Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Motricidade
versão impressa ISSN 1646-107X
Motri. vol.13 no.3 Ribeira de Pena set. 2017
https://doi.org/10.6063/motricidade.10058
ORIGINAL ARTICLE
Prevalence of Developmental Coordination Disorder signs in children 5 to 14 years in São Carlos
Patricia Carla de Souza Della Barba1,*; Erika Marques Luiz1; Raquel Cristina Pinheiro1; Gerusa Ferreira Lourenço1
1 Universidade Federal de São Carlos, São Carlos, Brazil
ABSTRACT
This study aimed to identify the prevalence of Developmental Coordination Disorder (DCD) in children aged 5-14 years, enrolled in public preschools and elementary schools in São Carlos - SP. There were 130 participating families. Instruments were: Developmental Coordination Disorder Questionnaire – Brazil (DCDQ - Brazil), Brazil criteria and a questionnaire for the characterization of children. The prevalence of DCD found was 30%, which is overestimated when compared to data found in much of the literature, justified by the use of the instrument for detection of the DCD. No significant difference was found between the presence of signs in boys and girls and there was a higher concentration of children with DCD signs on B2, C1 and C2 socioeconomic classes. The prevalence of DCD signs was higher in children over 8 years.
Keywords: Motor Skills Disorders, Developmental Coordination Disorder, Children, Prevalence, Developmental Coordination Disorder Questionnaire – Brasil (DCDQ - Brasil).
INTRODUCTION
Human development consists of progressive changes throughout life. In turn, the motor development is facing the movement and control of body parts, with a focus on childhood, as the child grows the development of the skills is enhanced (Berns, 2002).
To identify deficits in child development is essential to prevent possible future sequels. Once acknowledged, such interventions can minimize delays and therefore minimize future development disorders. Motor problems in childhood can significantly influence the performance of the child's daily activities. When such motor difficulties are not explained, i.e. by congenital or acquired neurological disorders, or global intellectual disability, we deal with Developmental Coordination Disorder (DCD) (Missiuna, Pollock, Egan, DeLaat, Gaines, & Soucie, 2008).
The DCD signs are noticeable. The child may have difficulty in action planning, organization, implementation and/or modification of their movements, as well as learning new skills. The movements of the child with DCD may seem immature when compared to their peers of the same age. Children do not recognize easily this error in motor execution, therefore, do not learn from their own mistakes to correct them, making it difficult to acquire new skills and change strategies to perform the same task (Missiuna, Gaines, Mclean, LeLaat, Egan, & Soucie, 2011; Silva & Beltrame, 2013, Missiuna et al, 2014).
Several motor aspects can be affected, as fine motor skills, gross motor function and postural control during movement execution. The impact is especially noticeable in everyday activities such as dressing, to tie the shoelaces, using cutlery, cycling, grab and throw a ball. However, some children have only academic performance, particularly in writing and spatial organization (Asonitou, Koutsouki, Kourtessis, & Charitou, 2012; Magalhães, Rezende, Amparo, Ferreira, & Renger, 2009).
These features make DCD heterogeneous, moreover, some co-morbidities are common such as Deficit Disorder, Attention Deficit Hyperactivity Disorder, learning problems and social-affective problems, making diagnosis a challenge (Ferreira, Nascimento, Apolinário, & Freudenheim, 2006).
The DSM - IV provides four diagnostic criteria that are essential and guide through the identification of DCD:
Criterion A: Performance in daily activities that require motor coordination is substantially lower than expected, considering childs age and individual intelligence. The motor disorder can manifest with significant delays in reaching motor milestones (eg, walking, crawling, sitting), dropping to things, "clumsiness," poor performance in sports, or poor handwriting.
Criterion B: The disturbance in Criterion A significantly interferes with academic achievement, or activities of daily living.
Criterion C: The disturbance is not due to a general medical condition (e.g., cerebral palsy, hemiplegia or muscular dystrophy) and does not meet criteria for Pervasive Developmental Disorder.
Criterion D: If their mental retardation and motor difficulties are greater than those normally associated with cognitive impairment. The DCD is characterized by marked impairment in the performance of motor activities, with significant negative impact on the performance of daily living activities and may include difficulty with global and fine motor skills. (American Psychiatric Association [APA], 2002, p. 49-50).
