Introduction
Hospital-at-home (HaH) is defined as a resource with nursing, medical, and home rehabilitation services to avoid hospital admission and facilitate early discharge, which offers acute and short-term complex interventions at home, aiming to replace total or partial hospitalization (U, E. C. Y. et al., 2017). It is an alternative to hospitalized patients with chronic illnesses, which contributes to increasing caregiver satisfaction, improving patient’s quality of life, and reducing costs without adding adverse effects to clinical results (Voudris & Silver, 2018). Common among several authors is the idea that HaH should be understood as a temporary service (Shepperd & Iliffe, 2005).
HaH, which emerged in the United States of America in the 20th century, involves the creation of multidisciplinary teams that carry out, for example, daily home visits to assess the patient’s clinical condition. This type of care is not exempted from a set of requirements to which the patient must comply and requires the patient's informed consent.
Hospital organizations (hospital and local health units) provide outpatient and inpatient healthcare. Hospitalization (designed as classic hospitalization (CH) in this research) involves the occupation of a crib/bed by a patient who needs health care to identify diagnosis and treatment or palliative care for a minimum period of 24 hours (Martins & Nogueira, 2017).
Cost-effectiveness analysis is an economic evaluation in which the consequences of different options for a target are translated into natural units. The relevance of data on the effectiveness of the services provided is crucial for an evaluation that allows determining which service has the lowest cost. For the cost-effectiveness analysis to be successful, it is necessary to verify the proximity relationship between the object of study and the data already available to verify the data from random and controlled studies and, finally, verify that the data are representative and a high degree of completeness (Lourenço & Silva, 2008).
The sustainability of the health system is a current issue, given the scarcity of resources. It is possible to reduce costs and improve care and the sustainability of the National Health Service (NHS) if health programs are implemented cost-effectively (Barros, 2014). Analyzing the implementation of HaH models in countries that have already done this evaluation, it seems this health program can contribute to the efficiency of the Portuguese NHS.
Home nursing care should be planned, organized, directed, and controlled, ensuring safe and quality practices. The nurse manager is responsible for operating the conditions for exercising best practices, in this case, at home. Transitioning from inpatient to HaH means forming a multidisciplinary team and consequently assessing the satisfaction of caregivers mobilized from hospital to home care, and this assessment becomes the responsibility of the care manager. The nurse managers addressing the subject of this study and their skills are understood to be an integral part of this change process in the national health service.
To contribute to the discussion on the economic impact of home hospitalization and the sustainability of the National Health Service, the present study aims to identify and synthesize the best available evidence on the cost and effectiveness of Hospital-at-home versus Classic hospitalization from all perspectives, identify which implementation model has the best cost-effectiveness.
1. Methods
This study is a systematic literature review with a qualitative and quantitative approach, a type of secondary study. The preference for this methodology focuses on the fact that this type of study allows a comprehensive synthesis of all existing scientific knowledge to date on an object under analysis, thus supporting an evidence-based conclusion to meet the objectives of the study (Bettany-Saltikov, 2012; Jordan et al., 2019). A research protocol was developed and registered at PROSPERO (CRD42021230000). This SRL was supported by the Joanna Briggs Institute® (JBI) conceptual model. The levels of evidence for effectiveness and the evidence for economic analysis defined by the JBI were used as a guideline.
1.1 Review question
The PICO question (table 1) formulated for this study was: “Which model of hospitalization, classic vs. hospital-at-home, has the better cost-effectiveness?”
1.2 Inclusion and exclusion criteria
The inclusion criteria were studies on patients hospitalized at the home of pediatric and adult and elderly age, studies that assess the cost and the effectiveness of the hospital-at-home, studies that compare the cost and the effectiveness of the model of hospital-at-home and classic hospitalization, and there were no context constraints in this review. The language was also an inclusion criterion. Therefore, we chose articles written in Portuguese, English, or Spanish and dated between 2010 and 2023. The outcomes of the studies included in this systematic literature review had the analysis of the cost-effectiveness of hospital-at-home and classic hospitalization. The types of studies included in this systematic literature review were randomized controlled trials, experimental studies, cohort studies, case-control studies, quasi-experimental studies, and descriptive studies.
