Migration is a disruptive experience in which individuals face many challenges and constantly rebuild their social networks. Migrants must adjust to unknown and sometimes adverse circumstances in the host country. They also have to adapt to a new culture and cope with several distresses, potentially impacting their mental health (Meng & Xue, 2020). According to Perry and Pescosolido (2012), disruptive events can play an additional role in modifying the structures and functions of social networks. They can compromise the social determinants of health embedded in them, such as social support and social capital, and generating exposure to health problems. However, the patchwork quilt of concepts operating as social determinants of health presents diverse construct operationalization routes, contributing to the contrasting findings about their predictive role on health and well-being (Lee et al., 2016; Thoits, 2011). Although the literature continues to explore the role of these social determinants, few studies have analyzed how migrants' social network structure and functions evolve during their migratory trajectories, particularly when the outbreak of COVID-19 amplified additional challenges.
This paper incorporates 2 studies. In study 1, our primary goal was to analyze how the immigrants from the Community of Portuguese Language Countries (CPLC) living in Portugal perceived their mental health before and during the pandemic. Specifically, we tried to understand how social networks overlap and how mental health and social support perceptions changed during that timeframe. We also researched into whether changes in health networks were explained by structural network features, such as social ties, network efficiency, and social capital. Then, in study 2, we took a similar approach by exploring the same variables before and during the pandemic, but with a sample of Portuguese citizens (non-migrants). Conducting another study with a sample of non-migrants allowed us to verify if a different network pattern happened between CPLC immigrants and non-migrants.
We start by clarifying the literature on social networks and highlight the importance of distinguishing different types of networks (specific-health networks) and their relationship with mental health. Afterwards, we look at social support and social capital as social determinants of health embedded in social networks to conceptually disentangle both constructs and evidence their repercussions on mental health, funneling the literature to the migration context.
Social networks and mental health
The literature states that social networks and interpersonal relationships play a role in psychological well-being, but it remains unclear how these networks are conceptualized and the resources embedded and mobilized (Lee et al., 2016). According to Morina et al. (2021), rapid narrative review of the links between social connection and health, the lack of social connection is associated with poorer mental health (e.g., depression, social anxiety, dementia, late-life suicidal ideation), as well as physical health (e.g., chronic symptomatology, frailty, coronary heart disease, early mortality), in different populations and contexts. Because the COVID-19 pandemic's primary measures included physical distance to contain the virus and decreased social connections, revealing links with poorer mental health (Morina et al., 2021), there remains the relevance of exploring how individuals' social networks changed and their relation to mental health outcomes during that time frame.
One perspective on social networks depicts Burt's structural holes theory and Granovetter's assumptions on strong (e.g., close ties, like family) and weak ties (e.g., coworkers; Burt, 2000). Following these premises, social networks with interpersonal gaps (structural holes) have weaker ties and are embedded with flows of non-redundant information, leading to more efficient networks (Burt, 2000). Network efficiency and information acquisition are essential for decision-making, mainly when the literature states that individuals' behaviors, attitudes, and mental health are shaped by network resources (Lee et al., 2016; Perry & Pescosolido, 2010). Network analysis offers the potential to gain insight into the network structure (e.g., homophily), its size (e.g., degree), and composition (e.g., the type of relationship the ego has with alters) to understand better social connections (Jiang & Carroll, 2009) and psychological processes.
The egocentric network approach has been used to study interpersonal ties and the structural features of social networks, where the (ego) reports about the members (alters) comprising their networks and their interrelationships (Perry et al., 2020). Most studies on this approach focus on general networks that only capture the relationships egos maintain with alters with whom they talk about relevant yet broad matters, leading to the depiction of networks embedded with overall resources (Perry & Pescosolido, 2010). According to Perry and Pescosolido (2010), individuals interact with specific people according to their needs at different moments of their lives and see their attitudes shaped by them, activating close ties and health discussants (e.g., specialists; Wellman, 2000) when health needs are urgent. To better understand the particularities of such a network, a specific-health network approach is crucial (Perry & Pescosolido, 2010).
Stability also characterizes social networks because all networks have a core, long-lasting connectedness within, increasing the likelihood of overlapping alters between different types of networks (e.g., general vs health-specific). However, disruptive events can increase the chance of tie-breaking, provoking changes in the network structures and functions, blocking access to new information and decreasing the number and quality of the embedded network resources (Perry & Pescosolido, 2012). The combination of multiple disruptive events can play an even more significant role among those who already have unstable social networks: immigrants are continuously rebuilding their social networks in the host country (Arpino & de Valk, 2018), where they face several stressful events related to their migratory status. When combined with the social impositions from the COVID-19 outbreak, these may make their networks less prone to stability and overlap, undermining their well-being and mental health. Social networks comprise relationships between alters and egos and interrelationships between alters, allowing egos to access and mobilize social determinants of health, such as social support and social capital. The following section will call attention to the link between social support and social capital, while trying to differentiate them and their association with mental health.
