Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Psicologia, Saúde & Doenças
versão impressa ISSN 1645-0086
Psic., Saúde & Doenças vol.17 no.1 Lisboa abr. 2016
https://doi.org/10.15309/16psd170111
Intergenerational impact of mental illness in juveniles with a history of victimization
Impacto intergeracional da perturbação mental em jovens com história de vitimação
Sofia Ribeiro* Miguel Basto-Pereira*, & Ângela Maia*
*Escola de Psicologia, Universidade do Minho, Braga, Portugal
Endereço para Correspondência
ABSTRACT
In Portugal, the Child Protection Services (CPS) followed 73,019 processes in 2014 alone, 1,452 more than the previous year. Portugal has the second highest prevalence of mental illness among the nine European countries evaluated; it is estimated that 42.7% of the population has at least one mental disorder throughout their life. Parental psychopathology is a risk factor for a set of seriously negative consequences in offspring, including mental health problems. The aim of this study is to explore the effects of parental mental disorder in the development of mental health among young people identified as victims of maltreatment. The sample in this study included 29 young adults aged between 18 and 25 years, identified as victims of abuse in childhood by the CPS. Our findings suggest that CPS identification of parental mental disorder statistically discriminates against these young adults in terms of general psychological distress and a set of Brief Symptom Inventory dimensions. Despite the detection of parental mental disorders and CPS intervention into families, mental health consequences were identified five years later. This study provides a set of politic recommendations on the protection of children and youth.
Keywords: intergenerational impact, adversity, victimization, mental disorder, Child Protection Services.
RESUMO
Ao longo do ano de 2014 foram acompanhados em Portugal 73019 processos de promoção e proteção, um aumento de 1452 processos desde o ano anterior. A prevalência de perturbações mentais ao longo da vida em Portugal é 42,7% apresentando a segunda prevalência mais elevada entre nove países da Europa. A perturbação mental dos pais tem sido associada a um conjunto de consequências negativas no desenvolvimento dos filhos, incluindo problemas psicológicos. Pretende-se explorar o efeito intergeracional da perturbação mental em jovens acompanhados por Comissões de Proteção de Crianças e Jovens (CPCJ) cuja perturbação mental dos pais foi detetada e a família alvo de intervenção. Participaram 29 jovens entre os 18 e os 25 anos (M=19 anos, DP=1,69), identificados quando menores pela CPCJ como maltratados. A presença de perturbação mental dos pais diferenciou estatisticamente os jovens ao nível da psicopatologia geral e de um conjunto de dimensões do BSI. Apesar da deteção da perturbação mental dos pais e do acompanhamento das famílias notam-se consequências na saúde mental dos filhos passados em média cinco anos. Deste estudo resulta um conjunto alargado de recomendações políticas na área da promoção e proteção da infância e juventude.
Palavras-chave: impacto intergeracional, adversidade, vitimização, perturbação mental, proteção da infância
Portugal has the second highest prevalence of mental illness among eight European countries, with an estimated 42.7% of the population suffering from at least one mental disorder throughout their life (Direção-Geral da Saúde, 2014). Parental psychopathology is a risk factor for a large set of adverse effects in offspring, including mental health problems (Atwoli, Nock, Williams, & Stein, 2014; Clark, Cornelius, Wood, & Vanyukov, 2004; Dougherty et al., 2013; Hirshfeld-Becker et al., 2012; Mars et al., 2012; McAdams et al., 2015; McLaughlin et al., 2012; Santana et al., 2015).
Some studies indicate intergenerational transmission of mental perturbation as shown when offspring have the same diagnoses as their parents (Clark et al., 2004), or a transmission of a general pattern of perturbation (Hirshfeld-Becker et al., 2012; McLaughlin et al., 2012). This relationship is independent of the diagnosed parents gender (Marmorstein, Malone, & Iacono, 2004; McLaughlin et al., 2012) and the gender of the offspring (McLaughlin et al., 2012). The risk for the offspring is greater when both parents have mental problems (Marmorstein et al., 2004; McLaughlin et al., 2012). The parental diagnosis also affects the severity of the descendent mental illness (Atwoli et al., 2014).
