Dietary habits and sleep patterns are predictors of adolescent health. Research indicates that approximately 11-30% of young people suffer from some form of sleep disorder (Blunden et al., 2012). Insomnia, in particular, is characterized by difficulty falling asleep and/or maintaining sleep, along with possible early awakenings, and significantly impacts the lives of those experiencing it, potentially leading to exhaustion and overindulgence (e.g., in eating) (Cunnington, 2013). The specific cause of insomnia is complex and challenging to identify. One risk factor for insomnia is being female, as young and adult women are more likely to develop insomnia than their male counterparts (Johnson, 2006). Additionally, factors like increasing age, tobacco, drug, and alcohol consumption (NHLBI, 2022), anxiety, depression (Strine & Chapman, 2005), and even smartphones excessive use/misuse (Van Deursen et al., 2015) could be risk factors for insomnia development. Research reveals that diet is a significant predictor of sleep quality and, therefore, can also be a cause of insomnia (Tan et al., 2015). Moreover, a high intake of sweets, sodas, and carbohydrates is associated with poor sleep quality, while a diet rich in fish, vegetables, and vitamin D is linked to better sleep quality (Tan et al., 2015).
Food addiction (FA) involves the consumption of highly palatable foods (i.e., foods high in sugar, salt, and fats) in quantities exceeding those necessary for maintaining homeostasis (Kalon et al., 2016). Therefore, this behaviour poses a risk for overweight and even obesity development (Falcon et al., 2021). FA is a clinical condition conceptualized in the context of substance dependence, involving a strong craving for the substance (i.e., food), loss of control over consumption, significant effort and time spent to obtain it, and inability to reduce or stop consumption (Torres et al., 2017).
Self-control is a skill that allows individuals to regulate and control their own behavioural, psychological, and physical processes in order to achieve a defined long-term goal (Blankstein & Polivy, 1982). The model proposed by Claudatos et al. (2019) aims to explain the bidirectional relationship between sleep disturbances-caused by external factors (e.g., increased screen time) and internal factors (e.g., changes in circadian rhythms)-and substance consumption in adolescents. This relationship can occur through three different pathways: 1) negative coping, 2) emotional dysregulation, and 3) reward seeking/weak impulse control.
The authors of the model argue that adolescence is marked by significant changes in sleep cycles, such as a preference for later bedtime (Claudatos et al., 2019). These changes occur due to shifts in young people's circadian rhythms influenced by environmental factors (e.g., early school start times), developmental factors (e.g., increased autonomy in managing their routines compared to childhood), and behavioural factors (e.g., reduced sleep time during the week compensated by longer sleep on weekends) (Wolfson & Carskadon, 1998). Moreover, sleep deprivation impairs inhibitory processes, affecting teenagers' behaviour and self-control, potentially leading to risky behaviours, such as consuming highly caloric foods (Claudatos et al., 2019). This relationship can create a vicious circle since addictive consumption of high-calorie foods may impact sleep, particularly its quality and interruptions (Claudatos et al., 2019). Negative coping is a mechanism that catalyses this relationship, as adolescents may consume substances as a coping mechanism to promote sleep (Goodhines et al., 2017), which might induce excessive consumption and have the opposite effect, disrupting sleep itself (Claudatos et al., 2019).
Regarding emotional dysregulation, it is known that sleep uniquely contributes to emotional recalibration and functioning (Walker et al., 2009). Therefore, sleep deprivation could impair emotional experience regulation. Adolescents in this situation might be more vulnerable to neurobiological changes in emotional regulation and reward response, diverging from those occurring in normal development of adolescents who have no sleep disorder/insomnia (Volkow et al., 2012). Thus, young people with varying circadian rhythms throughout the week may be more susceptible to reduced behavioural and emotional self-regulation, making them more prone to substance consumption (Claudatos et al., 2019). Additionally, concerning reward seeking/weak impulse control, adolescents undergo a crucial phase in the development of structures essential for the reward cycle's functioning, also involved in mood and behaviour, which can lead to alterations in reward functioning and impulse control (Clark et al., 2008). These changes can make them more vulnerable to initiating substance consumption (Romer et al., 2009).