In DSM - 5, most current version of the manual, new features are considered to diagnose DCD:
Criterion A: The acquisition and execution of coordinated motor skills are substantially lower than expected, considering the chronological age of the individual and the opportunity to learn and use the skill. The difficulties are manifested by clumsiness (p. Ex., Dropping or hitting objects), as well as slow or inaccuracy in the performance of motor skills (eg., take an object, use a knife or scissors, writing hand, cycling or playing sports).
Criterion B: O déficit nas habilidades motoras descritas no critério A devem interferir significativamente e persistentemente nas atividades diárias adequadas à idade cronológica (por exemplo, autocuidado e auto-manutenção), impactando a produtividade acadêmica / escolar, atividades pré-profissionais e profissionais, bem como no lazer e ao jogar.
Criterion C: The onset of symptoms occurs early in the development period.
Criterion D: Deficits in motor skills are not better accounted for by intellectual disability (Disorder Intellectual Development), or visual impairment and are not attributable to any neurological condition affecting movements (eg., cerebral palsy, muscular dystrophy, degenerative disease) (APA, 2014. p. 74-77).
With the DSM - 5 it was explicit the need for the child to have the opportunity to learn and use the requested skill. It was also clear in DSM - 5 that motor impairment should affect daily activities appropriate to chronological age. Another point made clear in the new manual is that symptoms should occur very early in the child's development, a point that did not appear in the manual used in this study.
To evaluate the four diagnostic criteria, according to the two versions of the DSM, a multidisciplinary work team is needed , since it is necessary to evaluate motor performance, impact on daily living activities, overall clinical condition and evaluate subjects intellectual condition (Missiuna et al, 2008).
No tests considered the gold standard for assessing these criteria, but there are some frequently used by researchers. According to Souza (2015), most of the studies analyzed in a systematic review, the criterion A was evaluated by the test Movement Assessment Battery for Children (MABC-2); for the criterion B, the most widely used questionnaire was the Developmental Coordination Disorder Questionnaire (DCDQ). To assess the criterion C and D there was no prevalence of any evaluation or specific instrument.
When all the diagnostic criteria listed in the DSM - IV are not assessed it cannot be said that the subject has DCD, for this reason many studies consider as probable DCD. Consequently, the prevalence of DCD ranges from 1.4% to 19% (Lingman, Hunt, Golding, Jongmans, & Emond, 2009; França, 2008; Silva & Beltrame, 2013). This variation reflects the different methodologies used to identify the prevalence of DCD in different contexts (Zwiker, Missiuna, Harris, & Boyd, 2012).
In the literature produced in Brazil there are few studies described that measure the prevalence of DCD and, for the most part, the whole DSM-IV is not evaluated. França (2008) sought to characterize the children motor performance investigating the prevalence of DCD, but he only used the MABC to assess motor performance of 417 children. The other criteria are not specified in the aforementioned study; thus, the prevalence of probable DCD was found to be 10.8%. The same occured in the study of Silva and Beltrame (2013), where 406 children were evaluated using only the MABC, that is, only assessing criterion A, and a prevalence of 11.1% was found.
More recently, two studies identified the prevalence of DCD in children in the state of São Paulo. Joias study (2014), in order to identify the DCD in seven years old children, enrolled in public schools in the city of Araraquara, SP, and based on the DSM - IV, used the MABC - 2 to assess the criteria A, the DCDQ - Brazil to evaluate the criteria B. Criteria C and D were evaluated implicitly by the researcher and by parental and teachers report. In this study, it was found a prevalence, joining the motor test and the questionnaire, of 0.99% for severe DCD and 2.97% for moderate DCD, according to the classification of the instrument used in the study (MABC - 2). The study by Silva (2015) using the DSM - 5 and MABC-2, DCDQ-Brazil and teachers report - identified a prevalence of DCD of 7.93% in children of seven years old of public schools, in Itirapina, SP.
Studies that use only one instrument to identify the prevalence of DCD, thus evaluating only one DSM criterion, tend to increase this percentile. Like that of Franca et al. (2015), that found a prevalence of 47%. The study evaluated, through the DCDQ - Brazil Instrument, 535 children aged 7-8 years living in the city of João Pessoa, Paraiba - Brazil. This confirms once again the need to combine different instruments and professionals to diagnose the disorder.