Social support, social capital and mental health
Social support is a multidimensional construct referring to the functions and characteristics of social relationships (Lourel et al., 2013). The operational aspect of social support is related to its functions (e.g., emotional, instrumental, informational and esteem transactions), while its structural facet encompasses social integration and social networks based on the network size as a proxy of the perceived support individuals have in their environment (Brissette et al., 2000). Recently, social support negative interactions have also been emerging, stating its role as a source of psychological stress (Thoits, 2011) able to promote adverse health outcomes (Platt et al., 2014).
Among social capital scholars, this concept has also started to be operationalized as direct transduction into social networks. Putnam (2000) began to describe social capital as bonding (individuals linked with strong, similar ties) and bridging social capital (individuals linked with weak, dissimilar ties). Moreover, the idea of strong and weak ties also plays a role in the structural holes approach proposed by Burt (2000), in which social capital emerges from social networks whenever gaps occur between alters’ interrelationships providing non-overlapping information and benefits to the ego. It can be argued that social networks that are less interconnected will generate more social capital because those networks have less cohesive ties, more structural holes and more non-redundant, efficient information. Further, following Lin and colleagues (2001) perspective, social capital refers to the resources that egos have in their social networks, which can be accessed or mobilized in purposive actions through different relationships established in their networks, allowing egos to overcome barriers and acquire advantages. As social capital is embedded in social networks, using a position generator to collect ego connections to detect ties that are in social advantage is essential to inform interventions aiming to reduce health disparities (Meanley et al., 2020).
Social connections are crucial for individuals' health, but the literature points to several underlying definitions making it challenging to understand which social connection elements are significant for individuals. For instance, social support and social capital are variables applied to measure social relationships. However, most of the time, many use them as the same construct, overlapping each other (Richardson et al., 2022). According to Richardson et al. (2022), social capital is a broader concept comprising a more extensive set of social connection characteristics, such as perception of connectedness and social support. Because this misconception makes it challenging to assess the impact of each indicator as a social determinant of health, the two constructs should be assessed separately. Despite being important determinants rooted in social networks that help individuals face adversities, social support is a component of social capital (Liu & Yeo, 2021).
For instance, when addressing the role strong and weak ties play when social support is provided, Kindler and Wójcikowska-Baniak (2019) showed that the former gives more emotional support, while the latter is responsible for instrumental support. However, Small (2017) illustrated that confiding with strong ties can generate losses in emotional support and well-being due to the probability of hurtful interactions, suggesting that weak-tie confidants are easier to approach and generate empathy. Indeed, the debate around strong and weak ties is not novel. In 2001, Kawachi and Berkman (2001) determined that weak ties can contribute to a sense of belonging and social identity, which is associated with better psychological well-being, while Mair and Thivierge-Rikard (2010) stated that strong ties were associated with the latter.
Another facet contributing to the strong and weak ties controversy is the similarity between the ego and its network alters. While relationships with others who are similar (homophily) may contribute to a greater sense of connectedness, boosting the perception of the network support due to the sense of belonging; the relationships with alters who are different (heterophily) allow accessing novel, diverse, and important information (Lee et al., 2016). As Majeed and Ajaz (2018) reinforced by anchoring on norms, social ties (particularly strong, homophilic ties) are not always beneficial to individuals, contributing to positive associations with unhealthy behaviors (e.g., smoking). Nevertheless, the impact of networks' homophily/heterophily ties on quality of life is still unclear (Lee et al., 2016).
Individuals' benefits from their networks go beyond the ties established with the network alters. To Platt et al. (2014), the number of alters individuals have in their networks is a proxy of their perceived social support, predicting their mental health and assuming a more prominent role than the perceptions of strong social support. However, network sizes change over time according to egos' needs and contexts, leading to differences in social support mobilization (Sweet et al., 2018). For instance, well-being can even be found when people have sparse networks with few social contacts (e.g., diverse and active networks with large numbers of alters can be stressful to maintain). In contrast, networks with a high level of offered support (e.g., family and stable) may elicit conflicts more easily (Sweet et al., 2018). As such, the overall role of the social network size still needs to be clarified. The mixed results highlighted in this section may not only be due to the multidimensionality of social support and social capital. This can also lead to contradictions, because few studies have consistently explored the role of these variables on mental health in social networks, keeping separate operationalizations for each construct. In the current study, we intend to capitalize on that differentiation.