To date, it is known that FA is related to weak emotional regulation (Kozak et al., 2017) and impulsivity (Kalon et al., 2016). However, there is still limited information on how it affects young people's sleep. FA conceptualization is based on the substance dependence model (Torres et al., 2017). Therefore, this research builds upon the conceptual model developed by Claudatos et al. (2019) with the aim of exploring the unidirectional relationship between FA and insomnia. Specifically, it seeks to understand how FA predicts insomnia and how self-control (both functional and dysfunctional) mediates this relationship.
Method
Participants
Initially, the sample comprised 1672 young individuals from Madeira, out of which 106 participants were excluded due to not providing consent (n = 56), not indicating their biological sex (n = 10), not meeting the specified age criteria (n = 20), or not providing reliable information for weight percentile calculation (n = 20). The final sample consisted of 1566 participants eligible for this study, with an average age of 14.79 (SD = 1.89). Inclusion criteria involved being a student in the Autonomous Region of Madeira and aged between 12 and 19 years. Thus, out of a total of 17,989 students attending the 3rd cycle of basic education and secondary education in Madeira during the academic year 2019/2020, 1566 students were eligible for this study. Consequently, the sample represents 8.72% of the Madeiran student population in the 3rd cycle of basic education and secondary education in the 2019/2020 public education year (DREM, 2023). The characteristics of the participants are shown in Table 1.
Table 1 Participants’ characteristics
| Characteristics | Adolescents (n = 1566) |
|---|---|
| n (%) | |
| Sex | |
| Males | 742 (47.4) |
| Females | 824 (52.6) |
| Level of Education | |
| Basic Education (3rd cycle) | 854 (54.5) |
| Secondary Education | 712 (45.5) |
| Residential Areas | |
| Urban Areas | 1178 (75.2) |
| Rural Areas | 388 (24.8) |
| Academic Performance | |
| Students with very good grades | 194 (12.4) |
| Students with good grades | 680 (43.4) |
| Students with sufficient grades | 635 (40.5) |
| Students with negative grades | 57 (3.6) |
| Academic Retention | |
| Students who had never been retained | 1155 (73.8) |
| Students who had been retained in one or more years | 411 (26.2) |
Measures
Sociodemographic Data. Sociodemographic measures included biological sex, age, residential area, level of education, academic performance, height, and weight.
Yale Food Addiction Scale (P-YFAS). This scale consists of 24 self-report items assessing addictive eating behaviours occurring over the past year (e.g., "I felt sluggish or tired from overeating."; Torres et al., 2017). The YFAS was developed according to the criteria for substance dependence disorder described in the DSM-IV-TR , which were adapted to food behaviour, resulting in seven criteria: 1) consuming larger amounts or for longer periods than intended (items 1, 2, 3); 2) inability to reduce or stop certain foods' consumption (items 4, 22, 24); 3) spending significant time and effort on food consumption (items 5, 6, 7); 4) giving up important social activities (items 8, 9, 10, 11); 5) persistent behaviour despite knowledge of its physical and psychological consequences (item 19); 6) tolerance (items 20, 21); and 7) withdrawal (items 12, 13, 14). Higher scores indicate more symptomatic expression consistent with a FA pattern. The scale provides continuous scores indicating the number of checked addiction symptoms. The first 23 items are rated on a 5-point Likert scale ranging from 0 “never” to 4 “4 or more times per week, or daily”, and the last item on a 5-point Likert scale ranging from 1 “1 or fewer times” to 5 “5 or more times”. The scale also has a dichotomous scoring system indicating whether a person exhibits symptomatic expression similar to a situation of FA (yes/no) if they have at least 3 symptoms and report clinically significant impairment. In this study, the continuous scoring method was used. The scale demonstrated good internal consistency for the Portuguese population, with α=.82, indicating its reliability (Torres et al., 2017).
Brief Self-Control Scale (BSCS). This scale assesses self-control and consists of 12 items rated on a 5-point Likert scale ranging from 1 "Not at all like me" to 5 "Very much like me". It has two dimensions: Maladaptive/Dysfunctional Self-Control (items 2, 3, 4, 5, 9, 10, 12, 13) (e.g., "I say inappropriate things."; Água et al., 2020) and Adaptive/Functional Self-Control (items 1, 6, 8, 11) (e.g., "People would say I have strong self-discipline."; Água et al., 2020). To calculate the total score, items related to the first dimension were reversed, so that a higher score corresponds to more adaptive self-control. The Maladaptive and Adaptive Self-Control dimensions demonstrated good and acceptable internal consistency, with α=.86 and α=.68 respectively, indicating the instrument's reliability (Água et al., 2020).
