INTRODUCTION
Maintaining physical performance, especially in long-term events, requires meticulous preparation (Hermand, Chabert, & Hue., 2019), and the physiological imbalance can result in muscle fatigue, damage, and changes in the systemic inflammatory response (Mara et al., 2013).
The achieved performance during prolonged exercise depends on several physiological factors: (a) the capacity to produce and use energy in a fast and prolonged way (Arellano & Kram, 2014) (b) the oxygen uptake (VO2max) as an indicator of the athlete’s ability to generate energy in the medium and long terms, and (c) the energy cost that represent the economy of energy expenditure at high intensity (Swinnen, Kipp, & Kram, 2018).
Another factor related to performance is the skin temperature’s ability to dissipate heat in muscle efforts (Bertucci, Arfaoui, Janson, & Polidori, 2013a; Ludwig et al., 2016), transferring the heat from the deepest tissues to the surface (Ammer & Formenti, 2016). At rest, it varies between 34°C and 36°C (Raymann, Swaab, & Van Someren, 2008), and it is performed by changes in the vascular tone of the skin and increased sweating. The blood flow is directed to the active muscles and the myocardium in order to supply their metabolic needs (Akimov & Son’kin, 2011).
The evaporation of sweat represents the main mechanism to reduce skin temperature during exercise (Chudecka & Lubkowska, 2010). At the beginning of the exercise, there may be a reduction in temperature due to sweating on the skin surface and the use of blood in the required muscles (Fernandes et al., 2012). However, in endurance sports, a constant increase in central temperature (Tcore) and skin temperature (Tskin) is observed, especially in high-temperature environments, which limits the performance and can increase the risk of exhaustion and heat stroke (Nybo, 2010).
To analyze the thermoregulation process and understand how this energy is dissipated, infrared thermography (IRT) can be used (Arfaoui, Polidori, Taiar, & Pop, 2012). Its main advantages are the non-invasive method; monitoring a specific region of interest (local analysis) or throughout the body (global analysis); freedom of movement during exercise; the lack of interference in the processes of heat loss by radiation, convection and evaporation; the accuracy; reproducibility; and the possibility of recording videos, with certain camera models (Fernandes et al., 2014).
Although the number of studies with IRT has increased in the last decade (Moreira et al., 2017), some methodological aspects remain controversial. One of them is the definition of regions of interest (ROIs) in thermal images because the Tskin can be affected by several factors of the daily routine, including nutrition, sweating, hours of sleep, and physical activity, as well as environmental factors (Fernández-Cuevas et al., 2015).
Working with athlete evaluation requires a careful evaluation to not interfere with the training routine and competitions. So, the definition of the evaluation moments and the adjustments to the protocols are extremely important to minimize interference in the athlete’s routine. Previous systematic reviews (Jimenez-Pavon et al., 2019; Fernández-Cuevas et al., 2015; Fernandes et al., 2012) concluded the effectiveness of checking Tskin using IRT. However, none of these reviews detailed the assessment protocols and Tskin behavior of endurance sports practitioners. As a result of this knowledge gap, the aim of this study was to identify the assessment protocols and the Tskin behavior of endurance sports practitioners.
METHODS
Protocol and register
This systematic review was written according to the PRISMA recommendations (Moher, Liberati, Tetzlaff, & Altman, 2015) and was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under number CRD4202018493.
Inclusion criteria
In this systematic review, experimental studies were included that met the following inclusion criteria (Moola et al., 2015): studies related to endurance sports, with trained athletes, of both sexes and aged between 16 and 49 years. In the outcome, the type of camera used, the ROIs of interest, the used protocols, and the results were considered.
Search strategy
The search occurred from March 1st to March 31st, 2020, in the National Library of Medicine (MEDLINE), Latin American and Caribbean Literature in Health Sciences (LILACS), SCOPUS, SPORT Discus, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, Science Direct, Cochrane and Scielo. The following keywords were used as descriptors for Medical Subject Headings (MeSH) or words in the text: thermography, skin temperature, infrared image, endurance sports, cycling, running, marathon, triathlon, and their synonyms. The following search phrase was obtained using the Boolean logic operators “AND” between descriptors and “OR” between synonyms: “Thermography” OR “Skin Temperature” OR “Skin thermal” OR “Infrared imaging” OR “Infrared thermography” OR “Infrared Camera” OR “Thermographic pictures” OR “Thermographic images” OR “Thermal images” AND “ Endurance training” OR “Bicycling” OR “Running” OR “Marathon” OR “Triathlon”. In addition, bibliographic references from other sources were explored to find studies that, perhaps, have not been retrieved from the databases.