The exclusion criteria were unnecessary since they contradict the inclusion criteria (Tufanaru et al., 2020). However, in the case of an SRL, the inclusion criteria should not be isolated (Tufanaru et al., 2020); therefore, in this study, exclusion criteria were the types of studies (secondary studies, opinion articles, letters from readers and comments), the language (all languages other than those included), the time of publication (studies not published between 2010 and 2023), studies that did not compare, analyzed, or did not research the cost-effectiveness of HaH and CH.
1.3 Search strategy
The selection process had two phases (Centre for Reviews and Dissemination, 2009; Bettany-Saltikov, 2012). The first corresponds to filtering the abstracts and titles of the studies identified in the search and selecting those that match the inclusion and exclusion criteria, excluding those that do not meet the predefined criteria. The second phase involved reading, in total, the studies selected (Centre for Reviews and Dissemination, 2009; Bettany-Saltikov, 2012). It was also necessary to verify the existence of duplicate studies (Centre for Reviews and Dissemination, 2009; Lefebvre et al., 2019). In this study, EndNote software was used as a resource to store, organize, and display the recordings made for each selected article.
During the development of the search strategy, it is necessary to identify the keywords (hospital-at-home, classic hospitalization, cost-effectiveness) and their translations to expand the search.
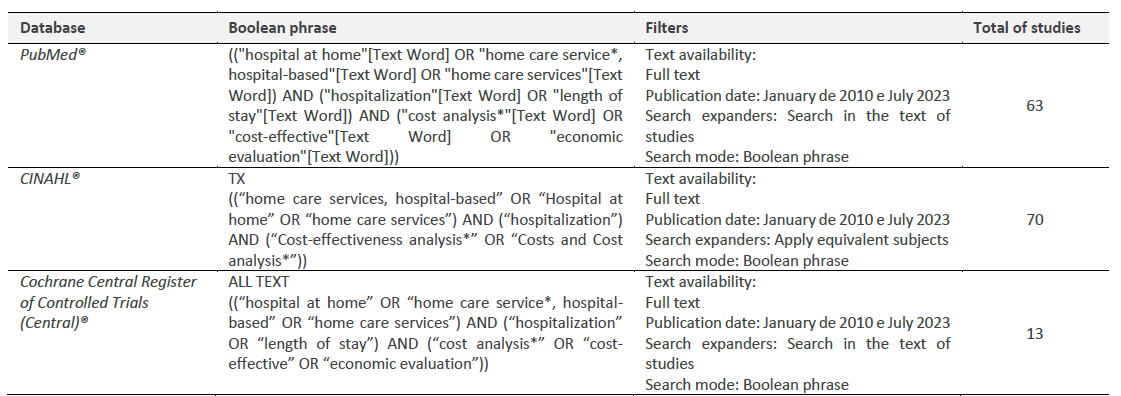
This research selected the databases and search engines recommended in the 2020 JBI Manual. Therefore, we resorted to CINAHL® (EBSCO HOST® via ESEP), Cochrane Central Register of Controlled Trials (Central)® (EBSCO HOST® via ESEP), and PubMed®, which integrates the MEDLINE® database, the NHS Economic Evaluation Database, and the Cost-effectiveness analysis registry (included in the JBI suggestions). A Boolean phrase was built for each database with the specific indexed terms for each and its respective limiters (table 2).