Different mechanisms of intergenerational transmission of psychopathology were suggested. Transmission of genetic vulnerability from one generation to another can partly explain this occurrence; however, studies with twins and adopted brothers point to a transmission resulting from environmental factors (McAdams et al., 2015). Negative parenting practices as a result of mental disorders; simple exposure to the symptoms of the parents; and learning by modelling and imitation may be sources of intergenerational transmission of mental disorder (McAdams et al., 2015; McLaughlin et al., 2012).
A two-way effect has been suggested, i.e. the perturbation of the offspring may also be associated with a worse prognosis for parents (McAdams et al., 2015). Because parents and children have a common family environment, we can consider the diagnoses of both parents and children to have the same genesis and be related to factors or events inherent in family dynamics (McAdams et al., 2015).
Sometimes, the parents' mental disorder coexists with other forms of adversity in the family environment - such as child abuse and violence - and these negative dynamics alone have been associated with mental disorder of children (Green et al., 2010; Sugaya, Hasin, & Olfson, 2012). In Portugal, during the year 2014, the Child Protection Services (CPS) followed 73,019 processes, an increase of 1,452 from the previous year (Comissão Nacional de Proteção de Crianças e Jovens em Risco, 2015).
Researchers have noted the need for preventive intervention for children of parents with mental disorder (Santana et al., 2015). Therefore, there is a need to explore psychopathological symptoms in young people whose family has a history of mental disorder, and also for intervention in the family.
The aim of this study is to explore the effect of parental mental disorder in the development of mental health in young people identified as victims of abuse. We hypothesized that young victims of maltreatment, who are at the same time offspring of parents with mental illness, have higher levels of psychopathology when they enter into adulthood compared with others young adults who are identified by CPS as maltreated but without official records of parental mental disorder.
METHOD
Participants
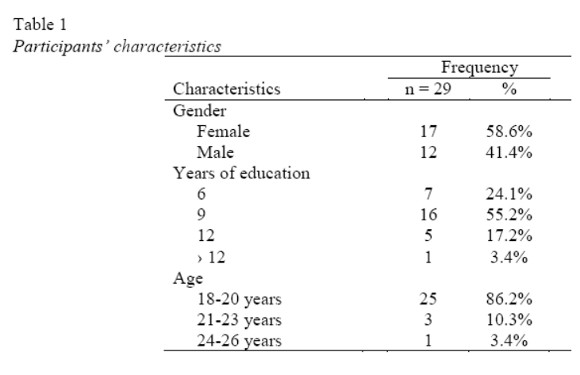
We consulted and screened 328 processes to get contacts and/or addresses. Of the 328 processes, it was impossible to make contact in 73 cases, for the following reasons: the process didnt have contacts; the addresses were outdated; absence abroad, death, prison or disability; other reasons which did not allow participation in this study. We contacted 255 young people and invited them to participate in the study. Twenty-nine young adults responded and agreed to participate (Table 1 ). The participants were aged between 18 and 25 years (M = 19 years, SD = 1.69; 12 males and 17 females) who the CPS identified as victims of maltreatment. When the processes were initiated the participants were between 7 and 17 years (M = 13.24 years, SD = 2.49).
Measures
Checklist for data collection processes. The Portuguese version (Silva & Maia, 2008) of the Family Adverse Childhood Experience Questionnaire was used (Felitti et al., 1998). This checklist was used in order to collect information from the official processes of the CPS, such as a family member with mental illness or the suicide of a family member. The dimension of parental mental illness is measured by a dichotomous score of "zero" (no mental disturbance registration or suicide of any member of the family) or "one" (mental disturbance recording and/or suicide of at least one family member).