Studies selection
Two independent evaluators selected the studies, and a third one resolved the disagreements found. This procedure was performed in all phases of the present study. Experimental studies that evaluated Tskin in endurance sports were selected in this systematic review. Studies of systematic reviews, case studies, reviews with meta-analysis, and abstracts (studies without full text) were excluded. Studies with a publication date prior to the year 2000 were also excluded due to the low resolution of images from older cameras.
Data collection process
The following data were extracted from the studies: profile of the participants, sex, height, total body weight, percentage of fat, maximum oxygen consumption (VO2max), ROIs used in the assessment, Tskin, type of camera, and the outcome.
Methodological quality and bias’s risk
Methodological quality and risk of bias were assessed using the Cochrane ACROBAT-NRSI scale. The instrument assesses seven domains: 1) confusion, 2) selection of study participants, 3) measurement of the intervention, 4) non-receipt of the assigned intervention, 5) losses, 6) measurement of the outcomes, 7) selective reporting of the outcomes. The first three are pre-intervention domains, and the other four are post-intervention domains. For each domain, the ratings “low”, “moderate”, “severe”, “critical”, and “no information” are assigned. The overall risk of bias in each study is the domain with the highest risk of bias (Sterne et al., 2016).
RESULTS
Figure 1 shows the flowchart of the studies included in the present study.
A total of 1128 studies were extracted from databases. The duplicated ones were excluded (421), and 16 were recovered by manual searches. From 723 studies to trial, 655 were excluded by not attending the inclusion criteria.
Table 1 shows the sample characteristic of 407 individuals who participated in these studies (380 male and 27 female). All studies presented the mean age, body weight, and height, except for Tanda (2016).
Table 1. Characteristics of the sample in the studies included in the systematic review.
| Article | Study |
|
|
|
|
|
|
|---|---|---|---|---|---|---|---|
| 1 | Perez-Guarner et al., 2019 |
|
41± 6 | 66.5± 10 | 174± 0.10 | 14± 6.1 | NI |
