Introduction
Odontogenic keratocysts (OKC) originate from the odontogenic epithelium, particularly from dental lamina remnants, presenting different growth mechanisms and biological behavior than other maxillo‑mandibular complex cysts.1 This cystic lesion exhibits aggressive behavior with a high potential for infiltration in maxillary bones and may clinically present as a solitary lesion or in the form of multiple lesions. It may be associated to Gorlin‑Goltz syndrome (basal cell nevus syndrome); patients affected by this syndrome present developmental abnormalities, such as cerebral calcification, bifid ribs, and increased susceptibility to different neoplasms, like basal cell carcinomas.2
OKC presents a predilection for the mandible, and about 75% of all cases affect its posterior region.3 This type of lesion can be diagnosed at any age but affects mainly the third and fourth decades of life, mostly in males.1 Due to its potential for bone destruction, OKC often grows to large dimensions before causing bone expansion. It is usually asymptomatic, and the presence of a fluid or semi‑solid yellowish‑white content can be observed macroscopically.4
In 2005, OKC was classified by the World Health Organization (WHO) as a benign neoplasm originating from the odontogenic epithelium, thus justifying its aggressive behavior, and some studies have suggested an influence of PTCH1 gene alterations in its etiology.5 The current 2017 WHO classification again classified this lesion as an odontogenic developmental cyst, indicating that the PTCH1 gene is not specific for this lesion when presenting loss of heterozygosity in the 9q22.31 chromosome region and that these characteristics are also found in other developmental cysts, such as dentigerous cysts.6
Radiographically, lesions may have either a unilocular or multilocular aspect, according to their size, with sclerotic borders, and may or not be tooth‑ associated.2 Lesions involving the third molar crown result in a dentigerous cyst appearance.
Therefore, a conclusive diagnosis cannot be made preoperatively, based only on clinical and radiographic information, so histopathological examinations are important.3
Histopathologically, OKC is characterized by the presence of a pathological cavity lined by corrugated parakeratinized stratified squamous epithelium, with uniform thickness ranging from six to eight cell layers. The basal cells are columnar with palisaded nuclei, exhibiting nuclear hyperchromatism.
The interface with the surrounding connective tissue is flat, and a thin fibrous capsule is observed, as well as a mild inflammatory mononuclear infiltrate in some cases.7 Epithelial remains and satellite cysts can be found in the capsule, and these have been suggested as being responsible for OKC recurrence rates.8
Several treatment methods have been reported, from conservative to radical surgery. Enucleation and marsupialization are associated with a high number of recurrences. Associated therapies have been described as able to decrease the recurrence potential of OKC, such as peripheral osteotomy, Carnoy’s solution treatment, electrocauterization, cryotherapy, and surgical resection. Decompression and/or marsupialization present high success rates compared to aggressive treatments, preserving important structures like dental elements and nervous structures.7
The present study aimed to perform a retrospective clinical‑pathological study of cases diagnosed as OKC at the Oral Pathology Service of the Federal University of Rio Grande do Norte (UFRN) from 1970‑2018, and to assess recurrence rates and their clinical and radiographic features.
Material and methods
The study protocol was approved by the Ethics Committee of the Federal University of Rio Grande do Norte (UFRN) (Approval Number 1.998.353). The present cross‑ sectional study consisted of a retrospective analysis of OKC cases diagnosed between January 1970 and July 2018, archived in the Laboratory of Oral Pathology of the Department of Dentistry, UFRN, Rio Grande do Norte, Brazil. This service is one of the referral centers in oral and maxillofacial pathology in Brazil.
Data such as patient’s age and sex, OKC’s anatomical site, association with teeth and radiographical aspect (unilocular or multilocular), type of biopsy, symptomatology, and association with Gorlin syndrome were compiled for all cases from the clinical data sent with the biopsy records. For recurrent OKC cases, the time of relapse (in months) and the treatment modality were also evaluated. Regarding the inclusion and exclusion criteria, only cases histopathologically diagnosed as OKC were included. OKCs with no sufficient clinical data in the patients’ biopsy request forms were excluded. All selected cases exhibited the typical histopathological OKC characteristics, described by WHO in 2017, namely, an uninflamed fibrous wall lined by a folded, thin, regular parakeratinized epithelium 5‑8 cell layers thick, without rete ridges; the parakeratinized surface was corrugated, and the basal layer was well‑defined and often palisaded, with hyperchromatic nuclei and focal areas displaying reversed nuclear polarity.6
The data were tabulated and analyzed by descriptive statistics using the IBM SPSS Statistics program (version 20.0; IBM Corp., Armonk, NY, USA).