Athens Insomnia Scale (AIS). This scale assesses the level of experienced insomnia and consists of 8 items (e.g., "Difficulty in initiating sleep."; Soldatos et al., 2000), corresponding to criteria A, B, and C of the International Classification of Diseases - 10 (ICD-10) insomnia diagnosis. Criterion A assesses difficulty initiating sleep, nocturnal awakenings, early morning awakenings, overall sleep quality, and sleep duration. Criterion B refers to the frequency of these events, with a minimum of at least 3 times per week over the last month. Finally, criterion C corresponds to the daily repercussions experienced due to lack of sleep (e.g., well-being, physical and mental functionality, and perceived sleepiness). Each item is rated on a 4-point Likert scale, ranging from 0 "No Problem at All" to 3 "Very Serious Problem". Total scores range from 0 (absence of insomnia) to 24 (severe insomnia level), with total scores equal to or higher than 6 indicating a symptomatic expression consistent with insomnia (Soldatos et al., 2003). Regarding internal consistency, the AIS-8 exhibited a value of α=.82 in validation for the Portuguese population, indicating good internal consistency and the scale's reliability (Lamelas et al., 2023).
Procedure
The research project was approved by the Ethics Committee of ISPA - University Institute and by the Regional Secretariat of Education, Science, and Technology of the Regional Government of Madeira. Subsequently, various public schools in Madeira were contacted to request permission to distribute online questionnaires to students in basic and secondary education. Prior to participation, informed consent was obtained from the young individuals, and an Informed Consent form was sent to the legal guardians of students under 16 years old, in collaboration with the Regional Secretariat of Education, Science, and Technology of the Regional Government of Madeira. After obtaining informed consents and ensuring compliance with inclusion criteria, students completed the questionnaire in the classroom setting. The research adhered to the Deontological Code of the Ordem dos Psicólogos Portugueses (2021) and the principles of the American Psychological Association (2017) regarding ethical treatment of participants.
Results
Initially, the sample was analysed to provide a general characterization of the percentiles, insomnia levels, and FA among the students. Regarding percentile evaluation, generally, the students predominantly had normal weight, with a total of 1116 (71.3%) students, followed by 215 (13.7%) students classified as overweight, 181 (11.6%) with obesity, and 54 (3.4%) underweight. Concerning insomnia levels, the sample had a mean of 4.45 (SD = 3.88), with a minimum of 0 and a maximum of 23, indicating that the majority of the young individuals in this sample, specifically 1072 (68.5%) young people, did not show symptomatic expression consistent with insomnia. However, 494 (31.5%) young people exhibited insomnia levels equal to or greater than 6, indicating symptomatic expression consistent with insomnia, revealing that a significant portion of students still experiences mild, moderate, or severe insomnia. Regarding FA (Food Addiction) levels, the mean was 2.85 (SD = 2.10), with a minimum of 0 and a maximum of 8 symptoms identified consistent with those presented in cases of FA. In general, young individuals exhibited only 2 symptoms consistent with those experienced in FA, with a total of 776 (49.6%) young people in this situation. However, the remaining 790 (50.4%) young people exhibited 3 or more symptoms consistent with those experienced in FA, indicating a high number of adolescents in this situation.
Subsequently, a simple linear regression model was conducted, with insomnia as the dependent variable and FA as the independent variable. The linear regression model revealed that FA is positively and significantly associated with insomnia (r = .23, p < .001). Furthermore, another complementary linear regression model was performed, adding the variables gender and age, as shown in Table 2. In this model, it was observed that in addition to the previously identified relationship between FA and insomnia, there is also a positive and significant relationship between sex and insomnia (r = .11, p < .001). This indicates that females are more prone to insomnia compared to their male counterparts. Conversely, there is no significant relationship between age and insomnia (r = .05, p = .049).