| 2 | Priego-Quesada et al., 2019 |
|
40± 6 | 78± 12 | 176± 0,04 | 14± 5 | 63± 6 |
| 3 | Tumilty et al., 2019 |
|
29.3± 5.8 | 65.5± 7.8 | 169.9± 6.2 | NI | NI |
| 4 | Rodriguez-Sanz et al., 2019 |
|
42.82± 6.97 | 73.19± 8.13 | 173.68± 9.79 | NI | NI |
| 5 | Priego-Quesada et al., 2017 |
|
34± 5 | 72± 12.9 | 175.7± 7.3 | NI | NI |
| 6 | Balci et al., 2016 |
|
22.2± 3.7 | 73.8± 6.9 | 181± 6.3 | 12.6± 4.2 | 54± 9.9 |
| 7 | Jensen et al., 2016 |
|
28.1± 8.2 | 69,9 ± 7,5 | 177,6 ± 7,8 | 22,1 ± 1,7 | NI |
| 8 | Ludwig et al., 2016 |
|
20.3± 1.8 | 70.14± 6.00 | 177± 0.03 | 8.64± 2.25 | 66.89± 4.55 |
| 9 | Priego-Quesada et al., 2016a |
|
29.5± 9.8 | 76.6± 9.2 | 179.2± 6.6 | NI | NI |
| 10 | Priego-Quesada et al., 2016b |
|
29± 10 | 77± 9 | 178.7± 6.5 | NI | NI |
| 11 | Priego-Quesada et al., 2016c |
|
29.9± 8.3 | 72.8± 10.6 | 175± 0.8 | NI | NI |
| 12 | Tanda, 2016 |
|
NI | NI | NI | NI | NI |
| 13 | Chudecka et al., 2015 |
|
20.77± 1.78 | 82.33± 7.19 | 184.11± 4.56 | NI | NI |
|
|
22.54± 2.01 | 86.27± 7.17 | 187.25± 4.62 | NI | NI | ||
| 14 | Priego-Quesada et al., 2015b |
|
29.3± 5.8 | 65.5± 7.8 | 169.9± 6.2 | NI | NI |
| 15 | Priego-Quesada et al., 2015a |
|
28.9± 8.3 | 72.8± 10.6 | 175.8± 8 | NI | NI |
| 16 | James et al., 2014 |
|
38± 11 | 77.3± 7.1 | 179± 8 | NI | 57.3± 4.0 |
| 17 | Abate et al., 2013 |
|
|
|
|
|
NI |
| 18 | Bertucci et al., 2013 |
|
16± 0.0 | 63.0± 0.0 | 179± 0.0 | 10.4± 0.0 | 2.87± 0.20 |
| 19 | Smith and Havenith, 2011 |
|
23± 3 | 73.8± 5.0 | 178.5± 4.1 | 10.9± 4.9 | 70.2± 13 |
|
|
24± 5.7 | 73.6± 6.9 | 181.6± 4.3 | 11.8± 4.7 | 57.9± 11 | ||
| 20 | Merla et al., 2010 |
|
25.2± 3.1 | 71.4± 4.2 | 175± 0.15 | NI | NI |
NI: not informed; kg: kilogram; cm: centimeter; O 2 max: maximal oxygen consumption; M: male; F: female.
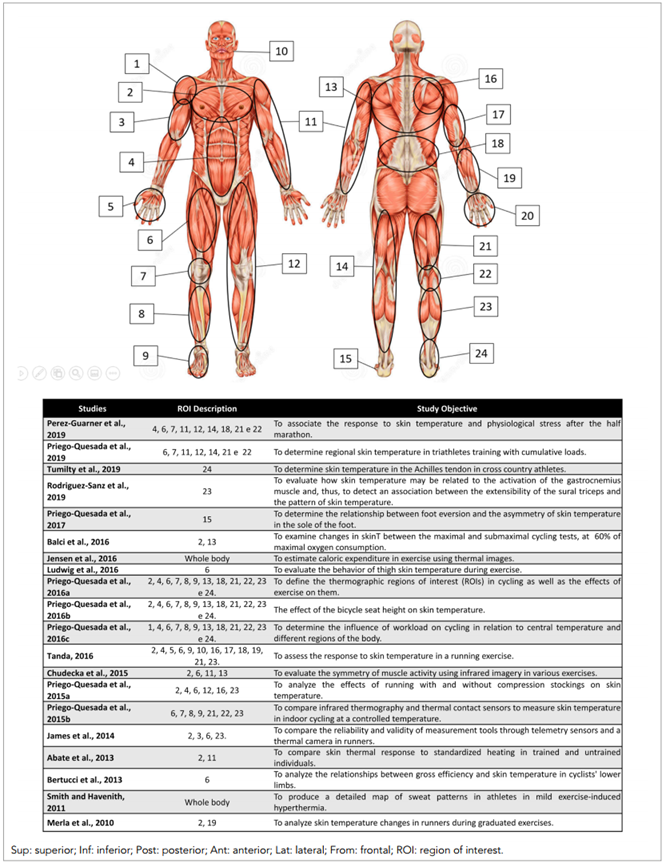
The ROIs were presented in Figure 2, where 24 different regions were used in the researchers’ assessments. The most evaluated region in endurance sports was the thigh.
Table 2 presents the type of the camera, evaluation protocols, the camera position, and the outcomes of the analyzed studies. Table 3 presents the methodological quality and risk of bias analysis of the selected studies.
Table 2. Results of the selected studies.
