Introduction
Polymethylmethacrylate (PMMA) is the main component of the acrylic resins most used for removable denture bases due to its favorable characteristics: excellent aesthetics, low water absorption and solubility, absence of toxicity, repairability, simple manufacturing technique, and low cost.1-3 However, it also has limitations, such as possible hypersensitivity due to the residual monomer,1 aesthetics compromised by the possible presence of metal clasps,4 relatively low impact resistance, which results in a higher risk of fracture,5 and difficulty inserting/detaching the prosthesis for patients with low manual dexterity.
In recent years, the development of thermoplastic resins has gained relevance in oral rehabilitation using flexible dentures as an alternative to the conventional removable partial denture in PMMA.6 They provide greater patient comfort, greater retention, less need for dental modification, absence of residual monomer, and low elastic modulus (hence, greater impact resistance and lower risk of fracture).4,6However, achieving a satisfactory polish of these prostheses is challenging, resulting in a lower surface brightness than PMMA and greater susceptibility to pigmentation by extrinsic factors. Several complications associated with the need to rebase or repair this type of prosthesis have also been mentioned.4,7
The surface characteristics of denture-base materials can be decisive in the establishment and development of microbial plaque and its harmful consequences on oral health. In fact, some studies have demonstrated a direct relationship between surface roughness and Candida albicans (C. albicans) adhesion.8,9Although there is no consensus among authors, most report that more irregular surfaces facilitate microbial colonization by providing niches or spaces (which are frequente in the oral cavity) where microorganisms are protected from cleaning and displacement forces.10-15Moreover, increasing roughness also increases the physical surface area of adhesion, which benefits colonization.15 This greater presence of microorganisms favors the development of denture stomatitis, gingival inflammation, and caries in abutment teeth.10,16-18
Roughness may also affect the surface’s physical-chemical properties, such as wettability, measured by the contact angle.
Some authors state that wettability may be related to C. albicans adhesion, but there are inconsistent data for the effect of surface hydrophobicity on the initial adhesion of C. albicans to denture-base materials.11-14,18
More recently, thermoplastic materials such as polypropylene and polyolefin, exclusively based on hydrocarbon chemistry and without incorporated fibers, have been used for removable denture bases and tooth-colored retainers to improve aesthetics, patient comfort, and impact resistance. However, the surface characteristics of these materials and their influence on the materials’ behavior, namely concerning C. albicans adhesion, are still unclear.
The main objective of this in vitro research work is to evaluate the surface roughness, contact angle, and C. albicans adhesion in two thermoplastic (flexible) prosthesis materials - polypropylene and polyolefin - and compare them with PMMA.
Thus, the following null hypotheses were formulated: H01 - There are no statistically significant differences in roughness between the resins studied; H02 - There are no statistically significant differences in the contact angle between the resins studied; H03 - There are no statistically significant diferences in C. albicans adhesion between the resins studied.
Material and methods
For the study of roughness and contact angle, nine specimens were manufactured with dimensions of 5 mm × 40 mm × 65 mm, considering ISO 20795-1.19 A mold was designed in Solid- Works® (Dassault Systemes, France) and 3D printed by LASER stereolithography. This mold was included in a muffle adapted to the processing of each resin, guaranteeing the spacing inside. Thus, three specimens of each of the following materials were made: polymethylmethacrylate/PMMA (Millennium® - Keystone Industries, Gibbstown, NJ, USA), using compression techniques; and polypropylene (RocalFlex®, São Paulo, Brazil) and polyolefin (iFlex®, TCS Dental Inc., USA), produced by injection technique.
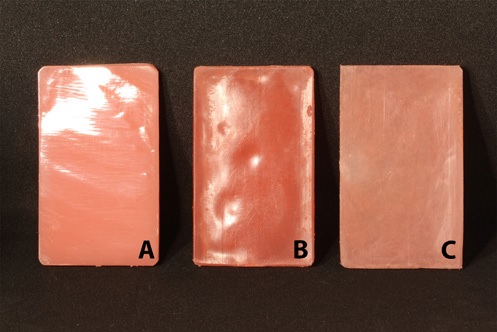
All specimens underwent conventional laboratory polishing according to the manufacturers’ instructions (Figure 1), executed by a single operator - an experienced prosthetic technician, to reduce variability related to the pressure applied during the procedure. The PMMA specimens’ surface was polished using a cloth polishing brush (ref 181-100-01, Dentaurus, Germany) mounted in a handpiece and a polishing stick for acrylics (ref 190-100-00, Dentaurus, Germany), followed by a cotton buff and the Acrylux paste (Rithuilium, Italy) to achieve the final brightness. Regarding the polyolefin specimens (TCS®), a brown rubber point (ref 4514-01) and a mini fuzz buff (ref. 4222-01) were used to finish and seal the surface; then, Polycril (ref. 4298-01) was applied with a turbo buff (ref. 4202-01) and Tripoli (ref. 4206-01) with a rag buff (ref. 4207-01), using continuous movements; finally, the iShine paste (ref. 4220-01) was applied using a rag buff on medium-high speed with very light pressure, until reaching a satisfactory appearance. The polypropylene specimens were polished with a medium grey acrylic polisher bur (ref. P 243 HM 10, Bredent, Germany) first, followed by the application of a pumice stone paste with a polishing brush at low speed; then, the same thermoplastic-resin polishing and a cotton buff were used.