Against a broad impact of DCD on the child's life, both in social and academic performance, as well as in participation in motor activities typical for the age, there is a lack of studies that prove the prevalence of DCD in Brazil.
The realization of an early identification as a decisive action for effective treatment can enable the education and guidance of all every day childrens stakeholders, avoiding negative impacts on the day-to-day(Cardoso & Magalhães, 2012).
This study is justified by the need to map the prevalence of DCD as early as possible, as well as to provide resources monitoring and guidance to teachers and schools.
The aim of this study was to identify the prevalence of Developmental Disorder Coordination (DCD) in children aged 5-14 years enrolled in pre-schools and primary public schools in São Carlos – SP, considering the variables age, gender and economic classification.
METHOD
This research was approved by the Committee of Ethics in Research of the Federal University of São Carlos, Brazil, with the number 409.521/2013.
The research was quantitative. and cross-sectional aiming to describe individuals of a population and its characteristics, analyzing the phenomenon at a given point in time.
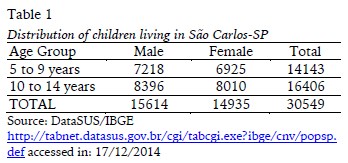
SampleAfter consulting the Census 2012, it was found the number of children in the age group of interest, residents of the city, divided by gender (Table 1).
Considering the data pointed by the literature, the estimated prevalence of DCD is 5 to 15% of school-age children (5-11 years) (APA, 2002; Cairney, Hay, Mandigo, Wade, Faught, & Flouris, 2007; França, 2008; Miranda, Beltrame, & Cardoso, 2011; Silva, Contreira, Beltrame, & Sperandio, 2011).
In this sense, it was necessary to calculate the sample size to detect an expected prevalence of 10% with 90% confidence and a maximum error of 5%. To ensure the validity of the study a minimum sample of 97 individuals would be required.
The study included 130 families of children from public schools in the city of São Carlos, SP, aged 5-14 years and 11 months. This age was selected to fit the scope of the questionnaire (DCDQ - Brazil).
In addition to the above features, it was considered only families who signed the Terms of Consent. Moreover, were excluded the children with a clinical diagnosis of physical or cognitive deficits (cerebral palsy, autism, muscular dystrophy, hearing or visual impairment), or children who have attended some form of physical rehabilitation services (Occupational Therapy, Physical Therapy, Psychomotor, etc.).
InstrumentsThe Economic Classification Criterion Brazil (2012), aims to classify the economic classes of the participants families defined in A1, A2, B1, B2, C1, C2, D and E. It evaluates the purchasing power of consumers through a system of points, with questions about the ownership of items and level of education of the household head (ABEP, 2012).
The Developmental Coordination Disorder Questionnaire - Brazil (DCDQ - Brazil) is a questionnaire for parents, self-administered. It evaluates the performance of children in different situations of daily life. Aims to screen DCD signs in 5-14 years and 11 months old children. The DCDQ has 15 items, which are divided into three groups: motor control during movement, thin/writing motor skills and overall coordination. To answer the questions, parents are instructed to compare their children with other children of the same age, where it says, "is nothing like a child", matches the score 1, to "extremely like your child", matches the score 5. All questions must be answered to allow the sum of the final score. The maximum score is 75. There are three cutoff points for DCD identification, and the age group of 5 to 7 years and 11 months, the score of 1-46 indicates that the child is suspected of having DCD; 8 to 9 years and 11 months, a score of 1-55 identifies that children have DCD signals; 10 to 14 years and 11 months, children between 1-57 scores are suspected of having DCD. The cutoff score used was validated in Canada (Cairney et al, 2007; Prado, Magalhães, & Wilson, 2009; Wilson, Kaplan, Crawford, & Roberts, 2007).
Questionnaire characterizing children - contains questions that aim to identify date of birth, prematurity, physical or intellectual disabilities, school problems, medication use and specialized treatment, based on the parents / guardians report.
ProceduresData collection was conducted in five public schools. This number has been defined using statistical calculations, seeking representation of the city.
