INTRODUCTION
Postural balance is a complex process involving coordinated actions of biomechanical, sensory, and neuromotor components. Their maintenance occurs through dynamic interaction of visual, vestibular, and somatosensory systems to adjust postural sway (Winter, 2009). A low ability to maintain postural balance is associated with an increased risk of falling as well as concerns and worries about falling among older adults (Rossat et al., 2010). In fact, a previous study by Davis, Campbell, Adkin, and Carpenter (2009) pointed out a significant and independent association between balance-related outcomes and concerns about falling. Therefore, preventive strategies that might improve postural balance and mitigate concerns about falling can potentially boost or even promote autonomy and health-related quality of life during ageing (Kendrick et al., 2014; Sherrington et al., 2020).
In this line, progressive resistance training (PRT) represents an effective exercise-based approach to foster significant health benefits in older adults, including muscular strength and mass gains, and improvement in functional capacity and executive function, all variables related to postural control and fall-related outcomes (Howe, Rochester, Neil, Skelton, & Ballinger, 2011; Mcleod, Stokes, & Phillips, 2019; Cavalcante et al., 2020; Santos et al., 2020). However, in light of the current literature, the effectiveness of PRT on postural balance and concerns about falling is still unresolved.
For example, a systematic review led by Howe et al. (2011), aimed to investigate the effects of exercise training in older adults, showed (sub-analysis of 21 studies) moderate effect sizes in favour of resistance exercise in several measures of static [unipodal static balance with eyes open (+3.88 seconds; 95%CI −0.53; 8.28), and closed (+1.64; 95%CI 0.97; 2.31)], and dynamic balance [Berg scale (-5.50; 95%CI −20.70; 9.72). Conversely, when it comes to more accurate measurements, a meta-analysis conducted by Low, Walsh, and Arkesteijn (2017), which included only studies that used the centre of pressure (CoP) measures through a force platform, did not demonstrate significant alterations in balance after resistance-based exercise programs.
Regarding concerns about falling, Kendrick et al. (2014) demonstrated that interventions with resistance exercise did not improve this outcome. However, it is worth noting that these results should be carefully analyzed since the study provided “very low” and “low” quality of evidence, suggesting the information on this issue is still insufficient to support robust evidence. Another point that should be mentioned is that the exercise protocols of the studies summarized in these three metanalyses used single-joint muscle groups; overload using elastic bands or bodyweight without proper progression and supervision (Howe et al., 2011); resistance exercises in the water or vibration platform protocols (Low et al., 2017) as well as multicomponent exercises or walking with overload programs (Kendrick et al., 2014).
While there is a range of resistance exercise prescription possibilities, the basic principle governing the training program design (i.e., progressive overload with whole-body prescription exercises) cannot be overlooked. This occurred in most of the previously mentioned studies intervention protocols and could have influenced training-induced adaptations. Thus, our study aimed to analyze the effects of a PRT intervention on both postural balance and concerns about falling outcomes in healthy older adults. It was hypothesized that the intervention with PRT with exercises for the whole body, which was supervised and followed the principle of progressive overload, could induce postural balance gains and mitigate concerns and worries about falling.
METHODS
Study design
This study was a randomized controlled trial of parallel groups with evaluations at baseline and on completion of the intervention and took place for 12-weeks. The study was approved by the local research ethical review board and registered in the Brazilian Clinical Trials platform (protocol: RBR-9djpfc). All participants signed an informed consent form prior to baseline assessments. The reporting of the study followed the CONSORT guidelines extension for non-pharmacological therapies (Boutron et al., 2017).
Participants and study eligibility
Male and female older adults were recruited through local advertising, social media, email invitations, direct contact with participants from previous studies, health services, community programs, and verbal communication. Participants were eligible if they met the following criteria:
aged 60 or older;
not having performed structured exercise such as aerobic and resistance training in the previous six months;
no clinical conditions or unstable diseases that contraindicate the exercise training protocol, based on the decision of a cardiologist (i.e. symptomatic ischemic heart disease or acute stroke);
no previously diagnosed cerebrovascular, neurological, or psychiatric disease (self-reported);
sufficient visual and hearing capacity (self-reported); and vi) women could not be under hormone replacement therapy.
Randomization, blinding and sample size
Participants were randomly assigned into a control or PRT intervention group in a 1:1 fashion using a random sequence, stratified by sex and age, through a computer-generated randomization code. To ensure concealment of allocation, randomization sequences were performed remotely at the end of the baseline assessments by an independent blinded researcher with no clinical involvement in the trial.