The polished surface of all specimens in each group (n=3) was quantitatively evaluated using optical interferometry,20-22which provided the arithmetic mean roughness (Ra) and the maximum heights of the roughness profile (Rz).23-26 The 3D optical roughness meter NPFLEX (Bruker, Germany) was used for roughness reading at 1200 x 1200 measurement points per specimen. The contact angles of each material (n=3) were calculated with the optical tensiometer Contact Angle System OCA15 (DataPhysics Instruments, Germany), using the sessile drop method with distilled water,20,27 taking measurements at 10 to 25 locations of the specimens.
To study C. albicans adhesion, nine specimens measuring 5 mm x 4 mm x 4 mm were evaluated. These specimens were obtained from the central part of the previously made specimens (three of each material), using diamond disks at low rotation. They were then visually analyzed to ensure there were no deformations, and their lateral surface was carefully trimmed and smoothed with a scalpel and polishing bur at low speed. After preparation, the specimens were placed in an ultrasound bath (Sonorex, Bandelin), individually immersed in distilled water for four periods of 15 minutes, and sterilized by ultraviolet light (Biosafe 2 - Ehret, Germany; λ=250 nm) for 30 minutes.
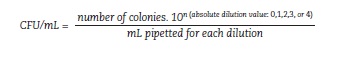
A fungal culture of C. albicans was previously performed for microbiological evaluation. The C. albicans biofilm was quantified through microbiological culture and measurement of CFU/mL (colony-forming units per milliliter). The yeast C. albicans ATCC 10231, obtained from the American Type Culture Collection (ATCC), was used. In an aseptic laminar flow chamber (Biosafe 2 - Ehret), nine specimens of each material (n=9) were distributed in 96-well cell culture plates. Then, 100 μL of the C. albicans suspension at 1x10 6 CFU/mL was added to the materials, and the plates were incubated at 37°C for 24 hours, shaking at 100 rpm (Heraeus Instruments), to allow biofilm formation. Afterward, the specimens were removed, washed twice with sterile phosphate-buffered saline (PBS) buffer, transferred to Eppendorf tubes containing 1 mL of PBS, and placed in an ultrasound bath (Sonorex, Bandelin) for 10 minutes to detach the adhered microorganisms. After vortexing each tube for 20 seconds, decimal dilutions of the respective supernatant were made. A 10-μL aliquot of each dilution was inoculated into Petri dishes containing Sabouraud dextrose agar (Liofilchem). The plates were incubated at 37°C for 24 hours. After the incubation period, the number of CFUs was counted using the following formula:
For all parameters evaluated, the results are presented as mean ± standard deviation (SD), median, minimum and maximum values, and interquartile range. Data were collected and stored in a database created using Excel® (Microsoft Office Plus Professional 2016, Microsoft, USA), and the statistical analysis was performed using the SPSS® v.28.0 software (Statistical Package for the Social Sciences, IBM, USA), considering a significance level of 0.05 (α=0.05). The Shapiro-Wilk test was used to test the normality of the distributions. The parametric ANOVA (Ra and contact angle) and the non-parametric Kruskal-Wallis (Rz and C. albicans adhesion) test and respective multiple comparisons (post-hoc Scheffe tests and Mann-Whitney U in combination with Bonferroni adjustment) were used to analyze the results between groups.