Migrations: Social networks, social support, social capital and mental health
As highlighted in previous sections, social support and social capital are determinants of health embedded in social networks, which are crucial elements in migrations. The literature on social support has shown social support to be a buffer against mood and anxiety disorders. For instance, Puyat (2013) revealed the protective effect of high levels of social support among long-term immigrants in Canada (> 10 years) and the adverse effects of low social support on recent immigrants (< 10 years), in mood and anxiety disorders. The literature has also suggested that migrants' strong ties may lead to social withdrawal through the association with the ingroup, restricting their networks and compromising their health (Lecerof et al., 2016). Despite this suggesting the benefits of having networks with more structural holes, the opposite effect has also been documented (e.g., Johnson et al., 2017).
Migration in Portugal: Health challenges and the burden of COVID-19
As a member state of the CPLC, Portugal plays a part in the migratory trajectories of this community’s citizens (e.g., immigrants from Brazil and Portuguese-speaking African Countries - PALOP), due to cultural proximity and shared language: a fundamental feature in migrations (Sin et al., 2021). Most immigrants living in Portugal are from the CPLC community, with Brazilian immigrants currently being the most representative group (Posch & Cabecinhas, 2020). According to the study by Godinho et al. (2008) on African and Brazilian immigrant's mental health, Brazilians are more prone to mental health problems, especially Brazilian women, which can be explained by the literature revealing higher levels of prejudice and discrimination towards them in Portugal, contributing to undermining their well-being (França & Oliveira, 2021). With the outbreak of COVID-19, Posch and Cabecinhas’ (2020) qualitative research on the mental health of Brazilian immigrants showed that the pandemic amplified the number of challenges these immigrants had to face (e.g., unemployment) and intensified their feelings of loneliness. As Brazil became an epicenter of the pandemic, xenophobia and social exclusion increased towards Brazilian immigrants in Portugal, changing their social networks by increasing their contacts with people from their origin country to cope with this disruptive event (Posch & Cabecinhas, 2020). In addition, a study conducted in Lisbon during the pandemic with immigrants coming from CPLC (70.6%), Middle Eastern and Asian countries (29.5%) revealed the worsening of their financial situation, particularly among undocumented immigrants (9.3%), with 20% also reporting a decrease in their health condition. This was higher among women, immigrants older than 45 years, with lower levels of education and lower incomes (Gama et al., 2022). The confinement and physical distance due to COVID-19 increased the mental health problems of both Portuguese (36%) and Brazilian (52%) citizens, despite few studies focusing on the topic during this critical period (Gil et al., 2022). Furthermore, understanding the impact of mental health care on the Portuguese population is still limited, and data are scarce, especially those exploring the social determinants of health, such as their social networks and social capital. To our knowledge, this is the first study in Portugal to map immigrants' perceptions of their complex social health context (social networks), working as social determinants of health (e.g., social capital, social support) and how those determinants interact.
Summing up, previous literature has emphasized that the implications of social support and social capital as social determinants of health are contradictory. The literature also states these determinants are embedded in social networks, which requires a social network’s approach as a source of information to operationalize these social determinants and their role in explaining mental health, through a specific-health network approach. Several studies suggest contradictory findings because the social determinants of health are multidimensional and because migrants' social networks suffer natural fluctuations during their trajectories in the host country (Kindler & Wójcikowska-Baniak, 2019). Those fluctuations per se will require an analysis of the impacts of network change, since significant resources related to their health are embedded in their networks. Furthermore, disruptive events, like COVID-19, can also prompt such network changes, resulting in additional modifications in the network's structure and functions, in further transformations of those social determinants, and in increases of the potential losses migrants suffer in their health and well-being.
Aims and hypotheses
This research incorporates two studies. Study 1 measured the perceived mental health of CPLC immigrants before and during COVID-19 and associated those outcomes with network changes that might have occurred during the same time frame. We did this by evaluating network overlap and exploring network size as a source of perceived available social support. We also approached social network changes by focusing on the differences in social ties’ patterns, network efficiency and social capital. Then, in study 2, we took the same approach by exploring the same variables before and during COVID-19 on a sample of Portuguese citizens (non-migrants). Immigrants are a population sub-group facing challenges that non-migrants do not have to. Thus, disrupting their social networks is expected to add challenges to their lives that may compromise their mental health. By conducting study 2 with a sample of Portuguese citizens (non-migrants), we checked whether the network pattern identified for CPLC immigrants was similar for non-migrants or if specificities could be identified for each group, allowing us to understand better the social determinants of health and their role in mental health perceptions.
In study 1, we expected CPLC migrants to have unstable networks (a decrease in overlap), reduced their perceived social support (smaller health-specific networks), and decreased their perceived mental health levels during the COVID-19 pandemic. Since we focused on a health-specific network approach, which is more prone to collecting strong ties, we hypothesized that CPLC immigrants would have more family alters. We also anticipated that before the pandemic, CPLC immigrant's health-specific networks should be status heterophilic (more non-migrants ties), switching to status homophilic (more migrants and/or transnational ties) during the pandemic. These changes in network composition would lead to a decrease in social capital (mostly with bridging social capital being lost), with consequently less efficient networks during the pandemic.
