INTRODUCTION
Mouth Breathing (MB) is a common chronic pathological condition during childhood that modifies the breathing pattern of the upper airways and leads to adopting a breathing pattern complemented by the oral route (Felcar, Bueno, Massan, Torezan & Cardoso, 2010; Inada et al., 2022). The breathing pattern of mouth breathing overloads the tonsils and larynx and, as a consequence, triggers functional, structural, pathological, postural, occlusive, and behavioural alterations (Campanha, Freire & Fontes, 2008; Okuro et al., 2011a). In addition, Uhlig, Marchesi, Duarte, and Araújo (2015) reported that adaptations caused by mouth breathing could be associated with mouth breather's quality of life.
Due to respiratory distress caused by MB, the body makes adaptations in its positions to facilitate the entry of air into the lungs (Okuro et al., 2011a). These adaptations produce compensatory muscular and skeletal actions in a way that mouth breathers project the head and extend the neck to increase the passage of air through the pharynx, reducing upper airway resistance (Sabatucci, Mastrovincenzo, Luchetta, Giannone & Ciavarella, 2015). Forward head posture leads to changes in the positions of the trunk and spine, such as loss of cervical lordosis, dorsal kyphosis, winged scapula, shoulders protrusion, abdominal protrusion (Okuro et al., 2011a) and knee position (Roggia, Santos Filha, Correa & Rossi, 2016). These factors lead to muscle shortening and alterations in the skeletal biomechanics, contributing to the disorganisation of the other muscles with their insertions and origins in the same structure. As a consequence, the cascading effect on posture and muscular imbalance are triggered (Okuro et al., 2011b; Silveira, Mello, Guimarães & Menezes, 2010).
Such changes reinforce the need to perform postural and respiratory reeducation exercises to reduce postural imbalances and maintain an adequate breathing pattern. Exercises for unblocking the thoracic spine are recommended to improve ventilatory mechanics, as they aim at respiratory reeducation with emphasis on the abdominal and diaphragmatic work (Teixeira, 2008). In addition, proprioceptive exercises are indicated for postural reeducation, specifically those that stretch and strengthen the muscle groups responsible for posture maintenance. They promote alignment of the vertebral segments and prevent frequent postural changes stemming from MB (Silva, Held, Sampaio, Di Lorenzo & Costa, 2007).
Given that, an average of 55 to 60% of school-age children are mouth breathers (Abreu, Rocha, Lamounier & Guerra, 2008; Felcar et al., 2010) and that the changes resulting from physical exercises are easier to see in younger individuals as body features are still under development (Teixeira, 2008) in this period, it is fundamental to disclose to parents and health professionals, exercise programs that are effective in postural and respiratory reeducation of children and adolescents. Indeed, López and Isasi (2019) reported low knowledge of parents/guardians regarding mouth breathing and its clinical manifestation. Despite the important benefits that physical exercise brings about for mouth breathers, there is no consensus on which is the best model of an exercise program for this group. Thus, the objective of this study was to conduct a systematic review to investigate the effect of different physical exercise programs on the posture of MB children and adolescents.
METHODS
The search strategies of this systematic review, as well as the methods of analysis and inclusion criteria, were specified and documented in a protocol (CRD42019124155 — PROSPERO). The search for studies focused on the effect of physical exercise on the body posture of MB children was carried out in the following electronic databases: Scopus, PubMed, Lilacs, Bireme, and Scielo. The selection of the descriptors was based on terms indexed in the Medical Subject Headings (MeSH) and included the following keywords in English: mouth breather, mouth breathing, nasal obstruction and exercise(s). These keywords were combined using boolean operators (“OR” and “AND”) and adapted to each database.
The studies were evaluated regarding aspects related to the effect of physical exercise on the posture of MB children and adolescents. The eligibility of these papers was determined independently by two assessors, who subsequently met to reach a consensus. A third assessor was consulted when there was a divergence in the results.