| Studies |
|
Evaluation protocol | Clothing | Result | ||
|---|---|---|---|---|---|---|
| Perez-Guarner et al., 2019 | C: FLIR E-60; R: 320x 240; S: TRP FLIR | Pre-race: 48h, 24h; Race: 21Km; Post-race: 24h and 48h | AT: 10min, TR: 23.2± 0.1°C; RHA: 20± 1%, TS: < 0.05º C; ES: 0.98, Ac: 2% | Underwear | skinT in the posterior upper limb and anterior leg, after the half marathon. > skinT the day before the race for most ROIs. | |
| Priego-Quesada et al., 2019 | C: FLIR E-60; R: 320x 240; S: TRP FLIR. | Mom 1 - pre camp. Mom 2 - 1st day camp. Mom 3 - 2nd day camp. Jump test: 5 to 20 squat reps (warm-up)+ 3 maximum jumps with 30sec intervals. | AT: 10 min; TR: 18°C, RHA: 44%, 54% and 63% (pre, test 1 and 2); TS: 0.05°C, ES: 0.98; Ac: ± 2°C. | NI | > skinT after training in all ROIs. > max skinT in the posterior thigh, knee and posterior leg. | |
| Tumilty et al., 2019 | C: FLIR T450SC; R: 320x 240; S: FLIR Tools (FLIR Systems Inc). | A tests session of 30 min, for nine weeks. | AT: 15min; TR: 21.8± 0.46°C, RHA: 47.3± 8.1%; Spectrum: 7.5-13μm, TS: 0.05°C; ES: 0.95 | NI | The IRT demonstrated high consistency and minimal variations in the Achilles tendon at rest during the 9 weeks. | |
| Rodriguez-Sanz et al., 2019 |
|
5 images of the gastrocnemius taken before and after Ru at 8Km/h for 15min. | TR: 24.1± 1 C; RHA: 45%± 10%, Spectrum: 8-9 μm; TS: 0.02K (30°C). | NI | After the exercise, skinT was significantly warmer for the participants in all the variables for the gastrocnemius muscle. | |
| Priego-Quesada et al., 2017 | C: FLIR E-60; R: 320x 240; S: TRP FLIR. | Mom 1 (PT) - maximum effort for 5 min (400 m track). Mom 2 - 10min warm-up, at 1% incline (60% MAS)+ 20min (80% MAS). Measurement: BT, IAT and 10 min after ending. | AT: 10min; TR: 22.9± 1.3°C, RHA: 44.4± 12.1%; TS: < 50mK (30°C), Ac: ± 1°C. | Shorts | Medial ROIs showed higher temperatures than lateral ROIs. Similar skinTs were observed in ΔT and ΔT 10 of the hindfoot. | |
| Balci et al., 2016 | C and S: Testo 875-1 ThermaCA; R: 160x 120. | Mom 1 - familiarization; Mom 2 (max test) - 70 to 85% Max HR (90 rpm), (1x 4min)+ (3x 2min)+ (nx 1min until exhaustion). > 27 to 36W/stage. Mom 3 (submaximal test): 4x 5min (until ventilatory threshold (50 to 60% Max HR Reserve> 27 to 36W at each stage). | TR: 21.3± 0.4°C; RHA: 64.5± 2.5%; TS: < 80mK (0.08°C); ES: 0.98. | Shorts,sneakers and socks | < skinT in the submaximal test until min 7.58± 1.03. After this, > skinT. In the maximal test, < skinT during the whole period and it did not increase in any Mom. | |
| Jensen et al., 2016 | C: AXIS Q1922; R: 640x 480; S: AXIS Communications | Mom 1 - warm-up 4min work 30sec recovery. Speed: 3, 5 and 7Km/h Mom 2 -- 8, 10, 12, 14, 16, 18Km/h (Ru) | TS: < 100mK; ES: NI. | NI | > skinT with> Speed. It was not significant between 16 and 18km/h. The average values of the optical flow for all the 14 individuals demonstrated a strong correlation with oxygen uptake. | |
