essential to complement the assessment and carry out therapeutic planning.5
Several treatments have been used to manage TMJ ankylosis, such as gap arthroplasty, interpositional arthroplasty and TMJ reconstruction with autogenous bone graft, and, more recently, alloplastic prostheses of the ramus and joint fossa, which have been the gold standard. However, joint prostheses’ cost is still too high for their wide use in public reference centers.2 Thus, this study aims to present a surgical case report in which TMJ arthroplasty was performed with the interposition of a temporal muscle flap as a feasible alternative.
Case Report
A 39-year-old Black male patient attended the public servisse of reference in oral and maxillofacial surgery in the metropolitan region of the state of Bahia, Brazil, for follow-up one month after suffering facial trauma in a motorcycle accident. Initial physical and tomographic examination revealed a complex fracture of the mandibular symphysis, with loss of bone fragment, associated with bilateral high condylar fractures, involving medial poles. Due to the time since the trauma, the patient presented some joint stiffness causing an anatomical reduction in mandible occlusion. The clinician started by performing osteosynthesis to reduce and fix symphysis fractures, treating the condyles conservatively.
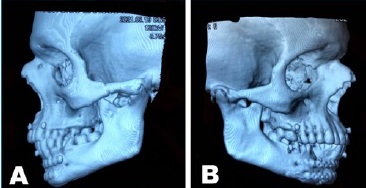
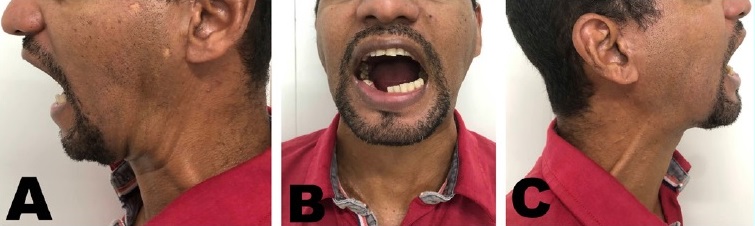
Eight months after the operation, the patient returned for an outpatient follow-up with complaints of pain in the TMJ region and difficulty with mouth opening. Physical examination revealed a limitation of about 10 mm of interincisal opening associated with dental malocclusion and a limitation of mandibular excursions (Figure 1). A new facial tomography showed bone fusion of the mandibular condyles with the glenoid cavity and bilateral TMJ ankylosis (Figure 2).
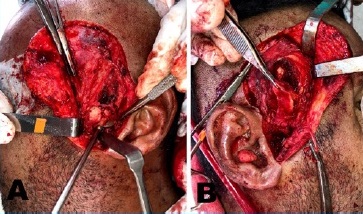
Based on clinical aspects, the clinician planned ankylotic block removal and interposition of a temporal flap. The procedure was performed in a surgical center under general anestesia and nasotracheal intubation. The Al-Kayat incision was employed to expose the TMJ region bilaterally for better exposure of the fused area and temporal musculature for rotation of the pedunculated flap (Figure 3).
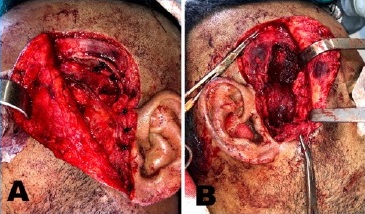
Low condylectomy was performed bilaterally using a Lindemann bur. A chisel and hammer were used to disconnect the condyle from the glenoid cavity. Then, reanatomization of the joint surface was performed with a multi-laminated bur. After condylar arthroplasty, muscular interposition of the pedunculated flap of the temporal muscle was conducted, filling the joint cavity, using Vicryl 3.0 for its fixation and covering the TMJ region, thus reducing the chances of recurrence (Figure 4).
During the execution of the technique, hemostasis was induced with electrocautery and ligation of the superficial temporal arteries. Abundant irrigation was applied with 0.9% saline solution. Layer-by-layer synthesis with Vicryl 4.0 was performed in the musculature, and 3.0 nylon was used for skin closure in the Al-Kayat incision. Compressive dressing was employed with gauze, micropore, and bandage and maintained for 48 hours.
The patient remained hospitalized in the unit until the third postoperative day (POD). During this period, he was on antibiotic therapy with Ceftriaxone 1g 12/12, analgesia, and venous anti-inflammatory. He was discharged on the fourth POD, with oral prescription. On the 15th POD, all skin sutures were removed, with no signs of inflammation. The patient maintained physical therapy, pain management medications, and active mobilization. At the 9-month follow-up, the patient was asymptomatic, with 23 mm of interincisal opening and no signs of recurrence (Figure 5).
Discussion and Conclusions
TMJ ankylosis is a pathology that modifies anatomy and function. It is generated by the growth of bone and fibrous tissues that cause a gradual loss of function.2 Patients affected by this process present limitations in mouth opening, mandibular hypomobility, and facial asymmetry, often characterized by deviation of the chin to the affected side.5,6In the present report, the patient had a severe opening limitation with a 12-mm interincisal distance, dental malocclusion, and limited mandibular excursions.
Among the classifications of ankylosis, the most commonly used divides the pathology into two groups: true ankylosis (intracapsular) and pseudoankylosis (extracapsular). The intracapsular type, as in the present case, involves the formation of fibrous and/or bone adhesions between the TMJ surfaces, with trauma and infections as the main etiological factors. The extracapsular type may originate from psychiatric, muscular, bone, and neurological disorders.5
Su-Gwan’s study reported that the etiology of 67.8% of ankylosis cases was related to trauma and 17% to some type of infection.7 In the present case, the patient developed bilateral intracapsular ankylosis with a bone fusion between the mandibular condyles and the glenoid cavity resulting from trauma to the chin region.
Regarding diagnosis, the literature suggests numerous complementary exams that can help, such as panoramic radiographs and frontal and axial views of the TMJ, which show loss of joint space and abnormal bone formation.
Computed tomography (CT) can also be used and provides a higher level of accuracy with a detailed rendering of hard tissues. Complementarily, especially in fibrous ankylosis, magnetic resonance can help diagnose and manage it, as well as soft-tissue window CT.5 Santos et al.6 stated that CT remains the gold standard for diagnosis, given its ability to detail imaging findings.
The treatment of ankylosis is imperatively surgical. The objective of the treatment is to release the joint by removing the ankylosed volume and remodeling the region as anatomically as possible, restoring functionality to the stomatognathic system.6 Several surgical techniques are used, such as simple gap arthroplasty, interpositional arthroplasty, reconstruction with alloplastic material, or even costochondral graft.6 The treatment of choice depends on some variables, including age.
Lima et al.4 report the case of a child patient who underwent arthroplasty in the gap due to the advantages of this auxiliary technique in the centrality of condylar growth, which is aimed in young patients. Treatment by costochondral graft has also been widely used, but its prognosis is unpredictable. Alloplastic materials or large prosthetic reconstructions should be indicated with caution in young people and children due to the incomplete growth of these patients.
In the presented case of an adult patient where prosthetic reconstruction was not available, the clinician opted for gap arthroplasty with temporal muscle interposition. This method has the main advantage of preventing impaired function and reducing the recurrence of bone fusion and consequent re-ankylosis.2 In addition, the use of the temporalis pedunculated muscle flap is beneficial because of its autogenous nature, good blood supply, and location close to the receptor bed.5,8,9
Among the alternatives to treat TMJ ankylosis, interpositional arthroplasty of the temporal muscle continues to be a feasible treatment option, due to its low recurrence rate, especially in adult patients, thus resulting in fewer postoperative complications and morbidities.