In study 2, we expected Portuguese non-migrants to reduce their perceived social support levels (reduce the number of ties) and their perceived mental health levels during the COVID-19 pandemic. Due to health networks gathering mainly strong family ties, we expected non-migrant ties to be constituted mainly by family alters. Since non-migrants have more stable networks than immigrants, we expected that their health networks would remain status homophilic (containing mainly non-migrant ties) during COVID-19, preserving their social capital levels and the efficiency of their social networks.
Method
Data collection and procedures
Study 1 and study 2 were conducted online through the Qualtrics Surveys platform (version 1.2020), using a convenience sampling strategy, with the study link shared online through social media. First, the participants (egos) had access to informed consent, through which they learned about the study's aims and procedures, being informed that the confidentiality and anonymity of their responses were guaranteed. In both studies, we collected from each participant two egocentric health networks: one referring to the network that egos perceived before the pandemic and the other addressing the network that egos perceived they had during the pandemic. Participants answered the socio-demographic questionnaire and then the egocentric network survey, eliciting the alter names and attributes. We randomized the order of networks to avoid order effects. Data collection for study 1 and study 2 occurred between July and November 2020. Specifically, in study 1, the first ego responded on July 30th and the last on November 6th. In study 2, the first ego responded on July 25th and the last on November 11th. Questionnaires took an average of 20 minutes to finish. The Ethics Committee of the Faculty of Psychology of Lisbon University approved study 1 and study 2. We followed the ethical code of the American Psychological Association (APA).
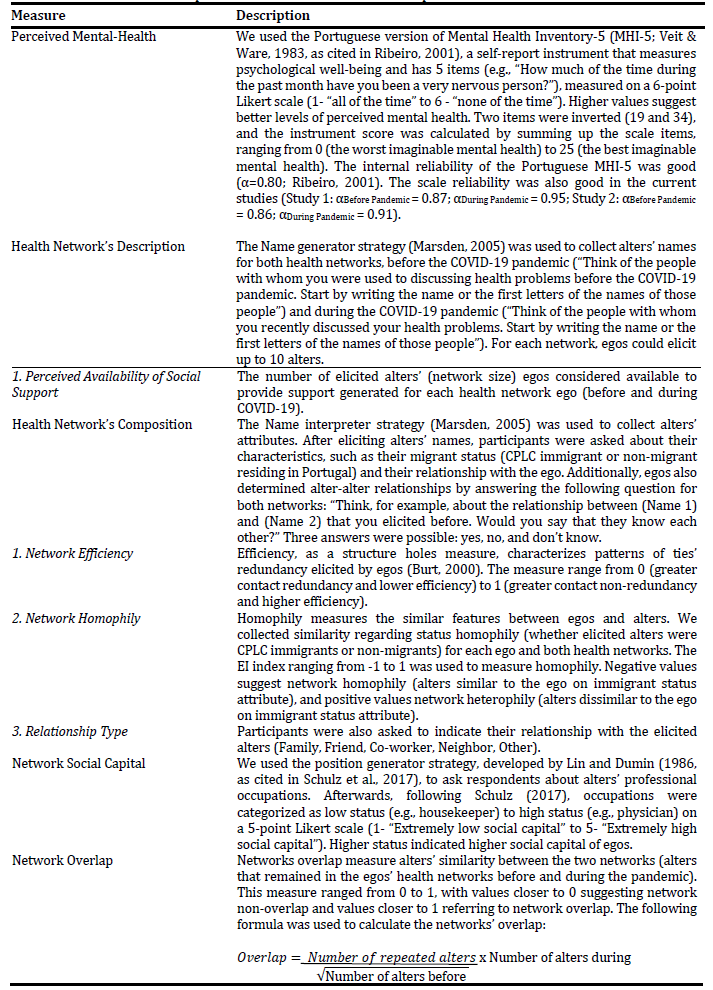
Measures
We used a self-report socio-demographic questionnaire to gather information from participants (egos). In study 1, we collected data on egos’ gender (Female, Male, Other), age (in years), educational attainment (primary, secondary and college degree), immigrants’ country of origin (Brazil, PALOPs-Africa’s Portuguese-speaking countries), immigrants’ length of time in Portugal (< 2 years, ≥ 2 years). In study 2, we collected data on egos’ gender (Female, Male, Other), age (in years), and educational attainment (primary, secondary and college degree). Both studies used the Mental Health Inventory-5 (MHI-5) and the Egocentric Network Questionnaire (Health Networks: size, composition, social capital and overlap; please see Table 1).