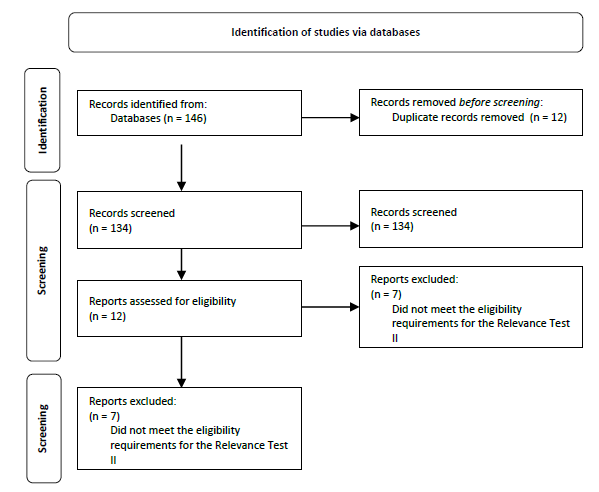
At an early stage, 146 studies were identified. After removing 12 duplicate studies, we totaled 134 studies for screening.
1.4 Study selection
Following the identification of studies, we applied a Relevance Test I (table 3) and later a Relevance Test II (table 3). This test aims to adjust the initial selection of studies (Pereira & Bachion, 2006).
The Relevance Test I, or Preliminary Relevance Test, was prepared based on straightforward questions about the study, and those who obtained "NO" in response were excluded (Pereira & Bachion, 2006). This first relevance test includes the questions: it integrates the criterion of the time of inclusion, and the study language is included in the investigators' criteria, among others (Pereira & Bachion, 2006).
Table 3 Relevance test I and II
| Relevance Tests I and II | ||
|---|---|---|
| Question | Yes | No |
| Does the study address the theme that is being investigated? | ||
| Operationalization: INCLUDE Studies with the model of the hospital at home and classic hospitalization with cost-effectiveness evaluation Hospital at home and classic hospitalization studies of pediatric and adult and elderly population EXCLUDE Studies of hospital at home and classic hospitalization that address other parameters (such as customer satisfaction risk of falling, among others.) Secondary studies, opinion pieces, reader letters and comments | ||
| Was the study published in the time defined by the SRL researchers? | ||
| The study was published between January 2010 and July 2023 | ||
| Was the study published in the language defined by the researchers? | ||
| The study was published in Portuguese, English, and Spanish. | ||
| Is the study available in full text? | ||
| Does the study involve humans? | ||
Following, the abstracts and references of the studies that were included in the sample are evaluated. Thus, the Relevance Test II is started, which follows the same guidelines as the previous one and in which it is determined which references are or are not included (Pereira & Bachion, 2006). Two investigators carried out this test independently, and, in case of disagreement, a third investigator was consulted (Muñoz et al., 2002).
In Relevance Test I, twelve studies were selected for full reading after removing duplicate studies and checking those that met the inclusion criteria. Then, the Relevance Test II was performed. After its application, five studies were selected for discussion and submitted to a methodological quality assessment test according to the methodology used in each study. The studies selected for the Relevance Test II were all in Full-Text format, thus allowing them to meet one of the parameters necessary to comply with rigor.
To complete this step and make the research more comprehensive, the bibliography of studies selected with the Relevance Test II was analyzed, and no other studies were included in the SRL (Berwanger et al., 2007; Bettany-Saltikov, 2012).
1.5 Assessment of methodological quality
The primary studies included in the systematic literature review will determine the quality of conclusions and the quality of evidence (Bettany-Saltikov, 2012). For this reason, investigators must assess the methodological quality of the selected studies to guarantee a better classification of the degree of recommendation and the level of evidence of the problem under study (Pereira & Bachion, 2006).
Table 4 shows the Level of Evidence and the Score of the Assessment of Methodological Quality of the studies included in the SRL, according to the JBI criteria.