Results
A total of 15,670 cases of oral and maxillofacial lesions were recorded during the study period. Of these, 106 (0.67%) presented a histopathological diagnosis of OKC, including 92 cases (86.8%) with no recurrence and 14 cases (13.2%) with recurrence.
Concerning non‑recurrent OKC cases, a higher frequency was observed in women (n=48; 52.2%) (female:male ratio of 1.09:1), patients’ age ranged from 9 to 85 years old, with a mean of 34.3 years, and most patients had white skin (n=48; 52.2%).
Most cases occurred in the posterior region of the mandible (n=62; 67.4%), and 18 cases (19.6%) were associated with pain.
Unilocular lesions were slightly more frequent (n=20, 21.7%) than multilocular lesions (n=19; 20.7%), and association with teeth was evidenced in 14 cases (15.2%). Five cases (5.4%) were associated with Gorlin syndrome (Table 1).
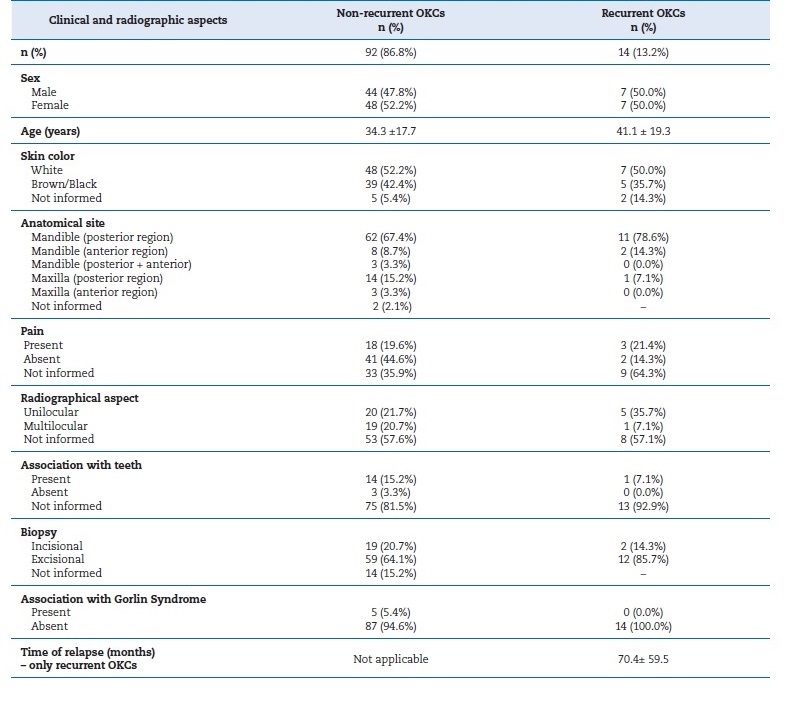
Table 1 Frequency of clinical and radiographic aspects of recurrent and non‑recurrent OKCs for a 48‑year‑period.
Among recurrent OKCs, a similar frequency between genders was noted, patients’ age ranged from 13 to 72 years, with a mean of 41.1 years, and half of the patients had white skin (n=7; 50.0%). The time of the relapse ranged from 8 to 168 months, with a mean of 70.4 } 59.5 months. Most cases occurred in the posterior region of the mandible (n=11; 78.6%), followed by the anterior region (n=2; 14.3%), and three cases (21.4%) were associated with pain.
Radiographically, five cases presented as a unilocular lesion (35.7%), and only one case was associated with teeth (7.1%). No case was associated with Gorlin syndrome. Regarding treatment during the first occurrence, prior to recurrence, two cases (14.3%) were treated conservatively, by decompression and enucleation, whereas four cases were treated by enucleation followed by ostectomy and use of Carnoy’s solution.
In eight cases (57.1%), no information about the treatment modality was available in the clinical record, and no satisfactory contact with the clinician was obtained.