| Ludwig et al., 2016 | C: AVIO TVS700; R: 320x 240; S: thermal images analysis software. | Mom 1 -- 10-min warm-up (100W); - Test- 100W+ 25W/min (80 to 90rpm). Measurement: BT, after warm-up, intra and IAT | AT: 10min; TR: 22-23º C, RHA: 50± 5%; Spectrum: 0.98, TS: NI; ES: NI. | NI | Base temperature was 32.50°C± 0.67. Post-exercise< skinT (30.87°C± 0.73). > skinT after release (3min) (32º C) and skinT after release (6min) reached 32.50º C. | |
| Priego-Quesada et al., 2016a | C: FLIR E-60; R: 320x 240; S: TRP FLIR. | Mom 1 (PT) - 5-minute warm-up (50W)+ 25 W/min until exhaustion (90± 3rpm). Mom 2 (test) - 3-min warm-up at 50 W (90± 2 rpm)+ 45 min at 50% of maximal power (90± 2rpm). Measurement: BT, IAT and 10min ΔT of Cy. |
|
Underwear |
|
|
| Priego-Quesada et al., 2016b | C: FLIR E-60; R: 320x 240; S: TRP FLIR. | Mom 1 (PT) - 5-min warm-up at 50W+ load increase of 25W/min until exhaustion (90± 3rpm); Mom 2 (test): 3-min warm-up at 50W (90± 2 rpm), followed by 45min at 50% of maximal power (90± 2rpm). | AT: 10min; TR: 23.4± 1.1 °C, 23.6± 1.2°C, 24.0± 1.2°C; RHA: 45.4± 12.5 %, 40.7± 11.3%, 50.8± 11.2%; TS: 0,05°C, Ac: ±2%. | Underwear | The knee flexion at 20° caused > skinT in the popliteal than at 40°. No differences in absolute temperatures among the three flexion angles in the other fifteen ROIs were found. | |
| Priego-Quesada et al., 2016c | C: FLIR E-60; R: 320x 240; S: TRP FLIR TRP FLIR. | Mom 1 (PT) - 5-min warm-up (50W)+ 25W/min until exhaustion (90± 3 rpm). Mom 2 (test): 3-min warm-up (50W) (90± 2rpm)+ 45min at 35% and 50% of maximal power (90 ± 2 rpm). Measurement: BT, IAT and 10min after ending. | AT: 15min; TR: 21.8± 0.7°C, 21.2± 0.8°C; RHA: 39.4± 4.5%, 39.0± 4.9%; TS: 0.05°C, ES: NI; Ac: ± 2%. | Underwear | There are no differences in the absolute values of skinT between workloads (35% or 50%) in any ROI. In addition, Cy workload presented no effect on skin temperature variation in most ROIs. | |
| Tanda, 2016 | C: FLIR T335; R: 320x 240. | Mom 1 (progressive load): 6km/h+ 1.5Km/h, each 5min, until 13.5km/h. Mom 2 (constant load): 5min (6Km/h)+ 25min of Ru (12km/h), Measurement: each 5min. | AT: 10min, TR: 22± 0.3º C; RHA: 60± 2%, TS: 0.05°C; ES: 0.98. | T-shirt, shorts and sneakers | Progressive load - < skinT. In constant exercise, < skinT reached a minimum value in the beginning, followed by an increase. | |
| Chudecka et al., 2015 | C: ThermaCAM SC500 camera; R: 320x 240; S: Agema Report. | Mom 1 (Group 1): 30-min warm-up+ 2000m test (rowing). Mom 2 (Group 2): 90min of resistance training (real game). Measurement: 20min BT and IAT. | AT: Group 1 - 30min; Group 2 - 20min TR: 25°C, RHA: 60%. | Shorts and sneakers | IAT, skinTs were smaller than the initial ones. Group 1 - there was no asymmetry in skinT. Group 2 - there was asymmetry both at the dominant and non-dominant sides. | |
| Priego-Quesada et al., 2015b | C: FLIR E-60; R: 320x 240; S: TRP FLIR. | Mom 1 (PT): 5min (max) 400m track. Mom 2 (test): 10-min warm-up+ 20min (75% MAS)+ 3min at 60% and 1min at 5Km/h. Measurement: BT, IAT and 10min after it. | AT: 10min, TR: 23.7± 0.8°C; RHA: 48.8± 10.9%, TS: 0.05°C; ES: NI, Ac: ± 2%. | Undressed | Wearing socks led to > skinT in the regions of the body that were in contact with the garment. It also led to > skinT in some regions of the body that were not in contact with the garment. | |