Table 4 JBI Evidence Level and JBI Methodological Quality Assessment Score
| Study | Title | Year | Level of evidence (JBI) | Score of the Assessment of Methodological Quality |
|---|---|---|---|---|
| 4 | Cost-effectiveness of home-based vs. in-hospital treatment of pediatric tuberculous meningitis | 2018 | IV (Economic evaluations) | Score 11/ QME |
| 25 | Costs of outpatient parenteral antimicrobial therapy (OPAT) administered by Hospital at Home units in Spain | 2017 | IV (Economic evaluations) | Score 9/ QME |
| 28 | “Hospital at Home” For Neuromuscular Disease Patients with Respiratory Tract Infection: A Pilot Study | 2013 | I | Score 10/ QME |
| 42 | Home treatment of COPD exacerbation selected by DECAF score: a non-inferiority, randomized controlled trial and economic evaluation | 2018 | I | Score 10/ QME |
| 74 | Intravenous ceftriaxone at home versus intravenous flucloxacillin in hospital for children with cellulitis: a cost-effectiveness analysis | 2019 | I | Score 11/QME |
The studies screened in the Relevance Test II were submitted to the classification of the level of evidence and its methodological quality using the “Critical Appraisal Checklist Tools” (JBI, 2020) and “Levels of Evidence” (JBI, 2013).
Before obtaining the results of the methodological quality assessment, researchers determined that the studies to be included for critical appraisal should have a quality equal to or greater than moderate. All five studies selected to classify the evidence level and assess the methodological quality were included in the systematic review of the literature.
The selection process must be recorded, and using a PRISMA flow diagram (Page et al., 2021) allows the number of included and excluded studies to be documented from the beginning to the end of this step of the systematic review of the literature (Figure 1).
2. Results
A total of five studies were included in this review. They were published between 2013 and 2019 in English. The selected studies have a high level of evidence (except Studies 4 and 25) and high methodological quality.
Regarding compliance with ethical criteria, all the studies respected them throughout the investigative process, having received approval from the ethics committees to which they submitted the research project.
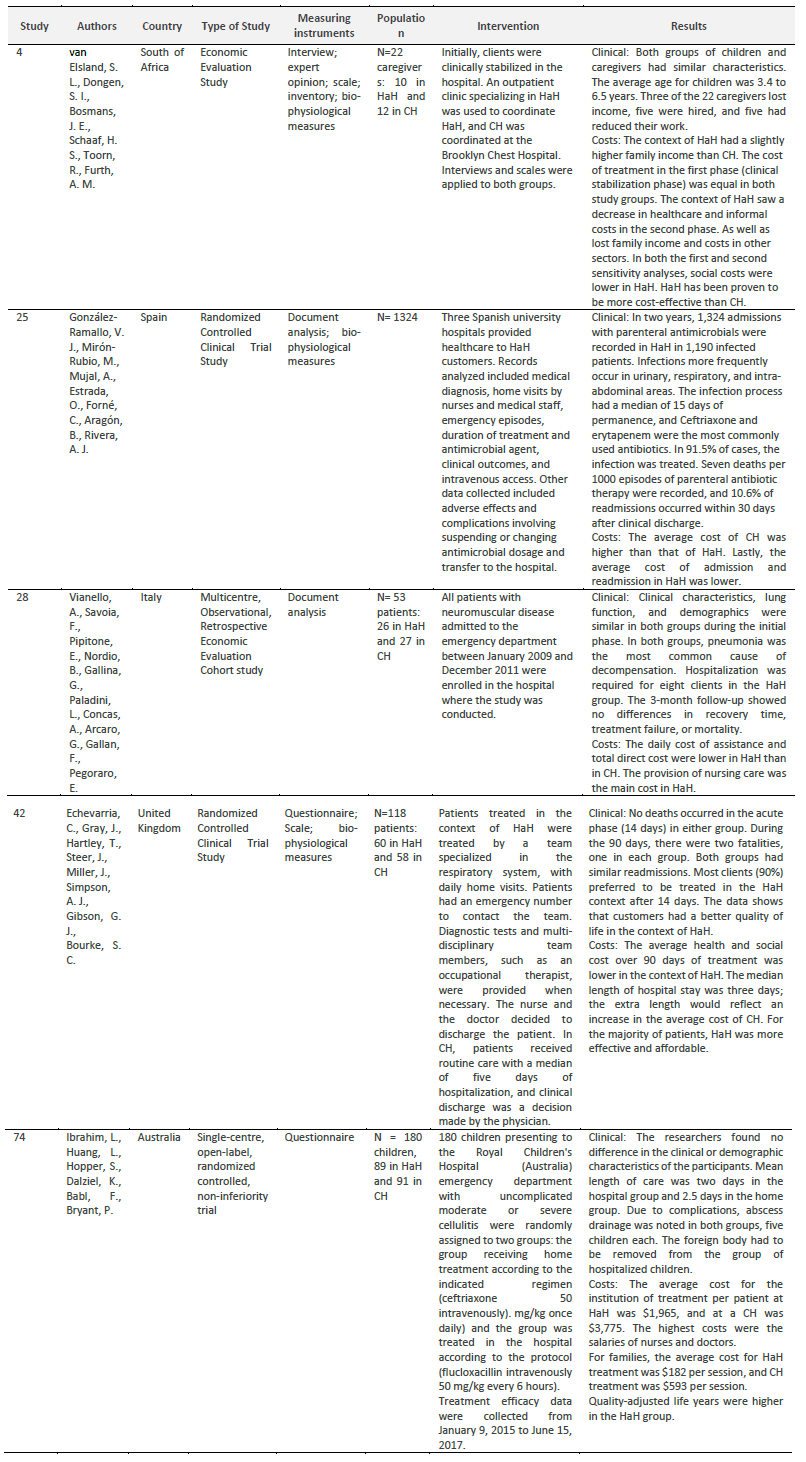
Table 5 describes the studies on authors, country of origin, type of study, measuring instruments, population, intervention, and results.