Discussion
OKC is one of the most controversial oral and maxillofacial pathological entities. In contrast to other odontogenic lesions, OKCs are noted for their potentially aggressive clinical behavior, with a predisposition for local recurrence.9
Few studies evaluating recurrence rates and clinical OKC characteristics are available, with some studies indicating recurrence rate discrepancies.3,4,7In this retrospective analysis, recurrence was observed in 13.2% of the 106 cases histopathologically diagnosed as OKC, while 86.8% did not relapse.
According to a previous study,7 the presence of multiple OKCs in the craniofacial region and high recurrence rates are most often associated with Gorlin‑Goltz syndrome. In the present study, however, only 5.4% of all analyzed cases were associated with this syndrome, with no recurrence after the initial treatment. These findings differ from other studies in which syndromic cases presented an average recurrence rate of 35.4%.10 Multiple cystic lesions associated with this syndrome are often non‑synchronous, and recurrent lesions may be difficult to distinguish from new cases, appearing in contiguous, not initially detected, sites; also, a recurrence surcharge is probable.
In the present study, the frequency of non‑recurrent OKC cases presented a female‑to‑male ratio of 1.09:1, being slightly more frequent in women. The literature is inconclusive, as some authors have stated that OKC has a slight male predilection,1,3,4while others indicate a slight preference for females,2,3,11corroborating the findings reported herein.
The age at which patients are affected by OKC commonly ranges from the 2nd to 9th decades of life.1,2,8,9In the present study, the patients’ age in non‑recurrent OKCs ranged from 9 to 85 years old, with a mean of 34.3 years. These results are similar to others described in the literature,1,2,8indicating a wide age distribution of patients affected by OKC.4,5
OKC is one of the most common odontogenic lesions affecting the mandible, usually involving the mandible angle and branch.10 In the present study, most non‑recurrent OKCs were detected in the posterior region of the mandible, corresponding to 67.4% of all cases. Pain was reported in only 18 cases. OKC most often present as an asymptomatic lesion, unless a secondary infection is present.7,8 The anatomical site with the highest rate of recurrence observed in the present study was the posterior mandibular region, as observed in other reports.3,4,7,10
OKC development commonly occurs in the anteroposterior direction, without causing evident bone expansion, with its discovery being most often based on a radiographic finding.1,3
A unilocular or multilocular radiolucent lesion with well‑defined contours is observed in imaging examinations.12 In the present study, the frequency of unilocular lesions in non‑recurrent OKC cases was 21.7%, while multilocular lesions represented 20.7%. Minor lesions are prone to be unilocular, while larger lesions tend to be multilocular.13 These findings suggest that recurrence is partially related to the cystic lesion rate of aggression. Therefore, in cases of multilocular lesions, a more aggressive treatment is indicated.14
Recent multicentric studies have verified that 25 to 40% of OKC cases are associated with impacted tooth crowns. Thus, dental eruption failure is a clinically constant factor,1,3,4although several odontogenic cystic lesions also present these characteristics.11 In the present study, tooth association was observed in 15.2% of the non‑recurrent OKC cases and 7.1% of recurrent ones.
Regarding treatment at the initial occurrence, two cases were treated conservatively by decompression and enucleation, while four cases were treated by enucleation followed by ostectomy and Carnoy’s solution use. The literature indicates that decompression followed by surgical enucleation reduces the likelihood of recurrence and that decompression followed by enucleation is advantageous, especially in cases of extensive lesions,15,16,17 with fibrous capsule thickening observed in previous decompression procedures, facilitating complete surgical lesion removal.18,19,20
Although cross‑sectional studies with retrospective analysis represent important study methods for collecting clinical data, they present some limitations. The main limitation of this study is the inadequate completion of some clinical records that accompanied the specimens sent for histopathological examination, consequently omitting relevant information and impairing the observation of clinical data related to the studied lesions.
Conclusions
In conclusion, the clinical and radiographic profile of recurrent and non‑recurrent OKCs observed in this study agree with findings commonly reported in the literature, except for the lack of gender predilection. Regarding clinical characteristics, no gender predilection for isolated or recurrent OKCs was observed.
The lesions occurred mainly in adults, and the most common anatomical site was the posterior mandible, presenting mainly as a unilocular radiolucency lesion in both groups.
In addition, OKC displayed a 13.2% recurrence rate when conservatively treated by decompression and surgical enucleation.