Data analysis
We started by extracting network efficiency scores and homophily EI indexes using the E-NET software (Borgatti, 2006). Following this, we computed descriptive statistics (mean (M), standard deviation (SD), median (Me), and interquartile range (IQR)) to characterize the study variables. Associations between variables were estimated using Kendall’s taub(T B ) correlation coefficient (T B < 0.30 small correlation; T B > 0.5 large correlation), which is a non-parametric procedure used whenever sample sizes are small, complemented with bootstrapping for standard errors (1000 samples) and 95% bias-corrected confidence intervals (CI). The exploratory data analysis (descriptive and correlation statistics using data visualization (boxplots and scatterplots) was performed using SPSS (v. 27, SPSS Inc., Chicago, IL) and R environment (graphical representations).
Study 1
Method
Participant and network characteristics. The sample comprised 18 participants (egos). The following inclusion criteria were defined: i) being a CPLC immigrant living in Portugal, ii) being more than 18 years of age. On average, CPLC immigrants, during the pandemic, rated their mental health as worse, particularly those living in the country for less time (less than 2 years). Besides that, they had more ego females and high educational attainment. Also, CPLC immigrants' health networks were composed mainly of family alters before and during the COVID-19 pandemic. The CPLC immigrants were skewed regarding Brazilian immigrants (please see Table 2).
Table 2 Sociodemographic Characteristic of CPLC egos and health networks before and during the pandemic (N = 18).
| n (%) | M (SD) | Me (IQR) | |
| CPLC Egos | |||
| Age | - | 32.89(13.96) | 26.50(22.2) |
| Gender | |||
| Female | 16(88.9) | - | - |
| Male | 2(11.1) | ||
| School Attainment | - | - | 3(1) |
| CPLC Country of Origin | |||
| Brazil | 16(88.9) | - | - |
| PALOP | 2(11.1) | - | - |
| Living in Portugal (< 2 years) | 6(33.3) | - | - |
| Living in Portugal (≥ 2 years) | 12(66.7) | - | - |
| Perceptions Regarding the Time Before COVID-19 (perception of past) | |||
| Perceived Mental Health | - | 18.33(5.63) | 19.5(9.25) |
| Living in Portugal (< 2 years) | - | 16.33(5.72) | 18.50(10.25) |
| Living in Portugal (≥ 2 years) | - | 19.33(5.55) | 20(10) |
| Perceived Availability of Social Support | - | 3(1.50) | 3(2.5) |
| Network Composition | |||
| Family | 32(59.2) | - | - |
| Friend | 16(29.6) | - | - |
| Co-Worker | 2(3.7) | - | - |
| Neighbor | - | - | - |
| Other (e.g., healthcare) | 4(7.4) | - | - |
| Migrant status | |||
| Immigrant | 17(31.5) | - | - |
| Non-migrant | 37(68.5) | - | - |
| Social Capital | - | 2.99(1.03) | 3.00(2.00) |
| Perceptions Regarding Time During COVID-19 (perception of present) | |||
| Perceived Mental Health | - | 16.72(5.96) | 16(9.5) |
| Living in Portugal (< 2 years) | - | 15.00(6.73) | 13.50(10.75) |
| Living in Portugal (≥ 2 years) | - | 17.58(5.60) | 17.00(11.50) |
| Perceived Availability of Social Support | - | 3(1.68) | 3(4) |
| Network Composition | |||
| Family | 37(68.6) | - | - |
| Friend | 13(24.1) | - | - |
| Co-Worker | 2(3.7) | - | - |
| Neighbor | - | - | - |
| Other (e.g., healthcare) | 2(3.7) | - | - |
| Migrant status | |||
| Immigrant | 26(49.1) | - | - |
| Non-migrant | 27(50.9) | - | - |
| Social Capital | - | 2.57(1.03) | 2.73(1.15) |
| Health Network´s Overlap | - | 0.71(.30) | 0.78(.50) |
Note. School attainment is an ordinal variable with a median of 3 illustrating college degree.
Results
CPLC immigrants’ health networks: Perceived mental health, networks overlap and perceived availability of social support (network size). On average, immigrants’ levels of perceived mental health before and during the pandemic decreased during the pandemic (M Before = 18.33, SD Before = 5.63, 95% CI [15.5, 21.1]; M During = 16.72, SD During = 5.96, 95% CI [13.8, 19.7]; Figure 1), revealing a network prone to changing alters (M = 0.71, SD = 0.30, 95% CI = 0.57, 0.85). The network's overlap role on perceived mental health during the pandemic for CPLC immigrants showed a small tendency for an increasing slope (T B = 0.02, 95% CI [-0.31, 0.35]; Figure 2A), which was steeper for perceived availability of social support on perceived mental health, revealing a moderate association (T B = 0.38, 95% CI [0.06, 0.63]); Figure 2B).