Quantitative methodology studies are prevalent in studies included in the SRL. Regarding the design of the studies, three are Randomized Controlled Clinical trial studies (Study 25, 42, 74), and the last one is a single-center, open-label; Study 4 is an Economic Evaluation Study, and Study 28 is a Multicentre, Observational, Retrospective Economic Evaluation Cohort study.
3. Discussion
Five studies out of 146 were included in this SRL. In the analysis of the evidence produced in the included studies, it was found that the authors were consensual regarding the HaH model being more cost-effective compared to the CH model (Vianello et al., 2013; González-Ramallo et al., 2017; Echevarria et al., 2018; van Elsland et al., 2018; Ibrahim et al., 2019).
Given the distinct geographic location of the studies, different health services, and different cost perspectives for analysis, we consider the economic advantages for the sustainability of the health service, as well as the effectiveness and safety of the HaH care delivery model, proven. The geographic diversity of the studies allows us to claim a worldwide interest in the cost-effectiveness assessment between HaH and CH.
In analyzing the studies, it was possible to verify that they addressed different pathologies, such as patients with COPD, tuberculous meningitis, neuromuscular disease and infection of the respiratory tract, with cellulitis treated with antibiotic and an investigation in antimicrobial parenteral therapy in patients with different pathology (Vianello et al., 2013; González-Ramallo et al., 2017; Echevarria et al., 2018; van Elsland et al., 2018; Ibrahim et al., 2019).
The study groups were similar in the five studies regarding demographic, clinical, and pathology characteristics.
The authors concluded that the mortality rate did not differ significantly between HaH and CH patients (Vianello et al., 2013; Echevarria et al., 2018). Some authors found that HaH reduces mortality and hospital readmission rates (Vianello et al., 2013; Echevarria et al., 2018; van Elsland et al., 2018). One study concluded that the mortality rate per 1000 HaH episodes was seven deaths (González-Ramallo et al., 2017).
The scores obtained in assessing anxiety and quality of life of patients admitted to HaH were better than those obtained in patients in the context of CH (Echevarria et al., 2018). The quality-of-life factor is higher in HaH (Vianello et al., 2013; González-Ramallo et al., 2017; van Elsland et al., 2018; Ibrahim et al., 2019).