The data collection took place from the following steps:
1 - Telephone contact with each school;
2 - Meeting with the Director and/or Teaching Coordinator to explain the research, request authorization and decide the best strategy for distribution of questionnaires;
3 - Distribution of questionnaires, which occurred in three ways: a) Delivered and returned by the students for parents to respond at home; b) Meeting with parents to answer the questionnaires in the presence of the researcher; or c) Delivered directly to parents address and returned by them to teachers.
4 - Gathering of questionnaires.
Statistical analysisIn the data analysis we used Fisher's exact test, which tests the significance for contingency tables based on the calculation of the probability of a particular data arrangement from a hypergeometric distribution. It is often employed when the sample size is relatively small due to be able to calculate, for example, the exact p-value, it does not depend on asymptotic results (Agresti, 2002).
RESULTS
Sample Profile
The study sample was composed of a balanced number of boys (48%) and girls (51%) randomly selected (Table 2).
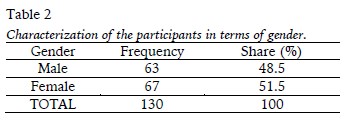
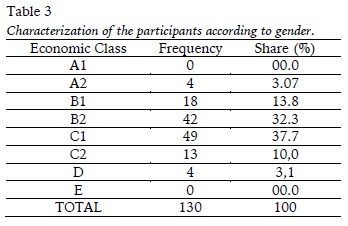
Table 3 shows that there was a higher concentration of participants in economic classes B2 and C1, according to the Economic Classification Criteria of Brazil.
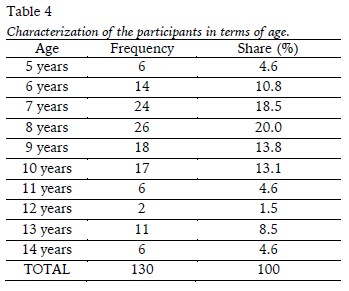
As to age, we can see in Table 4 that there was a concentration of participants between 7 and 10 years.
Descriptive results of DCDQ instruments - Brazil
DCDQ - Brazil
The DCDQ - Brazil classifies the child as "Probable DCD" or "Likely not DCD" according to the final score obtained in the questionnaire and according to each age group. Table 5 shows the results obtained by means of DCDQ - Brazil.
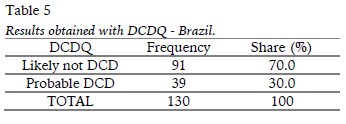
Table 5 highlights that 39 children had scores lower than expected, indicating "probable DCD", that is, 30% of the participants have to indicate DCD.
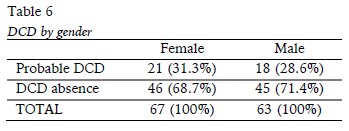
Association analysis of the variablesIn Table 6, it can be observed that the percentage of girls with DCD probability (31.3%) is very similar to boys (28.6%). Fisher's exact test was performed to verify this finding (p = 0.848), reinforcing the view that the percentage of DCD likely in children is independent of its gender.
Based on Table 7, it is plausible to say that DCD is related to the purchasing power of the families of children (Classification Criteria of Brazil), when we group the classes in A, B, C and D. Of the four children who belonged to the classification A, none had a likelihood of DCD. As in class B, only 9 of the 60 children (15%) presented DCD likely. In class C, approximately 48% of the children presented a probability of DCD.
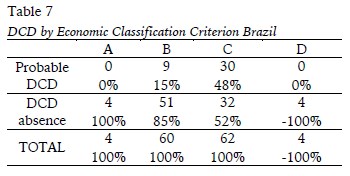
The p-value obtained by applying Fisher's exact test for this case was about 0.0003, thus reinforcing the relationship between DCD and household purchasing power.
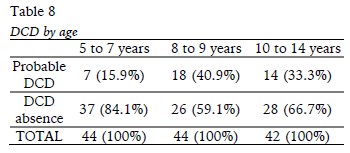
In view of Table 8, it was observed that the percentage of DCD is likely related to the age of the children. This percentage is only 15.9% in children aged 5-7 years and eleven months, against 40.9% in children aged 8-9 years and eleven months and 33.3% in children aged 10-14 years and eleven months (p=0.03).