Our sample calculation was based on an 80% probability of detecting an effect size of 0.18 (Kendrick et al., 2014) in the concern about falling outcome an alpha of 5%, and a correlation of 0.7 between measures using a within-between interaction approach, demonstrating a minimum sample required of 40 participants. However, considering a dropout rate of 15% during the follow-up, the final sample size was 46 participants (23 per group). We used GPower software 3.1.9.2 (Universität Düsseldorf, Germany),
Intervention groups
Progressive resistance training
Participants randomly assigned to the progressive resistance training (PRT) group performed three sessions per week of supervised resistance exercise, during 12-weeks, following the recommendations for PRT for older adults (Borde, Hortobágyi, & Granacher, 2015). The training program was composed of nine whole-body exercises: vertical chest press (pectoralis major), horizontal leg press (quadriceps, hamstrings, glutes and hip adductors), seated row (trapezius, latissimus dorsi and deltoids.), knee extension (rectus femoris and vastus medialis, vastus lateralis and vastus intermedius), barbell curl (brachial and brachioradial biceps), seated leg curl (semitendinosus, semimembranosus and biceps femoris), triceps pushdown (triceps braquial), standing calf raises (gastrocnemius and soleus), and sit-ups (rectus abdominis, external and internal obliques). All sessions were performed three times per week (Mondays, Wednesdays, and Fridays) at the same time of the day (8:00 to 10:00 a.m.).
The prescription was set on three fixed sets and repetitions ranging from 10-15 repetition maximum (RM), and the recovery interval between the sets and exercises ranged from 60 to 120 seconds. The average duration of each training session ranged from 50-60 minutes. The familiarization with the training program occurred in the first training sessions with light loads. Then, loads of each exercise were adjusted according to the participant's ability and improvement in exercise capacity throughout the training protocol to ensure that they were exercising with as much resistance as possible while maintaining proper exercise form and a full range of motion. Progression for PRT was planned when the upper limits of the target repetition zone were completed for the three sets for three consecutive training sessions. Subsequently, in the next session, the load was increased 2–5% for the upper limb exercises and 5–10% for the lower limb exercises. All exercise sessions were supervised by certified exercise instructors (ratio of 1 instructor to each 2-3 participants).
Control group
Participants assigned to the control group were asked to maintain their habitual lifestyle, and no supervised exercise program was offered during the 12-week intervention. However, free resistance exercise classes were offered to these participants for three months at the end of the trial.
Descriptive variables
General and clinical measures including age (years), stature (meters), body mass (kg), body mass index (kg/m²), education level (years), and medical history (i.e., hypertension, diabetes, cardiovascular, and neurological disease) were obtained. Global cognitive function was assessed using the Brazilian version of the Montreal Cognitive Assessment (MoCA) (Memória, Yassuda, Nakano, & Forlenza, 2013).
Dependent variables
Postural balance
A biomechanics force platform (Model OR6-7, 3.05, AMTI, USA) was used to assess the static postural balance of participants. The equipment contains four load cells arranged evenly below the platform, enabling measurements of the centre of pressure (CoP) using the anteroposterior and medio-lateral axes force components at a sampling frequency of 1,000 Hz, low-pass filtered (2nd order, zero-phase-lag, Butterworth, 5 Hz cut-off frequency), and transformed to obtain CoP values. In the present study, the parameters were characterized according to time and frequency of oscillation and data extracted included: anteroposterior and medio-lateral amplitude (cm) and velocity (cm/s), and total velocity (cm/s) and area (cm2) of CoP total sway.
The platform calibration was performed with participants remaining in bipodal support, with their feet comfortably apart (hip width) and looking at a fixed target for 10 seconds. This procedure was made to record the body mass of each volunteer. Next, the older adults performed trials under the following conditions: bipodal support with open and closed eyes. Each trial was performed three times for 30 seconds (Winter, 2009), and the CoP area was computed considering 93% of the data points, with the initial and the last second removed to avoid initial transients and anticipation effects, respectively. Participants were instructed to wear appropriate clothing and remove footwear in all trials. At the end of the assessments, data were stored on a computer, and the signals were processed using MATLAB® (MathWorks, Inc. Natick, Massachusetts, USA) routines to obtain the aforementioned CoP related parameters.