The treatment of HaH in patients with low-risk DECAF scores is clinically effective and safe, and patients have mentioned that in similar clinical situations, they would prefer to be treated at home (Echevarria et al., 2018). The study on the treatment of pediatric tuberculous meningitis reinforces the results of other studies about how treatment can be done at home with adequate clinical support, counseling, and follow-up (van Elsland et al., 2018). In HaH versus CH, 91.5% of patients diagnosed with infection treated in HaH had their situation successfully resolved (González-Ramallo et al., 2017). Research on patients treated at HaH with parenteral antibacterial therapy has shown this to be a safe and effective option (González-Ramallo et al., 2017). Patients treated with HaH who required readmission were those with respiratory infection and amyotrophic lateral sclerosis and, therefore, should not be advised to join HaH (Vianello et al., 2013). HaH, treating children diagnosed with moderate or severe cellulitis with intravenous antibiotics, has been clinically proven to be safe and effective while increasing parents' and children's satisfaction (Ibrahim et al., 2019).
Of the studies included in the SRL, one addresses the social perspective, loss of productivity, income, and employment during the treatment period, having concluded that there was a change in the total value of monthly income in both groups participating in the study, with the highest income being in the group of HaH (van Elsland et al., 2018).
In general, costs are lower in the HaH context, and the most expensive service was nursing, with the two most costly parameters in CH being inpatient and social services (Echevarria et al., 2018). The healthcare costs were similar in the period necessary for the clinical stabilization of patients. In contrast, later, these costs in the HaH group were 95% lower than those in the CH group (van Elsland et al., 2018). Informal costs lost productivity, and costs in other sectors were also lower for the HaH group (van Elsland et al., 2018).
The researchers of one of the selected studies presented the costs related to the total treatment of the infectious process. They concluded that the average cost of the care model was higher in CH (González-Ramallo et al., 2017). In HaH, for calculating average costs, costs with support and general expenses, with the pharmacy and with the multidisciplinary health team, complications of the clinical picture, and the need for care in the hospital emergency service were included. The cost of admission and readmission for the patient 30 days after clinical discharge in HaH was lower than the average cost of hospitalization in CH (González-Ramallo et al., 2017). Daily care and the total direct cost were lower for HaH patients than those treated in CH (Vianello et al., 2013).
The cost-effectiveness analysis of the intravenous cellulitis treatment was more effective and less costly in HaH than in CH. Even patients treated at HaH but hospitalized for complications did not incur additional costs (Ibrahim et al., 2019).
Researchers from different studies suggested some aspects to improve the research area of analyzing the cost-effectiveness of HaH and CH. The researchers state that, for a complete analysis, it is necessary to include the satisfaction of patients and caregivers and expand the perspective of health costs, not limited to the context of the regional or national health service. They highlight the importance of including data on quality of life, mortality and morbidity rates, and health outcomes for the completeness of the cost-effectiveness analysis. The researchers propose political investment in HaH to improve the family impact and contribute to lower costs (Vianello et al., 2013; González-Ramallo et al., 2017; Echevarria et al., 2018; van Elsland et al., 2018; Ibrahim et al., 2019).
The results previously expressed are the culmination of this investigation. However, the results do not demonstrate the limitations or barriers identified by the researchers. The language restriction may have led to the exclusion of studies; however, we consider that the inclusion of the English language, the language par excellence of scientific publication, minimizes this limitation, being an added value for the study. There was a scarcity of studies that met the inclusion criteria, and those that met had low evidence. Of the five studies selected, only one included caregivers/family in the investigation, which is a basis for providing care in the context of HaH. It is essential to reflect that costs are not merely monetary. For this reason, the studies must also consider the social and health costs for the clients, family members, and caregivers (including stress levels, clinical results, satisfaction with care provision, family income, and social support, among others).