DISCUSSION
This study aimed to identify the prevalence of Developmental Coordination Disorder (DCD) in children aged 5-14 years and 11 months, using self-administered questionnaires, considering the variables age, gender and economic classification.
With regard to the identification of the DCD signal, the results of the present study indicate a prevalence of 30%. Such findings are in line with the data found in the research of Franca et al. (2015). The prevalence found by the authors was 47% in a total of 535 children in the city of João Pessoa, Paraíba - Brazil, from the application of the DCDQ - Brazil Instrument (Franca et al, 2015). The high incidence is justified by the methodology of the study, which used only one tool for the detection of DCD signals. The instrument serves mainly for criteria B of the DSM - IV and partly for criteria A. Criteria C and D were evaluated according to the principles of the parents' vision, through a structured interview, general medical condition check and presence of physical or mental disabilities (Franca et al., 2015).
Studies that did not evaluate all the diagnostic criteria established by the DSM - IV present a higher prevalence than those that assessed all criteria (França, 2008; Silva & Beltrame, 2013). The more tools and professionals involved in the evaluation, the safer the diagnosis will be. This was emphasized and more clearly defined from the DSM - 5, where the correlation between the criteria and the need to assess each with a specific instrument is explicit.
The European Academy of Childhood Disability (EACD), guides that several professionals should participate in the diagnostic evaluation, as a medical doctor, psychologist, occupational therapist, physiotherapist and physical educator. The EACD brings DCDQ and MABC as the instruments best suited at the moment, to evaluate and diagnose the DCD, together with a medical evaluation to certify the absence of any physical or neurological disorders that may interfere with the childs motor capacity and a psychological evaluation attesting to the absence of cognitive and intellectual problems that may interfere with their performance (Blank., Bouwien, Polatajko, & Wilson, 2012).
Civetta (2008), developed the first study comparing the results found in two instruments, the MABC and the DCDQ. She identified that the connection of these generated large numbers of false positives and negatives. Joia (2014) found the same relationship, as did Souza (2016), proving that the instruments should be used concomitantly, in order to offer an accurate diagnosis. Since the MACB evaluates capacity and the DCDQ evaluates performance, encompassing criteria A and B of DSM V.
The DCDQ is a questionnaire answered by parents; has a self-administered format, i.e., when used as interview, enables interviewer bias. In this study, the questionnaire was given to parents for individual answers, without researcher interference ,. It is worth mentioning that is not common in Brazilian culture, answering survey questionnaires and return them to the researcher, for this reason there may be changes in the quality of responses (Silva, 2014).
It is also important to mention the size of Brazil which provides cultural differences and use of regional expressions, which could interfere with the understanding of parents about the issues (Silva, 2015; Joia, 2014).
Another point to consider is the lack of cultural adaptation of the cutoff point, since the questionnaire was culturally adapted but still uses the Canadian cut grade. Joia (2014), in his study, established a new cut-off point, using the ROC curve. The Canadian court score for 7 years old is 46 points, and the Brazilian court grade would be 49 points, justifying the high prevalence found in several studies. Being a single study, it cannot establish this note at national level, but highlights the importance of further studies.
Souza (2016) also proposed, in his study, a review in the points of cut currently used in Brazil. The DCDQ - Brazil and the MABC were applied to 100 children from 8 to 10 years of age, proposing a new cut from the ROC curve with the results of the two instruments. For children 8 years old the new cut grade would be ≤ 47, less than Canadian that is ≤ 49. The same happens with the cut grade for children of 10 years, where the Brazilian grade would be ≤ 52, different from the Canadian grade ≤ 57. These findings demonstrate the need for a study to establish a Brazilian cut note, since this disparity makes it difficult to accurately diagnose the disorder.
Regarding the prevalence of DCD in relation to gender, this study found no significant difference between the presence of signs in both boys and girls, the percentage found is very similar between genders (31% girls and 28% boys). This same result was found in the study of Joia (2014) and Silva (2015), but other studies show a higher incidence of DCD in boys (Giagazoglou et al., 2011).
Some studies were significantly related to the low economic class with motor difficulties (Grantham-Mcgregor et al., 2007; Assis-Madeira & Blascovi-Assis, 2013). The data from this study confirm this hypothesis. It can be observed a higher concentration of children with DCD signs in classes B and C. This factor may be related to the motor experiences that the individual passed, depending on the socio-cultural factors that surround him.