Table 2 Regression Coefficients of FA on Insomnia. Simple linear regression model of the correlation between FA (independent variable) and insomnia (dependent variable) with age and gender as covariates (total sample with male and female youth)
| Variable | B | β | SE | p |
|---|---|---|---|---|
| Constant | 5.05 | .79 | <.001 | |
| FA | .07 | .23 | .01 | <.001 |
| Sexa | .88 | .11 | .18 | <.001 |
| Age | .09 | .05 | .05 | .049 |
| Dysfunctional Self-control | .16 | .27 | .02 | <.001 |
| Functional Self-control | -.05 | -.05 | .03 | .061 |
| R2 | .19 |
Note. n=1566. The impact of FA on insomnia was examined, with the covariates being gender and age, as well as the variables dysfunctional self-control and functional self-control. aMen/boys = 1, Women/girls = 2. FA=Food Addiction
The mediation analysis was conducted using the SPSS PROCESS macro v4.2. Each model was generated with a 95% confidence interval, based on 10,000 bootstrap samples. The parallel mediation model presented in Table 3 reveals a significant positive direct effect of FA on insomnia (c’ = .07, p < .001). Additionally, there is a positive indirect effect of FA on insomnia, mediated by the dimension of Dysfunctional Self-Control - related to impulsivity (a 1 = .22). Conversely, a non-significant indirect effect of FA on insomnia was observed when mediated by the dimension of Functional Self-Control - related to self-discipline (a 2 = -.02), indicating that this is a mediator to be disregarded. The significance of the mentioned effects is determined by the exclusion of 0 from the confidence interval. The model is schematically represented in Figure 1.
Table 3 Parallel mediation of the correlation between food addiction (independent variable) and insomnia (dependent variable) with age and sex as covariates (total sample of male and female youth).
| Direct effect of FA on insomnia | SE | LLCI | ULCI | |
| .07*** | .01 | .05 | .08 | |
| Mediators | Indirect effects of FA on insomnia | BootSE | BootLLCI | BootULCI |
| Dysfunctional Self-control | .04*** | .00 | .03 | .04 |
| Functional Self-control | -.00 (NS) | .00 | -.00 | .00 |
Note. n=1566. SE = standard error; LLCI = lower limit of the confidence interval; ULCI = upper limit of the confidence interval; BootLLCI = lower bootstrap limit of the confidence interval; BootULCI = upper bootstrap limit of the confidence interval. ***p <.001; NS = nonsignificant
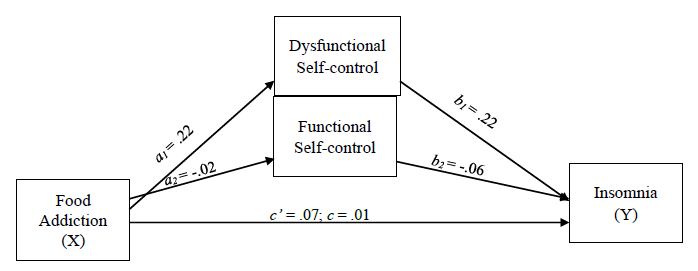
Figure 1 Schematic representation of the parallel mediation model of the correlation between food addiction (independent variable) and insomnia (dependent variable) with age and sex as covariates.
The above-mentioned mediation model has a total explained variance of 19% (R adj 2 = .19), indicating that 19% of the variance in insomnia is explained by FA and the dimension of dysfunctional self-control. In other words, a partial mediation of dysfunctional self-control in the relationship between insomnia and FA was observed.
This implies that dysfunctional self-control - associated with impulsivity - enhances the influence that FA has on insomnia. On the other hand, functional self-control - associated with self-discipline - does not interfere in the relationship between FA and insomnia.
Discussion
This study aimed to understand how FA can help explain insomnia in young people from Madeira, mediated by the variable of self-control. This research is particularly relevant as sleep-wake cycles and eating habits are regulated by circadian rhythms (Najem et al., 2019). Disruptions in circadian rhythms can be a risk factor for physical conditions like obesity (Kandeger et al., 2018) and psychological conditions like depression (Armitage, 2007). Circadian rhythms are also related to the reward system (Murray et al., 2009). Therefore, disturbances in circadian rhythms could affect inhibitory control, enhance impulsivity, and increase the seeking of rewards, reinforcing substance (e.g., food) consumption (Tashjian et al., 2017).
This study found that FA helps explain insomnia in young adolescents when their self-control tendencies lean towards dysfunctionality, indicating higher impulsivity and spontaneity (Lindner et al., 2015). Conversely, functional self-control, which is associated with self-discipline, resilience, and thoughtfulness (Lindner et al., 2015), does not mediate the relationship between FA and insomnia. This suggests that dysfunctional self-control is a risk factor for both FA development and subsequent insomnia.