Results
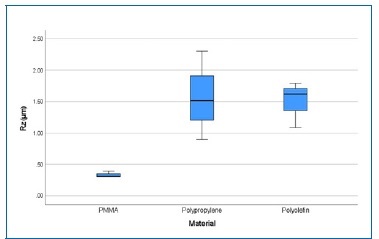
Table 1 shows the central and dispersion values, the minimum, and the maximum observed in each group for all variables studied: average roughness (Ra), maximum roughness (Rz), contact angle, and C. albicans adhesion. The 3D reconstruction of the polished specimens’ surfasse (Figure 2) showed differences in pattern, with evidently more uniform bands in the PMMA samples compared to the thermoplastic polymers under study. The groups of thermoplastic materials (polypropylene 0.15 ± 0.072 μm; polyolefin 0.15 ± 0.029 μm) had average Ra values higher than PMMA (0.03 ± 0.006 μm). Regarding Rz, the PMMA group had the lowest mean value (0.31 μm), and the polypropylene group had the highest (2.30 μm).
Table 1 Central and dispersion values, minimum, and maximum of the distribution of mean roughness (Ra), maximum roughness (Rz), contact angle, and C. albicans adhesion, per group.
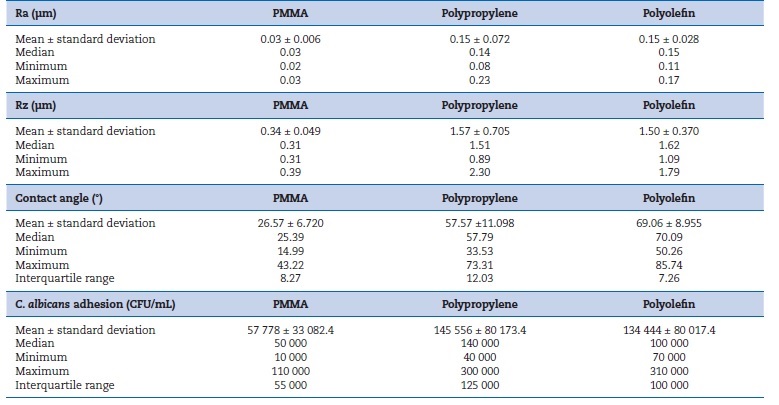
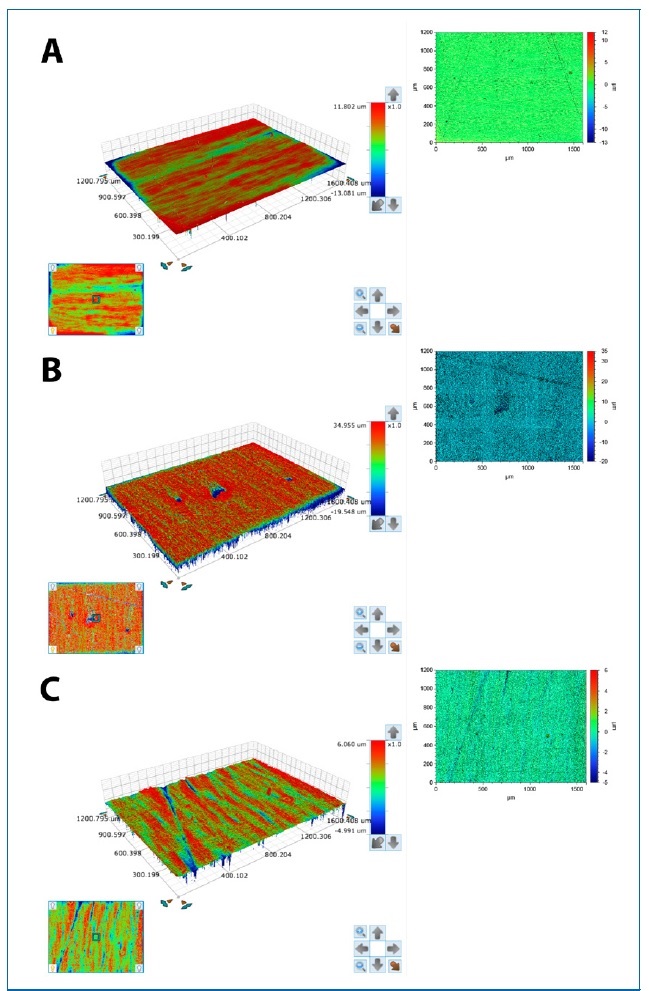
Figure 2 3D surface reconstruction of a polished specimen made of PMMA (A), polypropylene (B), and polyolefin (C).