| Priego-Quesada et al., 2015a | C: FLIR E-60; R: 320x 240; S: TRP FLIR. |
|
|
Underwear | There was no difference between the measurement methods (IRT and thermopar sensor) in the pre-test but some differences IAT and after cool-down. | |
| James et al., 2014 | C: FLIR e40BX; R: 160x 120; S: Flir tools. | Mom 1 (test): 5min treadmill (8Km/h), followed by 5x 3 min (8 to 10Km/h) and increasing 1Km/h in each set. | AT: 40min, TR: 31.9± 1º C; RHA: 61± 8.9%, Spectrum: 7.5-13μm, TS: < 0.045°C, ES: 0.98; Ac: ± 2%. | NI | The reliability of the telemetry was acceptable during stress tests, while the IRT displayed some errors due to the sweat rate as a result of exposure to heat during the test. | |
| Abate et al., 2013 | C: FLIR SC3000; QWIP; R: 320x 240; S: TRP FLIR 2.9. | Mom 1 (test): 1st Step: 0-5 min at 100W (60rpm); 2nd Step: 5-10min at 130W (60rpm); 3rd Step: 10-15 min at 160W (60rpm). | AT: 20 min, TR: 23 ± 1°C; RHA: 55± 10%, Spectrum: 8-9 μm, TS: 0.02K, Lens: 20º; ES: 0.98. | Shorts and sneakers | > skinT in untrained athletes than in trained athletes. | |
| Bertucci et al., 2013 | C: Cedip Titanium HD560M; R: 640× 512. | Mom 1 (test): 4-min warm-up+ 4min (100W)+ 40W each 4min. Measurement BT, during and immediately after ending. | Wavelength: 3.5 to 5 mm^ 0.25 mm. | NI | skinT at rest reached 31.41°C (before) and the same value afterwards. In individual 2, skinT reached 31.98°C (before) and + 0.9°C afterwards. During the test and 5 min after it, skinT reached the same temperature in individual 1 and it rose 0.9°C in individual 2 . | |
| Smith and Havenith, 2011 | C: Thermacam B2, FLIR; R: 160x 120 |
|
TR: 25.6± 0.4°C; RHA: 43.4± 7.6%. | Shorts and t-shirt | > Sweat rates in the central region (upper and middle) and lower back. < values (fingers, thumbs and palms). > sweat rates in the forehead compared to values in the chin and cheeks. > sweat rate in all regions (low and high intensity exercises) except for the feet and ankles. | |
| Merla et al., 2010 | C: FLIR SC3000 QWIP; R: 320x 240 | Mom 1: 7x 2 min of TR, 10% of incline and speeds (3, 5, 7, 9, 11, 13, 15Km/h). | AT: 20min; TR: 23 to 24º C, RHA: 50± 5%, Spectrum: 8-9μm | NI | After warm-up, < skinT, from stage 2 to 6, from 3º to 5°C and > skinT in recovery. | |
ROI: region of interest; C: camera; R: resolution; S: software; skinT: skin temperature; AT: acclimatization time; TR: temperature in the room; RHA: relative humidity of air; TS: temperature sensitivity; TR: treadmill running; W: watts; BT: before the test; IAT: immediately after the test; ΔT: time after the test; ES: emissivity of skin; Ac: Accuracy; PT: pre-test; Te: test; PoT: post-test; Ru: running; Cy: cycling; NI: not informed; Pos: position; Dist: distance; H: height; Mom: moment; IRT: infrared thermography; Thermacam Researcher Pro 2.10 software, FLIR: TRP FLIR.
Table 3. Methodological quality and risk of bias of the selected studies.