This study found a higher prevalence of DCD signs in children over 8 years (37%), and a prevalence of 15% in children 5-7 years. This difference can be explained by the difficulty in diagnosing DCD in younger children. The EACD (Blank et al, 2012) guides DCD diagnose in children of school age, i.e., over five years old. During this period the motor skills are already more stable, and the level of participation increases in activities of daily living; academic requirements reach a more sophisticated level and socialization plays a key role in building self-esteem.
Among the limitations of this study, the criteria A, C and D were evaluated by structured questionnaire, not following the recommendations of the EACD, which recommends the use of standardized instruments and a multi professional team. Another limitation concerns the low rate of return of the questionnaires sent to the parents, considering all the notes made above. We also point to the difficulty of parents and caregivers in answering the questionnaires, since they needed to compare their child to a peer of the same age and to establish if he had a performance that was remarkably similar to that of his child.
CONCLUSIONS
The present study found a prevalence of probable DCD of 30%. This is not a simple disorder to diagnose, since it requires a set of conditions, such as the effort of a multidisciplinary team, a series of evaluations and the combination of these assessments with the clinical observation of these professionals to identify the disorder.
This study used, based on the DSM - IV, assessing directly only the criterion B. For this reason, we have not found the prevalence of DCD, but the prevalence of disorder signs. The other criteria were checked indirectly through the DCDQ for parents. However, it emphasizes the importance of following all the criteria established by DSM, noting that today DMS - 5 more often used.
It may be noted in this study the need to reassess the DCDQ - Brazil in its semantics and vocabulary, as it was observed that parents had difficulty in understanding some items of the questionnaire. The DCD significantly influences the performance of daily activities of the child, as previously mentioned. The child signs are perceived as difficulty in action planning, organization, implementation and/or modification of their movements and learn new skills. That is, various motor aspects can be affected, making it a very heterogeneous disorder, complicating it identification and treatment. In addition, negatively reflecting on the construction and consolidation of self-esteem and the child's sense of competence.
Early diagnosis of DCD is essential because it can enable the education and guidance of all actors present in the children's daily lives, thus avoiding negative impacts on the day-to-day. Finally, the importance of the role of occupational therapist in the composition of the multidisciplinary team that will evaluate and diagnose DCD is highlighted, considering that the disorder significantly affects the activities of daily living and should be directed to the intervention as early as possible.
REFERENCES
Agresti, A. (2002) Categorical data analysis. Second edition. New York: John Wiley & Sons. [ Links ]
APA. American Psychiatric Association (2002). DSM–IV: Manual diagnóstico e estatístico de transtornos mentais: DSM - IV. Porto Alegre: Artes Médicas. [ Links ]
APA. American Psychiatric Association (2014). Manual Diagnóstico e estatístico de Transtornos mentais: DSM - 5. Porto Alegre: Artes Médicas. [ Links ]
Asonitou, K., Koutsouki, D., Kourtessis, T., & Charitou, S. (2012). Motor and cognitive performance differences between children with and without developmental coordination disorder (DCD). Research in Developmental Disabilities, 33(4), 996–1005. https://doi.org/10.1016/j.ridd.2012.01.008 [ Links ]