The ANOVA test revealed statistically significant diferences for Ra between the means of the studied groups (p=0.027). The multiple comparisons between groups (Scheffe’s post-hoc test) showed statistically significant diferences between PMMA and polypropylene (p=0.045). No significant difference was found between polyolefin and PMMA (p=0.052), but the p=0.052 value was very close to the threshold for statistical significance (Figure 3). Concerning the Rz parameter (Figure 4), no statistically significant differences were found between the groups studied (non-parametric Kruskal-Wallis
test; p=0.066).
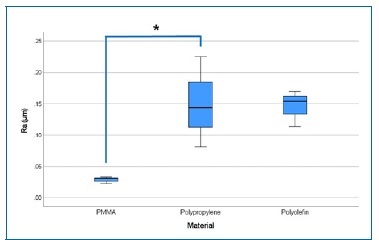
Figure 3 Arithmetic mean roughness (Ra) for each material. *p<0.05, ANOVA test, followed by Scheffe’s post-hoc test.
The average contact angle value for PMMA (26.57°±6.719) was much lower than that for thermoplastic resins, of which polyolefin registered the highest mean value (69.06°±8.955) (Figure 5). The ANOVA test and the post-hoc Scheffe test, performed to evaluate differences between the contact angles of the materials show significant differences (p<0.001) in the contact angle between the three groups (Figure 5).
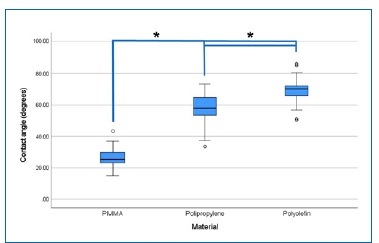
Figure 5 Contact angle (in degrees) for each material. *p<0.05, ANOVA test, followed by Scheffe’s post-hoc test.
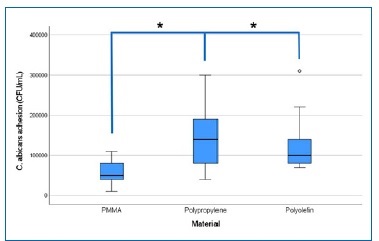
The non-parametric Kruskal-Wallis test indicated statistically significant differences in C. albicans adhesion between the different groups of materials (p=0.011). According to the Mann-Whitney U test in combination with the Bonferroni adjustment, there were statistically significant differences in C. albicans adhesion between the control group (PMMA) and polypropylene (p=0.007) and polyolefin (p=0.013), with the median being higher in the thermoplastic materials - polypropylene (140,000 CFU/mL) and polyolefin (100,000 CFU/mL) - compared to PMMA (50,000 CFU/mL). Accordingly, C. albicans shows higher adhesion in the thermoplastic resin groups (polypropylene and polyolefin) compared to the control group. There were no statistically significant differences in C. albicans adhesion between polyolefin and polypropylene (p=0.835; Figure 6).
Discussion
The characteristics of removable denture-base materials can be decisive in the establishment and development of microbial plaque and its harmful consequences on oral health. This investigation arises from the need to study the surface of those materials.
One of the most studied properties of denture-base materials is their roughness. Rough surfaces facilitate the pigmentation of the denture and can be a source of discomfort for the patient. On the other hand, several authors refer to the role of surfasse roughness in the initial microbial adhesion process as being positively correlated with the bacterial/fungal colonization rate of biomaterials.10,11,28 To minimize these problems, the denture bases are polished before their clinical use, aiming to produce a smooth and shiny surface by gradually removing rough layers from the surface, thus hindering microbial plaque formation.8,29
The surface roughness of the materials in this study was evaluated with an optical roughness meter. The Ra (average roughness) and Rz (maximum roughness) indicators were chosen for analysis because they are based on the roughness depth measurement and are the most used in the literature.
Furthermore, since these indicators provide average values, they are a good statistical parameter to characterize the amplitude distribution.30 In this study, after polishing all the specimens, the thermoplastic resins - polypropylene and polyolefin - showed a rougher surface than PMMA. The differences found between Ra values of PMMA and thermoplastic resins were probably due to the materials’ different physicochemical properties. It should be noted that the thermoplastic materials also had a high SD, which may be related to a lower surface homogeneity in the thermoplastic resin specimens. Thermoplastic materials have been associated with difficult finishing and polishing due to their low melting temperature, so a careful and minimal adjustment is recommended in these prostheses after processing.31
In several previous studies on C. albicans biofilm formation and adhesion to denture-base materials, the parameter chosen to represent the roughness was the average roughness (Ra).10,13,15,28,32-37The literature suggests a threshold for surfasse roughness of dental materials used in the oral cavity of Ra=0.2 μm, below which reduced microbial colonization is expected.11,38,39 After applying the polishing protocols to the diferente materials in this study, all the tested specimens presented a surface roughness below the limit of 0.2 μm, except for a polypropylene specimen whose mean Ra was 0.225 μm. Thus, it is assumed that, despite the statistically significant difference between PMMA and thermoplastic materials, the greater adhesion of C. albicans to these materials is not expected to be clinically significant.