| Studies | Pre-intervention | During intervention | Post intervention | Risk | ||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| Perez-Guarner et al., 2019 | Low | Low | Low | Low | Low | Low | Low | Low |
| Priego-Quesada et al., 2019 | Low | Low | Low | Low | Low | Low | Low | Low |
| Tumilty et al., 2019 | Low | Serious | Moderate | Low | Low | Low | Low | Serious |
| Rodriguez-Sanz et al., 2019 | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
| Priego-Quesada et al., 2017 | Low | Low | Low | Low | Low | Low | Low | Low |
| Balci et al., 2016 | Moderate | Serious | Moderate | Low | Low | Low | Low | Serious |
| Jensen et al., 2016 | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
| Ludwig et al., 2016 | Low | Low | Low | Low | Low | Low | Low | Low |
| Priego-Quesada et al., 2016a | Low | Low | Low | Low | Low | Low | Low | Low |
| Priego-Quesada et al., 2016b | Low | Low | Low | Low | Low | Low | Low | Low |
| Priego-Quesada et al., 2016c | Low | Low | Low | Low | Low | Low | Low | Low |
| Tanda, 2016 | Low | Low | Moderate | Low | Low | Low | Low | Moderate |
| Chudecka et al., 2015 | Low | Low | Low | Low | Low | Low | Low | Low |
| Priego-Quesada et al., 2015b | Low | Low | Low | Low | Low | Low | Low | Low |
| Priego-Quesada et al., 2015a | Low | Low | Low | Low | Low | Low | Low | Low |
| James et al., 2014 | Low | Low | Low | Low | Low | Low | Low | Low |
| Abate et al., 2013 | Low | Low | Low | Low | Low | Low | Low | Low |
| Bertucci et al., 2013 | Serious | Low | Serious | Low | Low | Low | Low | Serious |
| Smith and Havenith, 2011 | Serious | Low | Moderate | Low | Low | Low | Low | Serious |
| Merla et al., 2010 | Low | Low | Moderate | Low | Low | Low | Low | Moderate |
1) confusion; 2) selection of study participants; 3) assessment of intervention; 4) non-receipt of assigned intervention; 5) losses; 6) assessment of outcomes; 7) selective report of outcomes.
The main sources of bias in the present review were related to the pre-intervention and intervention phases. The lack of acclimatization of the volunteers before thermographic evaluations generated a confounding bias in sample results since the Tskin can be affected by movements prior to data collection, suggesting a moderate or severe risk in this domain (Rodriguez-Sanz et al., 2019; Balci, Basaran, & Colakoglu, 2016; Jensen et al., 2016; Bertucci et al., 2013; Smith & Havenith, 2011). Another bias observed in these studies was the sampling process, generating a selection bias, which was carried out for convenience (Tumilty, Adhia, Smoliga, & Gisselman, 2019; Balci et al., 2016). Some studies presented risks of bias during the intervention because they did not present information such as the position of the individuals, distance from the camera, the position of the camera, and characteristics of the equipment (Tumilty et al., 2019; Balci et al., 2016; Tanda, 2016; Smith & Havenith, 2011; Merla, Mattei, Di Donato, & Romani, 2010).
DISCUSSION
This systematic review identified 20 studies using IRT in endurance sports practice. It was organized by the patterns of Tskin assessment in endurance sports, such as ROI, equipment, protocols, and results.
The Tskin is influenced by the ambient temperature, and to avoid thermoregulatory effects, such as loss and gain of heat that can interfere in the IRT results, the ambient temperature must be between 18 and 25°C (Priego-Quesada, Salvador, & Cibrian, 2017). It can be seen that most of the included studies used this temperature range, with the exception of James, Richardson, Watt and Maxwell (2014), who used 31.9± 1°C. Other studies did not inform the temperature during the data collection (Jensen et al., 2016; Bertucci et al., 2013).
Another relevant element to observe is the relative humidity of the air since it influences the heat exchange between the body and the environment (Grinzato, 2010). There was no standardization since the relative humidity of the air presented in the studies varied from 19 to 69.9%. Two studies did not present it (Jensen et al., 2016; Bertucci et al., 2013). In humid environments, the effectiveness of heat loss decreases, and the humidity can condense in the body, resulting in heat gain that can alter the thermographic image captured (Johnson, 2010; Priego-Quesada et al., 2017).
In addition to the environmental variables, the acclimatization duration into the data collection room is also a considerable condition in IRT use (Marins et al., 2014). A great amplitude of acclimatization was found, varying from 10 minutes (eight studies) to 40 minutes (one work). Five studies did not report the use of acclimatization (Rodriguez-Sanz et al., 2019; Balci et al., 2016; Jensen et al., 2016; Bertucci et al., 2013; Smith & Havenith, 2011). However, there was a non-standardization about the clothing of subjects, where 6 studies standardized underwear (articles 1, 9, 10, 11, 14, and 15 according to Table 1), 1 using only shorts (5), 2 with shorts and sneakers (13 and 17), 1 with shorts and T-shirt (19), 1 with shorts, sneakers and socks (6), 1 with T-shirt, shorts and sneakers (12) and 8 studies did not inform the used clothing during the tests (articles 2, 3, 4, 7, 8, 16, 18, 20). These results reflected the importance of a standardization presented by Moreira et al. (2017) in the TISEM checklist. Since the type of clothing and acclimatization period influences the Tskin and affects the evaluated ROIs.