Concerns about falling
Concerns about falling were measured using the falls efficacy scale international (FESI) (Camargos, Dias, Dias, & Freire, 2010). This scale contains 16-items on how the individual feels or would feel regarding their concerns about falling in several daily living activities, such as taking a shower, walking around the neighbourhood, cleaning the house, and going up or down stairs. Each item has possible scores ranging from one to four. In the present study, it was computed the sum of scores for each question and obtained the total score, which ranged from 16 (without concern) to 64 (extreme concern).
Muscle strength
The one maximum repetition test (1-RM) was performed to verify whether the PRT overload progression was effective. The 1-RM leg extension muscle strength was assessed using standardized recommendations, as previously described (Amarante do Nascimento et al., 2013; Santos et al., 2020). The protocol was performed by a trained evaluator and carried out in three sessions at the same time of day, with a 48-hour interval between sessions. The load recorded as 1-RM was the one at which the participant performed a single maximal voluntary action in the concentric and eccentric phases.
Adverse events monitoring
Adverse events were defined as worsening health status or the appearance of musculoskeletal or cardiometabolic problems related to the exercise-based intervention. This information was gathered monthly using a face-to-face (during classes) or telephone contact. A researcher external to the daily activities of this study reviewed and compiled a monthly report for all adverse events.
Statistical analysis
Exploratory analyses were performed to verify the distribution of variables, identification of outliers, missing data, and asymmetries. We used linear mixed models to analyze the effects of the PRT intervention on postural balance and concern about falling outcomes. Descriptive data are presented as mean and standard error or standard deviation (numerical variables), or percentage (categorical variables). Within and between-group differences are