Introduction
Ozone gas (O3), discovered in the mid-19th century,1 is a highly unstable and water-soluble inorganic molecule composed of three oxygen atoms.2 Once formed, O3 reacts with any electron donor, undergoes oxidation, and decomposes, resulting in an hydroxyl radical and a dioxide (O2) molecule.3 This reaction makes ozone a potent oxidant that can act as a precursor of free radicals both in vitro and in vivo.3 The principles attributed to this therapy’s efficiency are related to its capacity for balancing biological oxidative stress.3 When in contact with organic fluids, ozone leads to the formation of reactive oxygen molecules that influence cellular metabolism; thus, it is beneficial to tissue repair.3 In addition, ozone has importante antimicrobial properties,4 influences the cellular and humoral immune system, has anti-hypoxic effects, and activates the mechanisms of protein synthesis.5
Ozone therapy has been used and studied in several fields of health care.6,7In dentistry, some authors use ozone to assist the treatment of generalized chronic periodontitis,8,9in indirect dental pulp capping,10 in oral wound repair,11 in prosthesis-related traumatic ulcer pain relief,12 and as an adjunct in the treatment of periimplantitis13 and osteonecrosis of the jaws.3 This report aimed to present two cases of facial trauma,with extensive damage to the gingival tissues, in which ozone was used as supportive therapy to help with tissue repair.
Case reports
Case 1: The patient, a 40-year-old male victim of a motorcycle accident, was referred to the Clinical Hospital of the Federal University of Uberlândia. The patient denied having any allergies and comorbidities. Extraoral examination revealed significant edema and hematoma. During the intraoral examination, the patient presented craniocaudal and laterolateral mobility of the maxilla, avulsion of teeth 21 and 22, and gingival laceration in the anterior maxilla with bone exposure extending from teeth 11, 12, and 13. Initially, the intraoral lacerations were debrided and abundantly irrigated with 0.9% saline solution. A split flap was performed to cover the exposed bone, and sutures were made with 4.0 Monocryl.
A computed tomography (CT) scan confirmed the presence of Le Fort I fracture (Figure 1). Within 2 days after trauma, the fracture was reduced and fixed with 2.0-mm titanium plates retained with 5-mm screws. The postoperative medication administered was 500 mg Amoxicillin (every 8 hours for 7 days), 100 mg Nimesulide (every 12 hours for 3 days), and 500 mg Dipyrone Sodium (every 6 hours for 3 days).
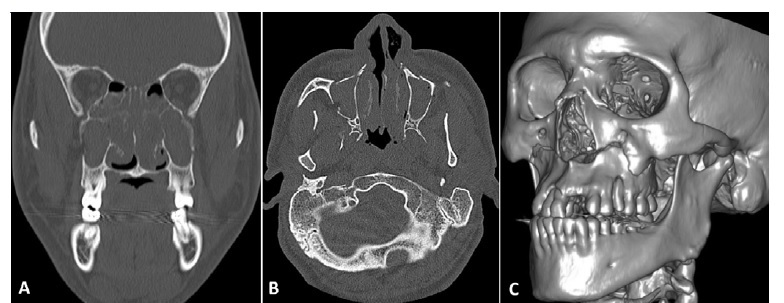
Figure 1 Case 1 - Computed tomography scan showing the Le Fort I fracture: (A) Coronal section; (B) Axial section; (C) Tridimensional reconstruction
In the immediate postoperative period, gingival ischemia was noted in the region between teeth 11 and 13. Weekly sessions of ozone were indicated until complete regression of the ischemic area and adequate tissue healing. Submucosal injection of 10 units of ozone gas at a concentration of 4 μg/ml was administered at four equidistant points, located 10 mm from the margins of the ischemic area. After this, the area was irrigated with 40 mL of ozonated water. The water was made in an ozone generator (Ozone Life, model O&L SS 2.0 Digital, São José dos Campos, São Paulo, Brazil) at a concentration of 40 μg/mL, resulting in ozonated water with a final concentration of 8 μg/mL. Daily hygiene with 0.9% saline solution was indicated.
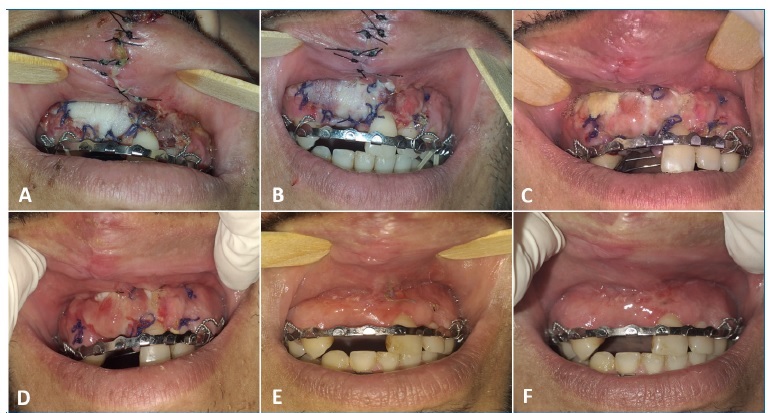
The patient was followed up for four weeks, and clinical improvement in the areas of ischemia was observed at each session (Figure 2). After 60 days, total healing and preservation of the gingival tissue had occurred.