4. Implications for clinical practice
For nurse management and clinical practice to implement HaH, it is necessary to form a team with elements that belong to the health institution, as these already embody the organization's vision, mission, and values. In the context of HaH, the care provided at home is provided by the institution, and its principles must be respected in all the models adopted for providing care. Another fundamental aspect is that the team providing care is multidisciplinary due to the possible complexity of the pathology or the family and social context in which the patient finds himself.
Creating a HaH unit involves several resources and requires elements of management competence. In this sense, it is essential that in the planning and implementation of HaH units, a nurse with management skills is present in the team.
The role of the nurse manager in the HaH scope calls for developing protocols, guidelines, and directives based on scientific evidence that ensure the quality of care and its safety (Ordem dos Enfermeiros, 2018). In addition to the safety of care, the nurse manager must ensure the creation of safe environments and participate in the remodeling, design, and adequacy of the physical space of the home environment. By recognizing the absence of the nursing team in monitoring patients 24 hours a day, as is done in a classic hospitalization environment, the nurse manager must prioritize the team teaching, instruction, and training procedures for the family or caregivers according to the needs of the patients. The guarantee of assistance within 24 hours is essential to obtain better clinical results, and the availability of a bed in a ward is important for a possible hospital readmission of a patient on HaH.
In this case, the nurse manager has the skills to prioritize, identify, and assess the problems and risks for patients, caregivers, and family members, placing them in a hierarchy (Ordem dos Enfermeiros, 2018). Regarding material resources, it is essential to highlight the need to ensure the proper functioning of the procurement method and stock management, which should be distinct from the hospital procurement and stock, to facilitate management.
Regarding costs, it is important to reflect that the costs are not merely monetary and that the costs for patients, families, and caregivers must also be considered from a social and health point of view (considering levels of stress, clinical results, satisfaction with the provision care, family income, social support, …).
Finally, the nurse manager must participate in the control and management of the HaH unit/service, given not only their competence to perform but also the fact that HaH is a recent model in Portugal and lacks the need for high management of costs. The need to determine a cost-effective model can be helped with the construction of health outcome assessment indicators, with the main objective of determining health gains (Ordem dos Enfermeiros, 2018).
Conclusion
Internationally, and according to the results obtained, HaH is a model established in developed and developing countries. Hence, the need to analyze care provision with a better cost-effectiveness ratio is notorious. In uniformity, the conclusions of the studies allowed us to understand, although with some parameters to be analyzed (namely the social cost for the patient and the family), that HaH is the most cost-effective model to provide health care in specific clinical diagnoses. However, it is necessary to reflect on the non-existence of an ideal HaH model that can be generalized, given the varied socio-economic and financial contexts. The primary needs of the patients, family/caregiver, as well as sanitary, hygienic, and housing conditions, must, even so, be mandatory assessment in any HaH protocol.
In future primary studies, it is relevant to deepen the social and family cost of HaH compared to CH and include them in the economic analysis. We also recommend more rigorous economic evaluation studies with a complete clinical and economic cost and results description.
The high cost of hospitalization is known to society, families, and patients, which is one of the reasons for implementing hospitalization at home.
In short, with the findings of this study, we intend to contribute to the discussion about the sustainability of the NHS and better scientific evidence in nursing management, giving nurse managers tools to carry out more active and grounded work.
Author contributions
Conceptualization, M.I.M., A.P.P. and M.R.S.; data curation, M.I.M. and A.P.P.; formal analysis, , M.I.M., A.P.P. and M.R.S.; investigation, M.I.M., A.P.P. and M.R.S.; methodology, M.I.M., A.P.P. and M.R.S.; project administration, M.I.M., A.P.P. and M.R.S.; resources, M.I.M.; supervision, A.P.P. and M.R.S.; validation, A.P.P. and M.R.S.; visualization M.I.M., A.P.P. and M.R.S.; writing-original draft, M.I.M.; writing-review and editing, A.P.P. and M.R.S.