presented as mean and 95% confidence intervals. Additionally, we used the principle of intention-to-treat for all analyses. An independent blinded researcher performed all statistical procedures using SPSS software for Windows, version 22 (IBM SPSS Corporation, New York, USA). The significance level adopted was set at 5%.
RESULTS
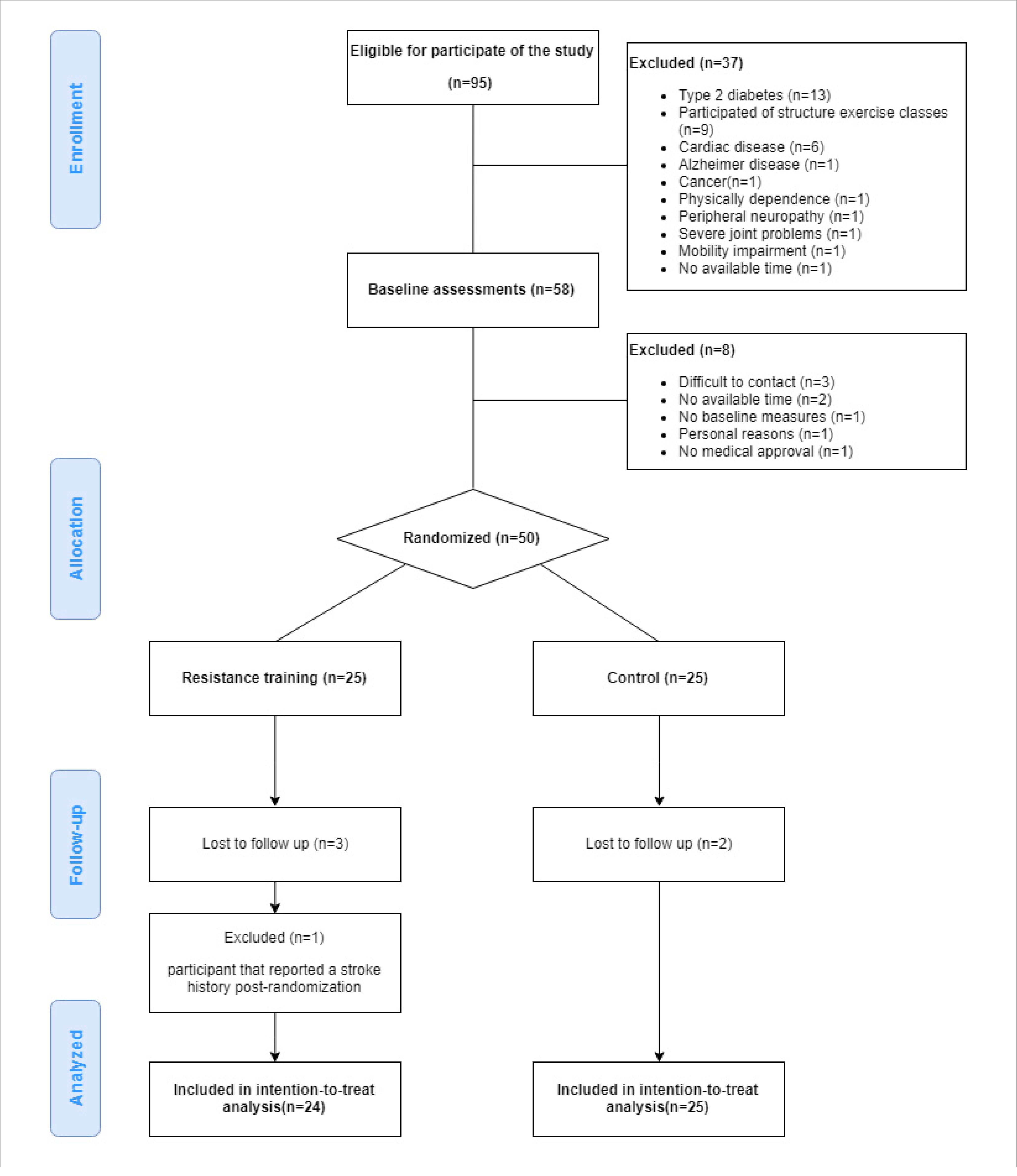
The flow chart of the study is presented in Figure 1. Of 95 potential eligible participants, a total of 58 older adults had baseline assessments; however, only 50 participants were randomized into the intervention groups. During follow-up, five participants (PRT= 3 and control= 2) withdrew from the study and one participant assigned to the PRT was excluded due to not mentioning a previous stroke at the baseline assessment (Figure 1). The mean compliance was 85.5% in the PRT, and no adverse events were observed during the study.
Table 1 presents the baseline characteristics of the study groups. The mean age was 67 years (most participants were women) with overweight (BMI> 26 kg/m2). Additionally, the mean MoCA score for PRT group was 21.5± 4.5 and for the Control group was 21.0± 4.3, both scores were < 26 points (probable cognitive impairment).
Table 1 General characteristics of participants*.
| Variables | RT (n= 24) | Control (n= 25) | |
|---|---|---|---|
| Sex (% female) | 64 | 60 | |
| Age (years) | 66 (5) | 68 (6) | |
| Education (years) | 13 (7) | 13 (6) | |
| Body mass (kg) | 68 (18) | 67 (13) | |
| Stature (m) | 1.59 (0.09) | 1.59 (0.09) | |
| BMI (kg/m²) | 26.7 (5.2) | 26.1 (4.1) | |
| Medical history (%) | |||
| Hypertension | 72 | 40 | |
| Dyslipidemia | 44 | 40 | |
| Fibromyalgia | 4 | 12 | |
| Arthritis | 8 | 8 | |
| Osteoporosis | 12 | 8 | |
*Data are presented as mean standard deviation (numerical variables) or percentage (categorical variables); BMI: Body mass index.
The effects of PRT on postural balance outcomes are presented in Table 2.
Table 2 Descriptive data of baseline and follow-up values; Effects of intervention on concerns about falling and center of pressure measures at trial completion.