Another parameter evaluated in the present study was the contact angle because it allows determining another fundamental feature of the surface of denture-base materials: hydrophobicity. Hydrophobicity is obtained by evaluating the wettability when a non-volatile liquid, such as water, comes into contact with a solid surface.40According to the literature, materials with a contact angle greater than 65º are considered very hydrophobic. Some authors consider that hydrophobic materials are more resistant to the action of water or water- soluble microorganism species.41-43 However, the relationship between the contact angle and bacterial adhesion is still controversial.41,44,45In this study, PMMA had the lowest average contact angle (26.57°), followed by polypropylene (57.57°) and polyolefin (69.06°). Polyolefin showed the worst wettability, corresponding to the highest hydrophobicity. The composition of the studied materials (as additives, cross-linking agents, fillers, and colorants) and the different polishing procedures may affect the hydrophobicity and surface free energy of denture base resins.45
Regarding C. albicans adhesion, the results of the presente investigation reveal differences between the materials studied, with superior adhesion in the thermoplastic materials - polyolefin and polypropylene - compared to PMMA. Certain surfasse properties of materials, such as roughness and wettability (quantified by the contact angle), can interfere with microbial colonization and biofilm maturation.11,46,47,48The initial adhesion of microorganisms is directly influenced by surface roughness, occurring more quickly on rough surfaces due to their larger contact area and obstruction of the mechanical cleaning action.49However, some studies did not find a relationship between C. albicans adhesion and the acrylic resin’s roughness.38,47,50
According to several authors, the ability of microorganisms to adhere to materials is related to the electrostatic force, which is more expressive on surfaces that present not only greater roughness, but also greater surface free energy.36,47,48,51
Other studies report a relationship between C. albicans adhesion to various surfaces with different surface roughness and surface free energy,41,44-46 which influences denture retention and contributes to the adherence, bonding, and colonization by fungal species. However, the direct relationship between these three factors (roughness, contact angle, and C. albicans adhesion) is not consensual.45
The present study found that the materials’ surface roughness, contact angle, and C. albicans adhesion to the material surface varied in the same direction. The results showed that surface roughness and contact angle were higher in thermoplastic materials compared to PMMA. C. albicans adhesion was also higher on these materials.
One of the limitations of this investigation was using specimens whose shape does not mimic a dental prosthesis. Also, it is important to emphasize that these materials’ polishing in clinical practice would be subject to other constraints. For example, the polishing of a prosthesis is not performed on completely flat surfaces, and a rotary polisher’s recommended speed and pressure are not always easy to standardize.1 Therefore, greater variability of Ra values can be expected in clinical practice. Variability between different operators can also occur, although this factor was minimized in this study by having a single operator.
The fact that water was used instead of saliva to determine the contact angle can also be considered a limitation of the study, although the inclusion of saliva would have brought many other possibly confounding factors to this study.52,53Even though saliva does not have the same characteristics in all individuals, using artificial saliva would have brought this assessment closer to the clinical reality.
Finally, this investigation was limited to the study of C. albicans adhesion and did not assess the importance of other microorganisms. Although C. albicans is a fungus of particular importance in various pathological situations of the oral cavity, namely denture stomatitis,16,17the biofilm that adheres to the surfaces of dental prostheses is composed of several microorganisms that interact and can actively intervene in the process of C. albicans adhesion to the denture.54,55
Conclusions
All the null hypotheses of this research work were rejected, given that:
• The surface roughness of the tested thermoplastic materials was higher than that of conventional PMMA;
• The contact angle values of thermoplastic materials were much higher than those of PMMA, suggesting that these materials are more hydrophobic;
• The C. albicans adhesion to the material’s surface was significantly higher in thermoplastic materials than in PMMA.
Under the conditions of this investigation, PMMA had lower roughness, lower contact angle, and lower C. albicans adhesion than polypropylene and polyolefin. Thus, it was confirmed as the first-choice material in the manufacture of removable resin dental prostheses.
Considering the possible association with a greater microbial proliferation in the salivary environment, the study of the surface of dental prosthesis base materials is clinically relevant. More studies should be performed to evaluate other conditions and different parameters.