Explaining changes in networks’ composition of CPLC immigrants: Health network’s efficiency, homophily and social capital. Analyzing the efficiency of the networks before and during the pandemic shows that CPLC immigrants started losing network efficiency during this period (M Before = 0.56, SD Before = 0.27, 95% CI [0.36, 0.62]; M During = 0.49, SD During = 0.23, 95% CI [0.36, 0.55]; Figure 3A). Additional network analysis revealed that, before the pandemic, the composition of the networks reported by CPLC immigrants had a majority of non-migrants as alters (Figure 3C), but during the pandemic, CPLC immigrants reported networks started having a majority of migrants, increasing their homophily (M Before = 0.26, SD Before = 0.81, 95% CI [0.04, 0.85]; M During = -0.03, SD During = 0.83, 95% CI [-0.36, 0.44]), changing from heterophilic networks to homophilic networks during the pandemic (Figure 3B). Further, a positive and strong association between network efficiency during the pandemic and status homophily was found (T B = 0.50, 95% CI [0.09, 0.76]), with network efficiency being positively associated with heterophilic ties (Figure 3C). This association, and the importance of weak ties (heterophilic ties), were also sustained by the relationship between social capital and status heterophily with a positive and moderate association between the two variables (T B = 0.37, 95% CI [0.04, 0.63]; Figure 3D).

Figure 2 CPLC immigrants’ health network’s overlap and perceived size slopes on perceived mental health during COVID-19.
Study 2
Method
Participants. The sample comprised 53 participants (egos). The following inclusion criteria were defined as follows: i) being a Portuguese native living in Portugal, ii) being more than 18 years of age. On average, Portuguese citizens (non-migrants) perceived lower levels of mental health. Besides that, the sample had more ego females and high educational attainment. Participants' health networks were also composed mainly of family alters before and during the COVID-19 pandemic. Regarding social capital, for participants’ perceived higher levels of social capital during the pandemic, please see Table 3.
Table 3 Sociodemographic characteristics of Portuguese egos and health networks before and during the pandemic (N = 53).
| n (%) | M (SD) | Me (IQR) | ||
| Egos | ||||
| Age | - | 24.79(7.62) | 22(9.50) | |
| Gender | ||||
| Female | 40(75.5) | - | - | |
| Male | 13(24.5) | - | - | |
| School Attainment | - | - | 3(1) | |
| Perceptions Regarding the Time Before COVID-19 (perception of past) | ||||
| Perceived Mental Health | - | 19.83(4.22) | 20(5.5) | |
| Perceived Availability of Social Support | - | 3.28(1.31) | 3.99(2) | |
| Network Composition | ||||
| Family | 105(60.4) | - | - | |
| Friend | 56(32.2) | - | - | |
| Co-Worker | 1(0.6) | - | - | |
| Neighbor | 3(1.7) | - | - | |
| Other (e.g., healthcare) | 9(5.2) | - | - | |
| Migrant status | ||||
| Immigrant | 4(2.3) | - | - | |
| Non-migrant | 167(97.7) | - | - | |
| Social Capital | - | 3.06(.85) | 3.00(1.21) | |
| Perceptions Regarding Time During COVID-19 (perception of present) | ||||
| Perceived Mental Health | - | 19.30(4.67) | 20(7.5) | |
| Perceived Availability of Social Support | - | 3.26(1.46) | 3(3) | |
| Network Composition (n, %) | ||||
| Family | 99(57.2) | - | - | |
| Friend | 59(34.1) | - | - | |
| Co-Worker | 3(1.7) | - | - | |
| Neighbor | 1(0.6) | - | - | |
| Other (e.g., healthcare) | 11(6.4) | - | - | |
| Migrant status (n, %) | ||||
| Immigrant | 2(1.2) | - | - | |
| Non-migrant | 168(98.8) | - | - | |
| Social Capital | - | 3.10(.92) | 3.00(1.31) | |
| Health Network’s Overlap | - | 0.86(.25) | 1(.20) | |
Note. School attainment is an ordinal variable with a median of 3 illustrating college degree.
Results
Non-migrants’ perceived mental health: Exploring ego-health network’s overlap and perceived availability of social support (network size). On average, non-migrants slightly decreased their mental health during the pandemic (M Before = 19.8, SD Before = 4.22, 95% CI [18.7, 21.0]; M During = 19.3, SD During = 4.67, 95% CI [18.0, 20.6]; Figure 4). The ego-health network’s overlap slightly decreased but remained close to 1 (M = 0.86, SD = 0.24, 95% CI [0.79, 0.92]), suggesting our sample of non-migrants activated networks with similar alters they had before the pandemic, and even during a disruptive event, they were able to maintain their social networks, showing they were stable. Yet, the role of the network overlap on perceived mental health during the pandemic showed a horizontal slope (T B = 0.01, 95% CI [-0.17, 0.20]; Figure 5A). Moreover, the association between the perceived availability of social support (network size) and perceived mental health during the COVID-19 was negative and small for non-migrants (T B = -0.10, 95% CI [-0.28, 0.08]), with a decreasing slope (Figure 5B).