| Outcomes | PRT (n= 24) | Control (n=25) | RT – CON | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (mean+/- SE) | Follow-up (mean+/- SE) | Delta change (95%CI) | Baseline (mean+/- SE) | 12-weeks (mean+/- SE) | Delta change (95%CI) | Between-group differences (95%CI) | P-value | ||
| Concerns about falling | 30.2+/- 1.1 | 29.2+/- 1.2 | -1.0 (-3.4; 1.3) | 26.4+/- 1.1 | 28.0 | 1.6 (-0.7; 3.9) | 1.3 (-2.1; 4.7) | 0.450 | |
| Bipodal eyes opened | |||||||||
| A-P amp CoP (cm) | 5.2+/- 0.4 | 4.2+/- 0.4 | -1.0 (-1.9; −0.2) | 5.5+/- 0.4 | 4.5+/- 0.4 | -1.0 (-1.8; −0.1) | -0.3 (-1.5; 0.9) | 0.642 | |
| M-L amp CoP (cm) | 3.0+/- 0.2 | 2.4+/- 0.3 | -0.6 (-1.1; −0.1) | 3.0+/- 0.2 | 2.5+/- 0.3 | -0.5 (-1.0; −0.1) | -0.1 (-0.8; 0.6) | 0.629 | |
| Total sway area (cm2) | 2.8+/- 0.5 | 3.5+/- 0.5 | 0.7 (-0.5; 2.0) | 2.9+/- 0.5 | 3.8+/- 0.5 | 0.8 (-0.4; 2.0) | -0.2 (-1.7; 1.2) | 0.753 | |
| A-P velocity (cm/s) | 2.3+/- 0.2 | 2.6+/- 0.3 | 0.3 (-0.3; 1.0) | 2.4+/- 0.2 | 2.4+/- 0.3 | -0.0 (-0.7; 0.6) | 0.2 (-0.5; 0.9) | 0.563 | |
| M-L velocity (cm/s) | 1.7+/- 0.3 | 1.9+/- 0.4 | 0.3 (-0.7; 1.2) | 1.7+/- 0.3 | 2.3+/- 0.3 | 0.5 (-0.4; 1.5) | -0.3 (-1.3; 0.6) | 0.491 | |
| Total path velocity (cm/s) | 3.2+/- 0.3 | 2.8+/- 0.3 | -0.3 (-0.9; 0.3) | 3.2+/- 0.2 | 2.9+/- 0.3 | -0.3 (-0.8; 0.3) | -0.1 (-0.8; 0.6) | 0.748 | |
| Bipodal eyes closed | |||||||||
| A-P amp CoP (cm) | 5.7+/- 0.5 | 4.5+/- 0.6 | -1.2 (-2.5; 0.1) | 6.4+/- 0.5 | 5.7+/- 0.5 | -0.6 (-1.9; 0.6) | -1.2 (-2.8; 0.3) | 0.117 | |
| M-L amp CoP (cm) | 2.9+/- 0.3 | 2.9+/- 0.4 | 0.0 (-0.9; 1.0) | 3.5+/- 0.3 | 2.4+/- 0.3 | -1.1 (-2.0; −0.2) | 0.5 (-0.5; 1.5) | 0.322 | |
| Total sway area (cm2) | 3.5+/- 0.7 | 4.2+/- 0.7 | 0.7 (-0.7; 2.2) | 3.8+/- 0.6 | 5.3+/- 0.7 | 1.5 (0.1; 2.9) | -1.1 (-3.0; 0.8) | 0.262 | |
| A-P velocity (cm/s) | 2.3+/- 0.3 | 3.0+/- 0.3 | 0.6 (-0.0; 1.2) | 3.0+/- 0.3 | 3.3+/- 0.3 | 0.3 (-0.3; 0.9) | -0.3 (-1.2; 0.6) | 0.472 | |
| M-L velocity (cm/s) | 1.8+/- 0.2 | 1.5+/- 0.2 | -0.3 (-0.8; 0.1) | 2.0+/- 0.2 | 1.4+/- 0.2 | -0.6 (-1.0; −0.1) | 0.1 (-0.4; 0.6) | 0.651 | |
| Total path velocity (cm/s) | 3.5+/- 0.4 | 3.6+/- 0.4 | 0.1 (-0.9; 1.0) | 4.1+/- 0.4 | 3.8+/- 0.4 | -0.3 (-1.2; 0.6) | -0.2 (-1.3; 0.9) | 0.710 | |
Amp: amplitude; A-P: anteroposterior; ML: medio-lateral; CoP: center of pressure. Data are presented as mean and standard error.
However, at the completion of the intervention, compared with the Control group (between-group differences), participants assigned to the PRT group did not present changes in the force platform variables (anteroposterior and medio-lateral amplitude and velocity, and total velocity and sway area of CoP) in both conditions (between-group differences to bipodal with eyes open and closed; main interaction effect: p> 0.05).
Additionally, PRT did not promote improvements in concerns about falling after completion of the intervention (between-group mean difference: +1.3 point; 95%IC −2.1; +4.7; p= 0.450). On the other hand, as expected, participants in the PRT demonstrated muscle strength gains in the leg extension exercise (between-group mean difference: +19 kg; 95%IC +3; +35) compared to the control.
DISCUSSION
Our main findings were that PRT did not promote gains in postural balance or reduce concerns about falling in healthy, community-dwelling older adults; As expected, PRT was effective in improving leg extension muscle strength, which demonstrates positive clinical implications in the light of known ageing-related physical decline and that our planed progressive overload was effective.