Assis-Madeira, E. A., Carvalho, S. G., & Blascovi-Assis, S. M. (2013). Desempenho funcional de crianças com paralisia cerebral de níveis socioeconômicos alto e baixo. Revista Paulista de Pediatria, 31(1), 51-57. https://doi.org/10.1590/S0103-05822013000100009 [ Links ]
Associação Brasileira de Empresas de Pesquisa (2012). Critério de Classificação Econômica Brasil. Disponível em: www.abep.org/novo/Content.aspx?SectionID=84 Acesso em: 12 jun. 2013. [ Links ]
Berns, R. M. (2002). Desenvolvimento da criança. Editora Loyola: São Paulo. [ Links ]
Blank, R., Bouwien, S. E., Polatajko, H., & Wilson, P. (2012) European Academy for Childhood Disability (EACD): recommendations on the definition, diagnosis and intervention of developmental coordination disorder (long version). Developmental Medicine & Child Neurology, 54(1), 54-93. https://doi.org/10.1111/j.1469-8749.2011.04171.x [ Links ]
Cairney, J., Hay, J., Mandigo, J. J., Wade, T., Faught, B. E., & Flouris, A. (2007). Developmental coordination disorder and reported enjoyment of physical education in children. European Physical Education Review, 13(1), 81-98. https://doi.org/10.1177/1356336X07072678 [ Links ]
Cardoso A. C., & Magalhães L. C. (2012). Validade de critério da Avaliação da Coordenação e Destreza Motora. Revista Brasileira de Fisioterapia, 16(1), 16-22. [ Links ]
Civetta, L. R., & Hillier, S. L. (2008). The developmental coordination disorder questionnaire and movement assessment battery for children as a diagnostic method in Australian children. Pediatric Physical Therapy, 20(1), 39-46. https://doi.org/10.1097/PEP.0b013e31815ccaeb [ Links ]
Ferreira, L. F., Nascimento R. O., Apolinário M. R., & Freudenheim A. M. (2006). Desordem da coordenação do desenvolvimento. Motriz, 12(3), 283-292. [ Links ]
Franca, A. S., Matias, R., Real, M. H. C., Vale, A. D. L., Pacheco, M. A. V., Clase, J. P. D., ... Araujo, C. R. S. (2015). Motor coordination and attentional problems in school-aged children in a low-income population from northeastern Brazil. Journal of Comorbidity, 5(2), 81. http://dx.doi.org/10.15256/joc.2015.5.52 [ Links ]
França, C. de. (2008). Desordem coordenativa desenvolvimental em crianças de 7 e 8 anos de idade (Dissertação Mestrado em Ciências do Movimento Humano). Universidade do Estado de Santa Catarina, Santa Catarina. Retrieved from http://tede.udesc.br//handle/handle/381 [ Links ]
Giagazoglou P., Kabitsis, N., Kokaridas, D., Zaragas, C, Katartzi, E., & Kabitsis, C. (2011). The movement assessment battery in Greek preschoolers: the impact of age, gender, birth order, and physical activity on motor outcome. Research in Disabilities, 32(6), 77-82. http://dx.doi.org/10.1016/j.ridd.2011.06.020 [ Links ]
Grantham-McGregor, S., Cheung Y. B., Cueto, S, Glewwe, P., Richter, L., & Strupp, B. (2007). Developmental potential in the first 5 years for children in developing countries. Lancet, 369(9555), 60-70. http://dx.doi.org/10.1016/S0140-6736(07)60032-4 [ Links ]
Instituto Brasileiro de Geografia e Estatística, Diretoria de Pesquisas, Coordenação de População e Indicadores Sociais (2014). NOTA 1: Estimativas da população residente com data referência 1º de julho de 2014 publicadas no Diário Oficial da União em 28/08/2014. Disponível em: http://www.cidades.ibge.gov.br/xtras/temas.php?lang=&codmun=354890&idtema=130&search=sao-paulo|sao-carlos|estimativa-da-populacao-2014-. Acessado em: 22/06/2015. [ Links ]
Jóia, A. F. (2014). Transtorno do Desenvolvimento da Coordenação em crianças de 7 anos de idade matriculadas em escolas públicas no município de Araraquara – SP (Dissertação de Mestrado em Terapia Ocupacional). Universidade Federal de São Carlos, São Carlos. [ Links ]
Lingman, R., Hunt L., Golding J., Jongmans, M., & Emond, A. (2009). Prevalence of Developmental Coordination Disorder using the DSM-IV at 7 years of Age: a UK population – based study. Pediatries,123(4), 692-700. https://doi.org/10.1542/peds.2008-1770 [ Links ]