Explaining changes in network composition of non-migrants: Health network’s efficiency, homophily and social capital. When analyzing the efficiency of the networks before and during the pandemic, data suggest that non-migrants slightly increased the efficiency of their health networks during the pandemic (M Before = 0.50, SD Before = 0.21, 95% CI [0.44, 0.56]; M During = 0.54, SD During = 0.24, 95% CI [0.47, 0.61]; Figure 6A). Regarding networks’ homophily, non-migrant networks were homophilic before the pandemic, with the majority having non-migrant alters. Furthermore, during the pandemic, their homophilic status was reinforced (shown in Figure 6B; M Homophily Before = -0.92, SD Homophily Before = 0.32, 95% CI [-0.98, -0.79]; M Homophily During = -0.95, SD Homophily During = 0.17, 95% CI [-0.99, -0.89]). Additionally, the association between network efficiency during the pandemic and status homophily was positive and small for non-migrants (T B = 0.20, 95% CI [-0.00, 0.38]; Figure 6C). Non-migrants' network efficiency was not associated with heterophilic ties, as these remained homophilic (with more non-migrants) during the pandemic. The significance of weak ties and the relationship between social capital and status heterophily was positive and small for non-migrants (T B = 0.17, 95% CI [-0.01, 0.34]; Figure 6D).

Figure 5 Non-migrants’ health network’s overlap and perceived size slopes on perceived mental health during COVID-19.
Discussion
Research on social networks, social support and social capital has demonstrated these constructs' importance in explaining health. During the migratory process, social networks suffer modifications in their structure, which can be enhanced by disruptive events, such as COVID-19, accentuating the challenges migrants have to face. Our research included two studies. Study 1 aimed to analyze how CPLC immigrants perceived their mental health before and during the pandemic and to what extent COVID-19 has changed those perceptions, their networks and the perceived availability of social support, by implementing an ego network analysis. We also aimed to analyze the changes in their social networks during the pandemic regarding network overlap, composition, efficiency, homophily and social capital testing; and which associations occurred between these variables. In study 2, we explored the same variables before and during the pandemic but with a sample of Portuguese citizens (non-migrants). With these two studies, we could explore if CPLC immigrants had a different pattern than a sample of Portuguese citizens regarding their social determinants of health.
We started by looking at the levels of perceived mental health before and during the COVID-19 pandemic. When we look at the descriptive results of studies 1 and 2, the levels of perceived mental health before the pandemic were similar between CPLC immigrants and non-migrants. However, when confronted with the disruptive event during COVID-19, the perceived mental health of both groups decreased but was more pronounced for CPLC immigrants. The pandemic may have accentuated modifications to the network's structure (Perry & Pescosolido, 2012) because migrant networks are constantly rebuilt at the destination (Arpino & de Valk, 2018), decreasing access to embedded resources and compromising migrants' health.
Indeed, perceived social support, accessed through the network size, was more significant for CPLC immigrants, who saw the size of their network decreasing during the pandemic. A positive association between the network size and perceived mental health was found for CPLC immigrants during the outbreak. The perception of greater availability of network resources amplifies the possibility of interacting with significant alters who are essential for the egos’ resilience, information acquisition and decision-making on health (Lee et al., 2016; Perry & Pescosolido, 2010). This element may be even more salient when facing challenges, just like the pandemic, when access to social ties was constrained. Thus, changes in immigrants' network composition may have inhibited the functional aspects of their perceived social support, constraining their mental health. Before the pandemic, the CPLC immigrant networks were status heterophilic, comprised more non-migrants, and had weak ties that allowed them to expand their resources associated with network efficiency. During the pandemic, their networks changed and became more homophilic, losing non-migrant ties and integrating stronger ties. With more unstable networks, CPLC immigrants lost ties during the pandemic that were able to provide functional elements and different types of social support and social capital, changing the flux of embedded resources in their networks. The pattern of CPLC network changes during COVID-19 moved from heterophily to homophily with increased bonding that decreased egos' bridging social capital and increased network redundancy. Such changes in egos' networks may have contributed to increasing their dependence on non-easily available virtual social support (transnational ties) and constraining their mental health. Just like Posch and Cabecinhas (2020) found, when studying the impact of the pandemic on Brazilian immigrants, during the outbreak, these immigrants increased their contact with family members that remained in Brazil. By limiting their relationships to transnational ties, these immigrants restricted the resources that could be mobilized from their networks and the perceived assistance they could have benefited from, concomitantly increasing their insecurity levels (Posch & Cabecinhas, 2020).