In general, there was an increase in Tskin after exercise (16 studies). However, one study observed a decrease in Tskin throughout the test (Balci et al., 2016). Priego-Quesada et al. (2016c) did not observe any variation in Tskin for the workload used. Tanda (2016) found that the individual’s average Tskin decreases continuously during the progressive load exercise, whereas Chudecka, Lubkowska, Leznicka and Krupecki (2015), while measuring immediately after exercise, observed that the average Tskins were lower than the initial ones.
These results may be influenced by the lack of standardization of the period of the data collection. Ten studies (articles 1, 2, 3, 6, 10, 14, 16, 17, 19, and 20, according to Table 1) collected the infrared images always at the same time, respecting the subjects’ circadian cycle. Only 1 study (9) reported that the data collections were carried out at different times, presenting it as a limitation of the research, and the other studies (4, 5, 7, 8, 11, 12, 13, 15, 18) did not control or did not report the data collection time. This fact could represent some bias since there is a correlation between the individual’s circadian cycle with skin temperature (Moreira et al., 2017).
Most of the studies noticed a decrease in Tskin in the initial moments of physical activity that occurs due to the directing of blood flow to the active muscle generated by cutaneous vasoconstriction. This same behavior was described by Neves et al. (2015a) in their systematic review about the thermal response in different types of exercise. These authors reported that the decrease in Tskin during initial moments of physical activity was verified in different parts of the body. This behavior is due to skin blood adjustments that promote vasoconstriction of the blood vessels in inactive regions, offering greater blood flow to the muscular region under stimulation (Neves et al., 2015a). The performed tests in this systematic review ranged from a maximum test with incremental load to exhaustion (articles 1, 5, 6, 8, 9, 10, 11, 13, 14, and 18 according to Table 1) and tests with controlled load (2, 4, 7, 12, 15, 16, 17, 19 and 20) that reflects the greater vascularization at the active muscles.
After this initial decrease in Tskin, there is no standardized reaction. Several factors were pointed as responsible for the Tskin behavior in the subsequent minutes, but the duration and intensity of exercise were the main ones. These findings are in line with those reported by (Neves et al., 2015b).
The IRT has been consolidated as an excellent tool for evaluating Tskin and body thermoregulatory responses during exercise, however, caution is needed. The sensitivity of the skin to external agents such as ambient temperature, relative humidity, activities performed before data collection, and procedures during the evaluation can significantly affect the data collected.
It also must be pointed that the resolution of the cameras influences the results. Nonetheless, only 2 (articles 16 and 19) used equipment with resolution lower than 320x 240 pixels, besides, 7 studies (articles 1, 2, 6, 9, 12, 16, and 17) reported camera 0.98 emissivity and one study (3) reported 0.95 emissivity, below the value predicted at TISEM checklist.
The limitations of this review are related to IRT and the difficulty of controlling the factors that affect the thermal responses of these studies. The risks of bias related to selecting the samples and the lack of blinding evaluators in the outcome indicate that these results must be analyzed with caution.
CONCLUSION
Based on the presented studies, it could be concluded that the thermal assessment protocols for endurance sports respected the acclimatization time in 75% of the selected studies and that the thermal image collections were performed, predominantly, in three moments: before the test, immediately after the test and 10 minutes after the test. The used ROIs were mostly selected in responses of a specific muscle recruited in each modality, emphasizing lower limbs muscles.
Regarding the equipment used, FLIR cameras were used in 70% of the studies, with a minimum resolution of 320x 240 pixels. This aspect is very relevant since the results will always be associated with the software, quality, and technology of equipment, paying attention to the resolution (pixels), accuracy, and, mainly, to the data collection procedures (distance, camera angle, controlled stability, acclimatization, ambient temperature, and relative humidity.
Mostly, the Tskin behavior in endurance sports decreased in the initial moments of physical exercise and increased after exercise. After this initial decrease in temperature, the thermal response is mainly dependent on the duration and intensity of exercise. At constant speed exercise, the Tskin increased after a few minutes of the beginning.
However, there are still many questions about the effectiveness and precision of field assessments about thermal responses in endurance sports during exercise, which can be explored in future researches.