Inclusion and exclusion criteria
The following inclusion criteria were applied: articles published in a peer-reviewed journal; observational studies (controlled, cross-sectional, longitudinal prospective or retrospective) on the subject; that measured the body posture; not targeted to groups with other respiratory pathologies; focused on children and/or adolescents; that approached exercise programs and postural reeducation for mouth breathers; published in Portuguese or English; carried until November 2022. There was no restriction to the initial year of publication since the aim was to consider a broad overview of the subject.
Among the exclusion criteria were studies that presented insufficient results, not full text available, and studies that were conference publications, scientific events summaries, final papers, literature reviews, commentaries or editorials. Studies that were not directly related to the main objective of the present study and those which had a sample that did not correspond to the age range defined for this study were also excluded.
Methodological quality assessment
The selected studies were analysed for their methodological quality using the PEDro scale (Morton, 2009). The PEDRo scale evaluates, based on 11 items, the quality of these studies and whether the criteria of a clinical trial in ideal conditions were followed. Item 5, which verifies the blind participation of the subjects in a study, was not applied since it cannot be scored in experimental studies that include interventions with physical exercise programs once it is not possible to blind subjects for the exercises. Hence, in this study, the maximum score on the scale was 10 points, which means that the higher the score on the scale, the higher the quality of the study.
The quality analysis of the studies was carried out by two independent assessors, and disagreements between them were discussed in consensus meetings. After the methodological assessment, the outcomes and results of the studies were analysed and grouped into topics for comparison and discussion.
RESULTS
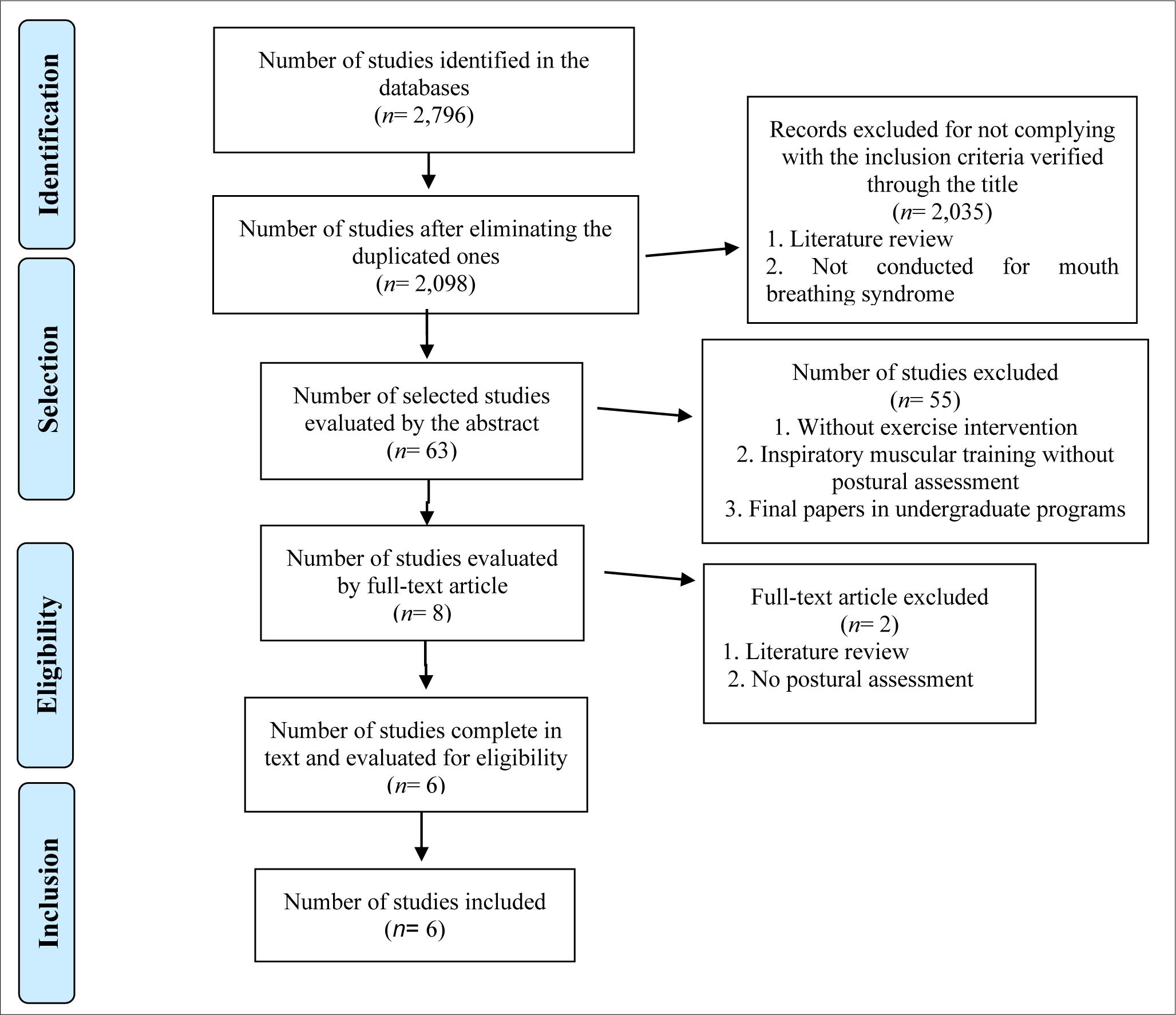