Brief Symptom Inventory (Derogatis, 1993). The Portuguese version was adapted by Canavarro (1995). This instrument evaluates psychopathological symptoms in nine dimensions: somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism (Canavarro, 1999). The participants classified, through 53 items, the degree to which each problem bothered them during the last week on a five-point Likert-style response scale. The average score of all items corresponds to the General Symptom Index (GSI). The Portuguese version of the Brief Symptom Inventory showed satisfactory internal reliability, with Cronbachs alpha ranging between 0.72 and 0.85 (Canavarro, 1999).
Procedure
This study was approved by the CPS, the National Commission for the Protection of Children and Young Persons at Risk, and the Ethics Committee of the University of Minho. The data was collected from the CPS in North Portugal. There was a period of 5.21 years (mean time) between the opening protection procedures and the time of our evaluation. Invitations to participate were carried out by letter, telephone, or personally through those responsible for the child protection process. Participants gave informed consent and signed a document that explained how all the research would be done and requesting authorization for access to official CPS records.
The questionnaires were performed individually in a quiet and private room. The objectives were individually explained and all questions were clarified. The information from the CPS records was collected for our checklist. Data collection processes involved the reading of all the records and attached files, including statements, CPS reports, health service reports, school reports and police reports.
Data was statistically analyzed using the Statistical Package for Social Sciences (SPSS) software (Version 22.0; IBM, 2013). Data analysis included descriptive statistics for the calculation of the prevalence of parental mental disorder in the CPS process. The statistical differences in psychopathological symptoms between young adults with both CPS processes and parental mental illness records, and young adults with CPS processes and no record of parental mental illness, were analyzed using the Mann-Whitney test.
RESULTS
The prevalence of parental mental disorder, based on the CPS process, was 37.9% (n=11).
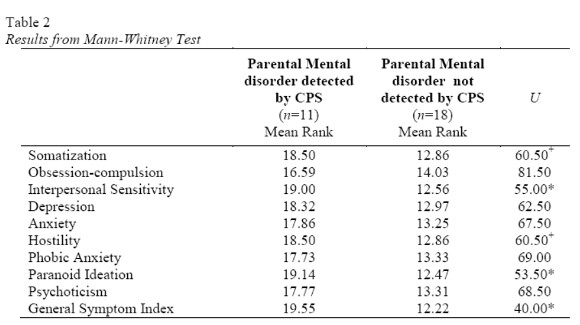
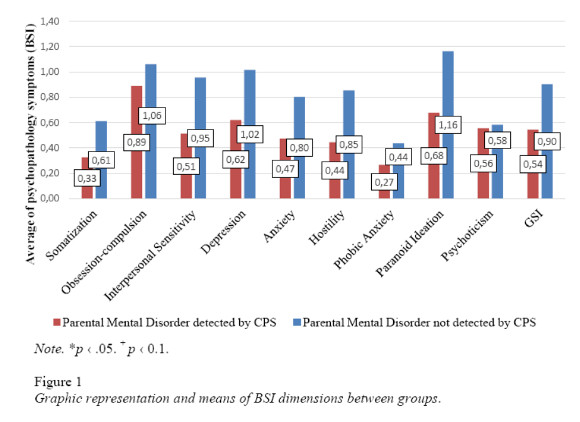
Young adults with parental mental disorder in CPS records have significantly higher levels of GSI (U = 49.00, p <.05), paranoid ideation (U = 53.50, p <.05) and interpersonal sensitivity (U = 55.00, p <.05) symptoms when compared with young adults with CPS processes without identified parental mental disorders (see Table 2). In 8 of the 9 BSI dimensions, the average of the symptoms was about twice as high for children of parents with a mental disorder (Figure 1).
DISCUSSION
To the best of our knowledge, this is the first longitudinal retrospective study which explores the effect of parental mental disturbance in the mental health of young people identified as maltreated at an early age by CPS records. This study had access to the parental mental disorder records of young people identified five years ago as maltreated, and to the psychopathological symptoms in early adulthood of these young people. This research is consistent with previous studies showing that the mental disorder of parents is associated with psychopathological symptoms in offspring (Atwoli et al., 2014; Dougherty et al., 2013; Hirshfeld-Becker et al., 2012; McAdams et al., 2015; Santana et al., 2015). The mean of most psychopathological symptoms assessed by the BSI is approximately twice for young people with parental mental disturbance registration, compared with young people whose parents dont have a mental disturbance record.