The results of this study align with previous research in this area and support the theoretical model proposed by Claudatos et al. (2019), demonstrating a unidirectional relationship between FA and insomnia. This relationship was also found in a study by Najem et al. (2019), where FA was associated with poorer sleep quality. Given that FA involves impulsive consumption of certain foods, it is naturally related to an individual's self-control (Luo et al., 2022). Higher levels of self-control are associated with increased self-efficacy and can reduce impulsivity, preventing excessive consumption (Wang et al., 2015). Conversely, lower self-control levels are linked to higher impulsivity, increasing the risk of developing FA (Minhas et al., 2021).
Moreover, uncontrolled consumption of certain foods can serve as a regulatory mechanism, allowing individuals to manage negative emotions (Lou et al., 2022). Individuals experiencing anxiety and depression tend to consume highly palatable foods as a way to alleviate their negative or depressed mood (Oliveira et al., 2020), highlighting the association of FA with impulsivity and mood (Kalon et al., 2016). Furthermore, chronic stress can exacerbate the dysregulation of the reward system, increasing the risk of developing FA (Wei et al., 2019).
Additionally, research has shown that the prevalence of FA among adolescents ranges from 2-16% (Rodrigue et al., 2019). These prevalence rates are influenced by cultural factors and can vary across populations (Luo et al., 2022). In a country like Portugal, with a rich culinary tradition, people might perceive consuming large quantities of food as acceptable, whereas in other countries, it might be considered excessive and characteristic of FA (Torres et al., 2017). In this sample, approximately half, specifically 776 (49.6%) young individuals, exhibited only 2 symptoms consistent with FA. However, the concern lies with the other half; the remaining 790 (50.4%) young individuals showed 3 or more symptoms consistent with those experienced in FA, a significantly high figure.
Regarding insomnia, 1072 (68.5%) young individuals did not exhibit symptoms typical of insomnia. However, 494 (31.5%) young individuals showed symptoms consistent with insomnia, indicating a substantial portion of students experiencing mild, moderate, or severe levels of insomnia. Thus, despite half the sample displaying mild levels of FA and the other half showing moderate to high levels, with the majority not exhibiting symptoms indicative of insomnia, the partial mediation of dysfunctional self-control in the relationship between FA and insomnia is pronounced. This suggests that in cases of very high FA prevalence, this relationship could be even more pronounced, leading to significantly higher insomnia levels.
As previously mentioned, it was also observed that females experience higher levels of insomnia, in line with Johnson's (2006) findings that the female biological sex (being a women) could be a risk factor for insomnia development. This may be explained by the pubertal development that young females experience during this phase (Zhang et al., 2016).
Despite providing valuable insights, this study has limitations. The inclusion of participants solely from the Autonomous Region of Madeira may have made the sample peculiar and distinct, with the region's cultural traits potentially influencing the variables under study. Future studies should aim to include Portuguese youth from across the country, including both mainland and other islands. Additionally, the online nature of the questionnaire, without the presence of a researcher, might have hindered clarification of participant doubts. Furthermore, the option to skip certain questions could have led participants to omit answers in specific parts of the questionnaire.
Nonetheless, this study has notable strengths. It is among the first to consider self-control as a mediator in the relationship between FA and insomnia. Moreover, the study was conducted with a sample that represents 8.72% of the student population in the Autonomous Region of Madeira in the 3rd cycle of basic education and secondary education in the 2019/2020 school year, which, despite appearing small, adds value to the study due to the substantial sample size (i.e., 1566 participants) and represents nearly 10% of the population under study.
The main conclusion of this study emphasizes the role of dysfunctional self-control as a driver in the relationship between FA and insomnia, partially amplifying FA's influence on insomnia. Simultaneously, functional self-control does not impact this relationship, meaning it does not shield individuals from initiating these addictive behaviours.
Thus, the results of this study highlight the importance of developing interventions for this age group, focused on dysfunctional self-control, particularly addressing juvenile impulsivity. Providing strategies aimed at promoting impulse control and pro-health decision-making is essential. Equally important is empowering young individuals and informing them about the importance of maintaining good sleep hygiene, explaining how circadian rhythms need to be aligned with individual needs to ensure optimal physical, emotional, cognitive, and mental functioning.