The search in the databases found a total of 2,796 studies. After checking for repeated studies, the articles were primarily selected by analysis according to the title/abstract, then by reading the full article and applying the proposed criteria and objectives of the study. As a final result, 6 papers were included in the review. Figure 1 shows the flowchart of the steps for the selection of the papers.
Methodological quality
The score of the methodological quality scale of the selected studies scale is presented in Table 1. The mean score was 5.5 (5-7) points on a scale of 0 to 10.
Table 1. Methodological quality of the analyzed studies.
| References | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Corrêa and Bérzin (2007) | 1 | 0 | 0 | 0 | - | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Corrêa and Bérzin (2008) | 1 | 0 | 0 | 0 | - | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Ferreira et al. (2012) | 1 | 0 | 0 | 0 | - | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Rezende et al. (2016) | 1 | 0 | 0 | 0 | - | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Schivinski et al. (2011) | 1 | 0 | 0 | 0 | - | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Weber et al. (2012) | 1 | 0 | 0 | 0 | - | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
Location and characteristics of participants
All the selected studies were carried out in Brazil (Corrêa & Bérzin 2007, 2008; Ferreira et al., 2012; Rezende, Carvalho, Phelipe, Rocha & Iunes, 2016; Weber, Corrêa, Ferreira, Milanesi & Trevisan, 2012). Subjects were recruited at public schools through speech therapy (Corrêa & Bérzin 2007, 2008) or specialised health service demands (Ferreira et al., 2012; Rezende et al., 2016; Weber et al., 2012). The diagnosis of mouth breathing was confirmed by examination of upper airway obstruction (13.14) or by otorhinolaryngological (Ferreira et al., 2012; Weber et al., 2012) and dental diagnosis (Rezende et al., 2016). Participants were between 7 and 17 years old, totalising 87 subjects in all the selected studies (55% male). The characteristics of participants, measuring instruments, and interventions are summarised in Table 2.