Victimization in childhood is itself a recognized risk factor for the development of psychopathological symptoms (Green et al., 2010; Sugaya et al., 2012). This study adds that the coexistence of victimization with parental mental disorder aggravates this risk, since the average of each dimension of the BSI is higher when compared with young people also identified as abused, but whose parents do not have a mental disorder record.
Although family intervention took place when parental mental disorder of participants was detected, nevertheless, even after an average of five years, there were still effects on the lives of these youths. This study offers a wide range of politic recommendations in the area of promotion and protection of children and youths. It seems pertinent to improve the screening tools and referral of CPS cases and to extend the same measures to all members of the family. Close cooperation between the CPS and mental health services appears to be essential for more effective and preventive intervention with children of parents with mental illness. These interventions may provide youths with personal resources and coping strategies, which aim to prevent the intergenerational transmission of mental disorders and serious psychopathology symptoms. Government policies based on scientific knowledge can contribute to improvements on social, economic and public health levels.
This study had some limitations. The sample size was small and should be increased. In addition, the instrument used for the evaluation of the CPS records did not allow access to specific parental diagnosis and the type of intervention provided to the family; this access would be useful for future studies. Prospective longitudinal studies should be carried out in order to overcome the present limitations. Despite these limitations, this study was an excellent opportunity to explore the effect of the overlap of adversity with parental mental disorder.
Future studies should have a larger sample and collect more complete data from the CPS processes, such as the diagnoses of the parents and the types of intervention provided. This would allow an evaluation of the intervention and lead to further improvements in the monitoring of families with several problems.
This study suggests that the maltreatment of youth with parental mental disorder is an important risk factor for serious mental health problems from childhood to adulthood. Despite these limitations this study provides a set of practical recommendations and suggests unexplored directions for future studies.
REFERENCES
Atwoli, L., Nock, M. K., Williams, D. R., & Stein, D. J. (2014). Association between parental psychopathology and suicidal behavior among adult offspring: Results from the cross-sectional South African Stress and Health survey. BMC Psychiatry, 14, 65. doi:org/10.1186/1471-244X-14-65 [ Links ]
Canavarro, M. C. (1995). Inventário de sintomas psicopatológicas – BSI [Brief Symptom Inventory - BSI]. In M. R. Simões, M. M. Gonçalves, & L. S. Almeida (Eds.), Testes e Provas Psicológicas em Portugal (pp. 95–109). Braga: APPORT/SHO. [ Links ]
Canavarro, M. C. (1999). Inventário de sintomas psicopatológicos – BSI [Brief Symptom Inventory - BSI]. In M.R. Simões (Ed.), Complementaridade de dados do SPSS (pp. 588–593). Lisboa: Edições Sílabo [ Links ]
Clark, D. B., Cornelius, J., Wood, D. S., & Vanyukov, M. (2004). Psychopathology risk transmission in children of parents with substance use disorders. The American Journal of Psychiatry, 161, 685–91. doi:org/10.1176/appi.ajp.161.4.685 [ Links ]
Comissão Nacional de Proteção de Crianças e Jovens em Risco (2015). Relatório Anual de Avaliação da Atividade das CPCJ 2014 [Annual Report on evaluation of CPS activities 2014]. Retrieved from: http://www.cnpcjr.pt/preview_documentos.asp?r=5603&m=PDF [ Links ]