Non-migrants perceived mental health also decreased during the pandemic, but their mean levels remained better than those presented by CPLC immigrants. The outbreak changed social interactions, and the perceived mental health of non-migrants may have decreased due to social isolation and increased depression (Passos et al., 2020). However, non-migrants did not face additional network disruptive challenges like immigrants, counting on stable networks from which they could mobilize the resources needed to solve the health requirements that the outbreak presented. Non-migrant networks remained homophilic, with more non-migrant alters. Contrary to CPLC immigrants, non-migrant networks increased their efficiency during the pandemic, despite having redundant information, suggesting their networks were well structured for specific needs despite being populated by strong ties. We might speculate that information redundancy might be beneficial in some contexts, such as health crises for non-migrants when communication and access to healthcare facilities and services are challenging. However, it can undermine immigrants' network efficiency when their networks become filled with redundancy, arising from increasingly strong ties and decreasingly weak ones. For CPLC immigrants, bridging social capital seems crucial for overcoming barriers. Finally, it was also seen that there was a slight decrease in non-migrants’ levels of perceived mental health generated by more extensive networks. Apart from generating redundancy, extensive networks are demanding and crowded with strong ties. Extending the network can, therefore, contribute to maladaptive responses (Sweet et al., 2018). This result may suggest perceived social support as a source of psychological distress in light of extensive networks. Having an efficient network that serves ego necessities, allowing it to mobilize social capital, can also play a pernicious role in ego health.
Limitations and future studies
This study has some limitations that should be addressed in future research. The sample size in both studies was small and non-probabilistic. In study 1, since immigrants are a subgroup of the population, it was harder to collect data from CPLC immigrants when compared to non-migrants, generating an unbalanced sample size between studies. In addition, the sample size may have been compromised by the burden generated by personal network surveys, which are more time-consuming and cognitively demanding when compared to conventional surveys (McCarty et al., 2019). In that sense, results should be interpreted cautiously and within the scope of the study sample. Despite being used to assess health-specific networks, the egocentric network's approach is based on individuals' perceptions, and egos may have mentioned alters according to their relationships and interests (Jiang & Carroll, 2009). Our sample in study 1 also included mainly young female immigrants and was skewed towards Brazilian immigrants. Thus, the results should not be generalized to all CPLC immigrants living in Portugal. Additionally, study 2 included mainly young Portuguese females (non-migrants). Moreover, the study 1 and study 2 data collection happened between July and November 2020, encompassing different stages of the COVID-19 pandemic, and different results may have been obtained at each stage of the pandemic.
Furthermore, social networks are dynamic and unpredictable events dominate the migratory experience; thus, a longitudinal approach could enhance knowledge on this subject. Moreover, future research should address the composition of networks and the types of social capital that can be accessed, continuing to enhance the role of strong and weak ties on health, in the migration context. Studies combining social capital and the functional aspects of social support are also necessary to depict which alters in egos networks provide emotional, instrumental, and informational support. Even though Kindler and Wójcikowska-Baniak (2019) presented the association between emotional and instrumental support with weak and strong ties, studies on the relationship between informational social support and the structural holes’ theory are still needed. Finally, future social network studies should address cultural differences when exploring the social determinants of immigrant health.
Conclusions and implications for practice
The present study aims to clarify how disruptive events combined (migration trajectory and COVID-19) to change individuals' perceived social networks before and during the outbreak. Using an ego-network approach, we analyzed CPLC immigrants' and non-migrants’ health-specific social networks to measure how their perceived social determinants of health, social support and social capital changed and related to perceived mental health.
The pandemic amplified the challenges immigrants faced during their migratory trajectory, generating even more instability in their networks and impairing their perceived social support. By reducing the bridging social capital embedded in CPLC immigrant networks, these changes decreased the network's efficiency and undermined immigrants' mental health perceptions. During the outbreak of COVID-19, several measures were implemented to decrease the deleterious effect of the pandemic on migrants. In Portugal, migrants with irregular status were temporarily allowed full access to the health care system. Nevertheless, more than having admission to the health care system may be needed to effectively access this system because measures per se were not accompanied by the mobilization of the social determinants of health embedded in networks. As this preliminary study evidences, even minor network changes can contribute to significant differences in how CPLC immigrants perceive their mental health. Interventions regarding the management of disruptive crises, promoting informal support systems to assess immigrants' needs, and making resources available, should be designed at the community level (e.g., community groups meeting periodically), bridging the community with health services. By doing so, immigrant networks will expand with new ties and be able to activate social capital according to their needs.
Credit authorship contribution statement
Paulo Nascimento: Conceptualization; Data Curation; Formal analysis; Funding acquisition; Investigation; Methodology; Resources; Software; Validation; Visualization; Writing - Original Draft; Writing - Review & Editing. Magda Sofia Roberto: Conceptualization; Data Curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing - Original Draft; Writing - Review & Editing. Ana Sofia Santos: Conceptualization; Data Curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing - Original Draft; Writing - Review & Editing.