Table 2. Summary of characteristics of the studies included in the review.
| Author, year/country | Sample characteristics | Evaluation instruments | Intervention |
|---|---|---|---|
| Corrêa and Bérzin (2007)/Brazil | 19 children (11 male and 8 female) 10.6± 1 years old |
Postural assessment: computerized image analysis Bilateral EMG of the sternocleidomastoid, suboccipital and upper trapezius muscles |
12 weeks, 2x/week/30min Therapeutic exercises with a Swiss ball and diaphragmatic breathing re- education. Proprioceptive neuromuscular facilitation Stretching and strengthening of the stabilizer muscles in the spine |
| Corrêa and Bérzin (2008)/Brazil | 19 children (11 male and 8 female) 10.6± 1 years old |
Bilateral EMG of the sternocleidomastoid, suboccipital and upper trapezius muscles during inspiration | 12 weeks, 2x/week/30min Therapeutic exercises with a Swiss ball and diaphragmatic breathing re- education Proprioceptive neuromuscular facilitation Stretching and strengthening of the stabilizer muscles in the spine |
| Ferreira et al. (2012)/Brazil | 10 children (6 male and 4 female) 10± 2.1 years old |
Biophotogrammetric postural assessment - SAPO software Maximal inspiratory (MIP) and expiratory pressure (MEP), inspiratory capacity (IC), Peak Expiratory Flow (PEF) and chest and abdominal wall mobility |
10 weeks, 2x/week/60min Muscle stretching and strengthening. Swiss ball, diaphragmatic stimulation, and stretching of the accessory muscles of inspiration |
| Weber et al. (2012)/Brazil | 12 children (6 male and 6 female) 10± 1.8 years old |
Craniocervical postural assessment – SAPO software | 10 weeks, 1x/week/60min Therapeutic exercises with a Swiss ball and diaphragmatic breathing re- education. Proprioceptive neuromuscular facilitation Stretching and strengthening of stabilizer muscles in the spine |
| Schivinski et al. (2011)/Brazil | 10 children (5 male and 5 female) 10.2± 2.65 years old |
Postural assessment: New York method Chest and abdominal mobility measurements Respiratory pattern: measurements |
24 weeks, 2x/week Intervention with kinesiotherapy muscle stretching and strengthening exercises Swiss ball, elastic bands, GPR, Isostretching, Klapp, and Pompage |
| Rezende et al. (2016)/Brazil | 17 children (9 male and 8 female) 11.64± 3.75 years old |
Postural assessment: photogrammetry Respiratory pattern: measurements |
12 weeks, 1x/week Intervention with isostretching exercises |
Characteristics of interventions
The protocols of the exercise programs differ among the studies. In four studies, strengthening exercises, muscle stretching, and diaphragmatic respiratory reeducation were performed (Corrêa & Bérzin 2007, 2008; Ferreira et al., 2012; Weber et al., 2012), while in the other two, only muscle strengthening and muscle stretching exercises were performed (Ferreira et al., 2012; Rezende et al., 2016). The duration of the interventions varied between 10 (Ferreira et al., 2012; Weber et al., 2012), 12 (Corrêa & Bérzin 2007, 2008; Rezende et al., 2016) and 24 (Ferreira et al., 2012) weeks. The weekly frequency of the exercise programs was one (Ferreira et al., 2012; Rezende et al., 2016; Weber et al., 2012) and two (Corrêa & Bérzin 2007, 2008; Ferreira et al., 2012) weekly sessions.
Details on exercise control and intensity were not recorded in any of the studies. In addition, none of the studies presented a control group.
Evaluation instruments
The postural assessment protocols differed among the studies (Table 2). They used either computerised image analysis (Corrêa & Bérzin, 2007), biophotogrammetric analysis (Ferreira et al., 2012; Rezende et al., 2016; Weber et al., 2012), the New York method (Ferreira et al., 2012) or electromyographic activity of the accessory muscles of breathing (Corrêa & Bérzin, 2008). The breathing pattern was evaluated in 3 studies (Ferreira et al., 2012; Rezende et al. 2016), either by measurements (Rezende et al., 2016) and by manovacuometer (Ferreira et al., 2012). The assessment procedures were performed before and at the end of the exercise sessions.