Our results did not show improvements in any postural balance outcome using the force platform measures at the end of 12 weeks of PRT in older adults. Previous literature investigating the chronic adaptations of PRT on postural balance is controversial, with some studies demonstrating positive effects and others no significant changes, mainly due to the studies using different tests to assess postural balance. For example, to the best of our knowledge, Orr, Raymond, and Singh (2008) were the first to perform a systematic review to analyze the effects of isolated PRT on postural balance, and the summary of the findings showed no effectiveness of resistance exercise on balance. The authors clarified that these findings might be due to low compliance in the training sessions and the heterogeneity of balance tests. Additionally, Pirauá et al. (2019) investigated the impact of 24 weeks of PRT with and without unstable surfaces on balance in healthy older adults. At the mid-point (12 weeks), compared with the control, participants of both PRT groups did not demonstrate improvements in Berg balance scores (+1.42; 95%IC −0.23; 3.08). However, at the end of the intervention (24-weeks), the PRT groups presented improved Berg scores (+1.22; 95%IC 0.19; 2.63), suggesting that the magnitude of changes induced by PRT on static balance may be dependent on the measurement test of balance and length of intervention.
In fact, when we look into studies that have been used measures of force platform, like in a trial which compared the effects of two different modalities (resistance and walking training) in older adults, Messier et al. (2000) demonstrated improvements in CoP indicators such as area, velocity, and time during the bipodal trial with eyes closed after 18 months of intervention. However, we have to highlight in this study, participants were older (aged 80 years and older), presented low physical function, and several comorbidities such as obesity (BMI> 30 kg/m2) and osteoarthritis, and the protocol employed was based on free weights progressive resistance exercises for upper and lower limbs. Similarly, the study led by Liu-Ambrose, Khan, Eng, Heinonen, and McKay (2004) also demonstrated improvements in balance outcomes after high-intensity whole-body PRT in older women with low bone mass after a long-term follow-up period (25 weeks). Thus, it is reasonable to hypothesize that the effect of PRT on postural balance may be greater in populations with poor health status.
Pooling the evidence to date, although we designed a resistance exercise protocol following the principle of progressive overload and with whole-body exercises, there was no significant effect of training on force platform variables. These findings may be due to the characteristics of the sample, which included older adults with relatively good health (average comorbidity numbers: 1.8± 1.3), and good functional capacity, as well as the short intervention length (12 weeks), all factors that could affect the training adaptations in balance. Additionally, a recent meta-analysis of Falck, Davis, Best, Crockett, and Liu-Ambrose (2019) observed that physical exercise has the potential to produce larger effect sizes in measures of physical function such as muscle strength and functional capacity, whereas the magnitude of these changes is reduced when the outcomes analyzed include flexibility and balance.
Notwithstanding that PRT improved lower limb muscular strength, there was no significant reduction in concerns about falling after the intervention. The meta-analyses conducted by Kendrick et al. (2014) pointed out that interventions with physical exercise may reduce concerns about falling; however, the quality of evidence of PRT for this outcome is low. In fact, concern about falling is a complex outcome and can be related to several factors, including physical and mental elements and behavioural and environmental outcomes (Zijlstra et al., 2009). Therefore, interventions aimed at mitigating concerns about falling should consider the interrelationship of these factors.
The strengths of our study include a randomized controlled trial approach using the intention to treat principle, measures of balance using the gold-standard method, and a protocol following the principles of training and current guidelines of PRT for older adults. However, the study also has limitations that deserve to be highlighted:
the sample size was composed only of healthy older adults; thus, the results observed cannot be generalized to participants with clinical conditions (i.e., physical and cognitive impairment);
it was not possible to blind the evaluators due to the limited staff number to perform assessments;
physical activity levels were not tracked (i.e., subject or objective measures).
However, participants received the same advice to maintain their usual lifestyle habits, and biweekly telephone calls were made to the participants in the control group to reinforce this instruction.
Practical standpoint
Although resistance training could promote important benefits for the older population in cognitive and physical aspects (Falck et al., 2019), when the objective is to improve posture balance and/or fear of falling, interventions that target specific components, as balance training, should be incorporated in exercise programs. Additionally, further investigations may address whether combining resistance and balance training (e.g., resistance training using unstable devices/surfaces) could positively modulate such outcomes.