Figure 2 Case 1 - Follow‑up of ozone therapy in the area of gingival ischemia between teeth 11 and 13. (A) Day 0; (B) Day 3; (C) Day 7; (D) Day 14; (E) Day 21; (F) Day 28
Case 2: The patient, a 36-year-old male victim of a motorcycle accident, was referred to the Clinical Hospital of the Federal University of Uberlândia. The patient denied having any allergies and comorbidities. Extraoral examination showed abrasions in the right mental (chin) region. During the intraoral examination, the patient showed changes in occlusion, craniocaudal and laterolateral maxillary mobility, upper lip laceration, and gingival laceration in the anterior maxillary region from teeth 13 to 22. The intraoral lacerations were sutured with 4.0 Vycryl.
The CT scan confirmed the presence of Le Fort I fracture (Figure 3). Within 3 days after trauma, the fracture was reduced and fixed with 2.0-mm titanium plates retained with 5-mm screws. The postoperative medication was the same as that prescribed for the previous case.
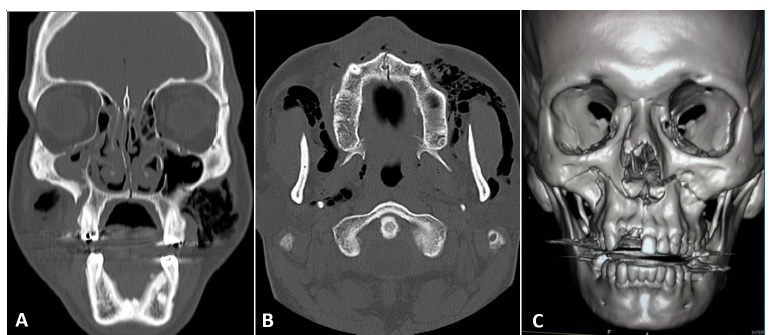
Figure 3 Case 2 - Computed tomography scan showing the Le Fort I fracture: (A) Coronal section; (B) Axial section; (C) Tridimensional reconstruction
In the immediate postoperative period, gingival ischemia was noted in the anterior region of the maxilla. Ozone was indicated, and the protocol followed the same specifications as in the previous case. The patient was followed up for five weeks, and clinical improvement was observed at each session (Figure 4). After 60 days, total healing and preservation of gingival tissue were observed.
Discussion and conclusions
Facial trauma may have clinical characteristics such as injuries to the soft tissues, bones, teeth, and scalp.14,15Fractures of the middle third of the face are relatively common, including Le Fort fractures. In both cases described in this report, the patients suffered avulsion of maxillary anterior teeth and extensive gingival lacerations as a result of trauma, which led to tissue ischemia.
The gingiva is part of the chewing mucosa that covers the alveolar process and surrounds the cervical portion of the teeth. Gingiva predominantly consists of connective tissue, and its main components are collagen fibers, fibroblasts, vessels, and nerves. Repair is a complex phenomenon that occurs to reconstruct disorganized or traumatized tissues, and it envolves cells16 and numerous chemical mediators.17 This perfect and coordinated cascade of cellular and molecular events results in an adequate reconstruction of injured tissue.18 The healing response can be divided into several phases: inflammation, reepithelization, granulation, tissue formation, matrix formation, and remodeling.19 Supportive therapies that favor restoration of the normal morphology and tissue repair would be interesting to use in several clinical situations.
In the present report, ozone gas and ozonated water were used as an adjuvant therapy to promote gingival and alveolar mucosa repair, and clinical improvement was observed right from the first application. Studies in the literature suggest that ozone acts to repair the acute phase of the wound through collagen synthesis and fibroblast proliferation. One of those studies evaluated the effects of a topical application of ozone gas on palatine gingival tissue repair in pigs. It was observed that ozone therapy could be effective in the early stages of repair with increased expression of the vascular endothelial growth factor.11 Other authors have found improved repair of guinea pig skin wounds after using topical ozonated olive oil.20 In an experimental study, a reduction in the amount of granulation tissue, lower number of inflammatory cells, and wider deposition of collagen type I were observed in Wistar rats with skin lesions that received 0.1 mL of subcutaneous ozone gas daily for 7 and 14 days.21 An in vitro study22 observed the inhibitory effects of ozone on nuclear factor kappa B (NF-κB) and suggested that ozone had anti-inflammatory capabilities.
In the early healing of unepithelized gingival grafts, the effect of ozone therapy has been shown to increase blood perfusion at the following time intervals: 1, 2, 3, 6, and 8 days postoperatively.23 In the present cases, the areas of ischemia in the gingiva decreased over weeks. Other studies have observed similar results, with a significant reduction in wound size and improvement in tissue quality after 1 week of ozone treatment.16 Isler et al.24 observed that topical ozone gas applied to palatal wounds provided faster reepithelization on day 14 than other treatment protocols.
In the present report, concentrations of 4 μg/ml ozone gas and 8 μg/ml ozonated water were used. Studies have shown that ozone concentrations of 10-40 μg/ml result in reepithelization and granulation, while concentrations above 80 μg/ml are cytotoxic and indicated for antimicrobial purposes.25 A randomized study26 of palate mucosa wounds in 30 patients using ozonated water (concentration 11-12 μg/ml) observed accelerated wound healing within the first 48 hours after treatment onset.
Although clinical studies have shown improvement in the repair process after ozone use, the literature still lacks quality scientific evidence about the role of ozone in the repair process of injured tissues.11 Recent clinical studies developed in medicine6,7and dentistry12,13have shown enhanced beneficial properties of ozone therapy. However, there are still few case reports in the literature worldwide.
Low ozone concentrations showed beneficial effects on the repair of ischemic wounds after trauma, with preservation of gingival tissue after treatment.