Effects of the intervention
All studies showed an improvement in body posture after the exercise program, despite the difference in methods of postural assessment and exercise programs. Corrêa and Berzin (2007) observed a reduction in forward head posture (p= .003) and winged scapula (p= .04) after intervention; Ferreira et al. (2012) found a reduction in the values measured by the biophotogrammetric analysis of the Charpy angle (angle between the xiphoid process and lower angle of the last ribs) (p= .04); Rezende et al. (2016) detected alteration in the angles of the sternoclavicular joint (p= .003), anterior superior iliac spine (p= .001) and superior posterior iliac spine (p= .009); Schivinski et al. (2011) observed an increase in the score of evaluation of the New York method for postural assessment (p= .005); and Weber et al. (2012) found a reduction in forward head posture (p= .001) and the restore of the cervical curve (p= .01). All these results characterise an improvement in the postural pattern.
Concerning the breathing pattern, Corrêa and Berzin (2007) showed a reduction (p< .05) in electrical activity on the assessed muscles during quiet stance position and aligned posture after the intervention. Corrêa and Berzin (2008) found a reduction (p< .01) in the electromyographic activity during nasal inspiration in all assessed muscles. Ferreira et al. (2012) observed an increase in the inspiratory capacity (p= .05), a reduction in maximal inspiratory pressure (p= .02) and a reduction in the xiphoid respiratory coefficient (p= .03). Rezende et al. (2016) found an increase in maximal expiratory pressure (p= .001). Schivinski et al. (2011) observed a reduction in the measurement of the expiratory xiphoid and an alteration in the breathing pattern (initially, 70% of the school children had chest breathing, 20% mixed, and 10% abdominal breathing. After the sessions, the ratios changed to 50% chest and 50% mixed breathing). Details of the results are shown in Table 3.
Table 3. Summary of results in the studies.
| Author, year/country | Results |
|---|---|
| Corrêa and Bérzin (2007)/Brazil |
Postural assessment: ↓ angle: plumb bob and ear lobe and prominence of scapula ↑ angle: manubrium and left shoulder ↓ angle: lower angle of scapula and C7 ↓ Decreased activity of cervical muscles |
| Corrêa and Bérzin (2008)/Brazil |
Postural assessment: ↓ Sternocleidomastoid activity ↓ Suboccipital activity ↓ Upper trapezius activity |
| Ferreira et al. (2012)/Brazil |
Postural assessment: ↓ values assessed for the Charpy angle (p= .04). Breathing assessment: ↑ of inspiratory capacity (p= .05) and reduction of the xiphoid respiratory coefficient (p= .03) |
| Weber et al. (2012)/Brazil |
Postural assessment: ↓ of forward head posture (p= .001) and restore of the cervical curve (p= .01) |
| Schivinski et al. (2011)/Brazil |
Postural assessment: ↓ The protrusion, shoulder rotation, and dorsal kyphosis ↓ Uneven hip lines ↑ Normal posture ↓ Xiphoid measurement during expiration ↑ Mixed breathing pattern ↑ Mobility of the xiphoid region ↑ Axillary region mobility |
| Rezende et al. (2016)/Brazil |
Postural assessment: The decrease in the angle of the sternoclavicular joint (p= .003) |
DISCUSSION
The objective of this review was to verify the effect of different exercise programs to correct postural imbalances in children and adolescents with Mouth Breathing Syndrome. Although previous data have shown that different devices had a positive effect on the breathing pattern in mouth breathers (Fonsêca et al., 2022), interventions with physical exercises can interrupt the progressive worsening of the condition, both in breathing pattern and in muscular and skeletal factors, which reduces the evolution of postural imbalances (Silveira et al., 2010). However, few studies have investigated the effects of physical exercise interventions on MBS (Barbiero, Vanderlei, Nascimento, Costa & Scalabrim Neto, 2007), despite their beneficial effects on overall body function (Ferreira et al., 2012). The main finding of this study was that the stretching of shortened muscles and the strengthening of stabiliser muscles of the spine resulted in the reduction of postural imbalances in mouth breathers. Also, respiratory correction techniques, such as diaphragmatic breathing reeducation and stimulation and stretching of the accessory muscles of inspiration, positively influenced the body pattern of mouth-breathing children.