Magalhães, L. C., Rezende, M. B., Amparo, F., Ferreira, G. N., & Renger, C. (2009). Problemas de coordenação motora em crianças de 4 a 8 anos: levantamento baseado no relato de professores. Revista de Terapia Ocupacional da Universidade de São Paulo, 20(1), 20-28. http://dx.doi.org/10.11606/issn.2238-6149.v20i1p20-28 [ Links ]
Miranda, T. B., Beltrame, T. S., & Cardoso, F. L. (2011). Desempenho motor e estado nutricional de escolares com e sem transtorno do desenvolvimento da coordenação. Revista Brasileira de Cineantropometria & Desempenho Humano, 13(1), 59-66. http://dx.doi.org/10.5007/1980-0037.2011v13n1p59 [ Links ]
Missiuna, C., Gaines, R., Mclean, J., LeLaat, D., Egan, M. E., & Soucie, H. (2011). Description of children identified by physicians as having developmental coordination disorder, Developmental Medicine & Child Neurology, 50(11), 839-844. http://dx.doi.org/10.1111/j.1469-8749.2008.03140.x [ Links ]
Missiuna, C., Pollock, N., Egan, M., DeLaat, D., Gaines, R., & Soucie, H. (2008). Enabling occupation through facilitating the diagnosis of Developmental Coordination Disorder. Canadian Journal of Occupational Therapy, 75(1), 26-34. -https://doi.org/10.2182/cjot.07.012 [ Links ]
Missiuna, C., Cairney, J., Pollock, N., Campbell, W., Russell, D. J., Macdonald, K., Cousins, M. (2014). Psychological distress in children with developmental coordination disorder and attention-deficit hyperactivity disorder. Research in Developmental Disabilities, 35(5), 1198–1207. https://doi.org/10.1016/j.ridd.2014.01.007 [ Links ]
Prado, M. S. S., Magalhães, L. C., & Wilson, B. N. (2009). Cross-cultural adaptation of the Developmental Coordination Disorder Questionnaire for Brazilian children. Revista Brasileira de Fisioterapia. 13(3), 236-43. http://dx.doi.org/10.1590/S1413-35552009005000024 [ Links ]
Silva, A. F. R. (2015). Prevalência do transtorno do desenvolvimento da coordenação em crianças de 7 anos de idade matriculadas em escolas públicas de Itirapina-SP (Dissertação de Mestrado em Terapia Ocupacional). Universidade Federal de São Carlos, São Carlos. [ Links ]
Silva, E. V. A., Contreira, A. R., Beltrame, T. S., & Sperandio, F. F. (2011). Programa de intervenção motora para escolares com indicativo de transtorno do desenvolvimento da coordenação - DCD. Revista brasileira de educação Especial, 17(1), 137-150. http://dx.doi.org/10.1590/S1413-65382011000100010 [ Links ]
Silva, J., & Beltrame, T. S. (2013). Indicativo de Transtorno do Desenvolvimento da Coordenação de escolares com idade entre 7 e 10 anos. Revista Brasileira de Ciências do Esporte, Florianópolis, 35(1), 3-14. http://dx.doi.org/10.1590/S0101-32892013000100002 [ Links ]
Souza, T. F. (2015). Critérios Diagnósticos para a Identificação do Transtorno do Desenvolvimento da Coordenação: Revisão Sistemática da Literatura (Trabalho de Conclusão de Curso de Especialização em Intervenção em Neuropediatria). Universidade Federal de São Carlos, São Carlos. [ Links ]
Souza, T. D. F. D. (2016). Especificidade e sensibilidade do Questionário de Transtorno do Desenvolvimento da Coordenação-Brasil para crianças de 8 a 10 anos (Dissertação de Mestrado em Terapia Ocupacional). Universidade Federal de São Carlos, São Carlos. [ Links ]
Wilson, B. N., Kaplan, B. J., Crawford, S. G., & Roberts, G. (2007). The Developmental Coordination Disorder Questionnaire 2007©(DCDQ07). Administrative manual for the DCDQ107 with psychometric properties. [ Links ]
Zwiker, J. G., Missiuna, C., Harris, S. R., & Boyd, L. A. (2012). Developmental coordination disorder: a review and update. Official Journal of the European Pediatric Neurology Society, 16(6), 573-581. http://dx.doi.org/10.1016/j.ejpn.2012.05.005 [ Links ]
Acknowledgments:
To research participants and CNPQ
Conflict of interest:
Nothing to declare.
Funding:
Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ)
Manuscript received at September 28th 2016; Accepted at April 2nd 2017
* Corresponding author: Rodovia Washington Luís, s/n, São Carlos - SP, 13565-905, Brasil E-mail: patriciadellabarba@yahoo.com.br