Derogatis, L. R. (1993). BSI Brief Symptom Inventory: Administration, Scoring, and Procedure Manual (4th ed.). Minneapolis, MN: National Computer Systems. [ Links ]
Direção-Geral da Saúde (2014). PORTUGAL Saúde Mental em números – 2014 [PORTUGAL Mental Health in numbers - 2014]. Retrieved from: https://www.dgs.pt/estatisticas-de-saude/estatisticas-de-saude/publicacoes/portugal-saude-mental-em-numeros-2014.aspx
Dougherty, L. R., Smith, V. C., Bufferd, S. J., Stringaris, A., Leibenluft, E., Carlson, G. A., & Klein, D. N. (2013). Preschool irritability: Longitudinal associations with psychiatric disorders at age 6 and parental psychopathology, Journal of the American Academy of Child and Adolescent Psychiatry, 52, 1–17. doi:org/10.1016/j.micinf.2011.07.011.Innate [ Links ]
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258. doi:org/10.1016/S0749-3797(98)00017-8 [ Links ]
Green, J. G., McLaughlin, K. A., Berglund, P. A., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67, 113–123. doi:org/10.1001/archgenpsychiatry.2009.186 [ Links ]
Hirshfeld-Becker, D. R., Micco, J. A., Henin, A., Petty, C., Faraone, S. V., Mazursky, H., Biederman, J. (2012). Psychopathology in adolescent offspring of parents with panic disorder, major depression, or both: A 10-year follow-up. American Journal of Psychiatry, 169, 1175–1184. doi:org/10.1176/appi.ajp.2012.11101514 [ Links ]
IBM Corp. Released 2013. IBM SPSS Statistics for Windows [Computer Software], Version 22.0. Armonk, NY: IBM Corp. [ Links ]
Marmorstein, N. R., Malone, S. M., & Iacono, W. G. (2004). Psychiatric disorders among offspring of depressed mothers: Associations with paternal psychopathology. American Journal of Psychiatry, 161, 1588–1594. doi:org/10.1176/appi.ajp.161.9.1588 [ Links ]
Mars, B., Collishaw, S., Smith, D., Thapar, A., Potter, R., Sellers, R., Thapar, A. (2012). Offspring of parents with recurrent depression: Which features of parent depression index risk for offspring psychopathology? Journal of Affective Disorders, 136, 44–53. doi:org/10.1016/j.jad.2011.09.002 [ Links ]
McAdams, T., Rijsdijk, F. V., Neiderhiser, J. M., Narusyte, J., Shaw, D. S., Natsuaki, M. N., Eley, T. C. (2015). The relationship between parental depressive symptoms and offspring psychopathology: Evidence from a children-of-twins study and an adoption study. Psychological Medicine, 45, 2583–2594. doi:org/10.1017/S0033291715000501 [ Links ]
McLaughlin, K. A., Gadermann, A. M., Hwang, I., Sampson, N. A., Al-Hamzawi, A., Andrade, L. H., Kessler, R. C. (2012). Parent psychopathology and offspring mental disorders: Results from the WHO World Mental Health Surveys. The British Journal of Psychiatry, 200(4), 290–299. doi: 10.1192/bjp.bp.111.101253. [ Links ]
Santana, G. L., Coelho, B. M., Borges, G., Viana, M. C., Wang, Y. P., & Andrade, L. H. (2015). The influence of parental psychopathology on offspring suicidal behavior across the lifespan. Plos One, 10, e0134970. doi:org/10.1371/journal.pone.0134970 [ Links ]
Silva, S., & Maia, A. (2008). Versão Portuguesa do Family ACE Questionnaire (Questionário de história de adversidade na infância) [Portuguese version of ACE Study Questionnaire]. In A.P. Noronha, C. Machado, L. Almeida, M. Gonçalves, S. Martins, & Ramalho, V. (Eds), Actas da XIII conferência avaliação psicológica: Formas e contextos. Braga: Psiquilibrios Edições
Sugaya, L., Hasin, D., & Olfson, M. (2012). Child physical abuse and adult mental health: A national study. Journal of Trauma Stress, 25, 384–392. doi:org/10.1002/jts.21719.Child [ Links ]
Endereço para Correspondência
Praceta do Vilar 2, 4710-057 Braga. E-mail: a62232@alumni.uminho.pt
Recebido em 05 de Outubro de 2015
Aceite em 10 de Dezembro de 2015