MBS is a common syndrome that can be caused by lip seal and diseases of the nose (Inada et al., 2022) and affected mainly children who are growing and developing posture patterns. The most frequent postural alterations during this period are forward head posture and protruding abdomen (Meereis et al., 2013). These postural alterations can lead to reduced contraction capacity, shortening, and atrophy of the muscles. In the present study, it was observed that the exercises programs to increase muscular balance through the use of techniques of Global Postural Reeducation (Ferreira et al., 2012) and proprioceptive neuromuscular facilitation (Corrêa & Bérzin, 2007; Weber et al., 2012) had beneficial effects in the postural reeducation of MBS. Once Global Postural Reeducation is a method appropriate for correcting postural deviations and breathing control, muscular stretching provides an increase in muscle length, improvement in the range of movements, flexibility and, consequently, improves the contraction capacity of the affected muscles (Souchard, 2005; Teodori, Negri, Cruz & Marques, 2011). Therefore, muscular stretching may have reduced the muscular atrophy generated by MBS. For that reason, it was proven effective in the increase of muscular and postural balance.
In addition to the reeducation of body posture, physical exercise was also effective on respiratory function. After all, one of the implications of mouth breathing is the reduction of ventilatory muscle strength, probably due to postural alterations developed (Okuro et al., 2011b). In the present study, improvement of breathing pattern was observed both in studies that performed specific exercises of ventilatory diaphragmatic reeducation (Corrêa & Bérzin 2007, 2008; Ferreira et al., 2012; Weber et al., 2012) and in studies that did not perform them (Ferreira et al., 2012; Rezende et al., 2016). Moreno, Silva, Zuttin and Gonçalves (2009) observed an increase in inspiratory and expiratory muscle strength and chest mobility of young and sedentary women after a 4-week program using proprioceptive neuromuscular facilitation techniques. These findings corroborate with the present study, which could indicate that postural reeducation performed as the sole form of treatment can bring benefits to the breathing pattern, even without specific training, since some muscle groups also act as an accessory to breathing, in addition to maintaining the position of limbs and posture. However, it is worth noting that the association between postural and breathing exercises promote additional gains in respiratory function (Ries et al., 2016).
Although the studies included in the present study did not present the control of the intensity of the exercises, it was observed that muscular stretching and strengthening exercises (conducted at a minimum frequency of a weekly session, in a period equal to or greater than 10 weeks), using different techniques, with or without the use of materials, were sufficient to promote adaptations in the posture of children and adolescents with MBS.
As a limitation of the present study, the methodological quality of the analysed studies can be indicated. Although selection criteria were applied according to the Pedro scale, in which the studies showed a minimum score of 5 points, no study used a control group. The control group is essential to compare the effect of the intervention and, above all, to guarantee the reliability of the parameters used in the evaluation of these effects. However, all studies showed significant results for the postural control variables compared to the period before the training programs, which may indicate their effectiveness.
CONCLUSIONS
Although it is difficult to compare studies and establish guidelines for the formulation of an exercise protocol, it can be observed that muscular stretching and strengthening exercises, particularly of the stabiliser muscles of the spine, were the most frequent intervention. The minimum weekly workout frequency, in a period equal to or greater than 10 weeks, may be effective in improving the body posture of children and adolescents with MBS. Taking into account the high prevalence of MBS in children and adolescents and its consequences for posture, physical educators and physiotherapists should consider the combination of breathing and postural exercises in physical interventions for this population. For some reason not understood yet, the results showed studies only carried out in Brazil. Thus, new research is encouraged in order to investigate the effect of physical exercise programs on the posture of mouth breathers conducted around the world.