Introduction
Nurses are the greatest health workforce and have a crucial role in pharmaceutical care (PC), namely preparing and administering medication, assessing therapeutic and adverse effects, managing medication adherence, educating patients in self-medication, and identifying patient needs (De Baetselier et al., 2021).
Nurses play their role in pharmaceutical care within a health team composed of other professionals, mainly physicians and pharmacists, that designs, implements, and monitors the therapeutic plan. Interprofessional work is vital for improving health outcomes (De Baetselier, Dijkstra, et al., 2022).
History says that nurses’ roles in pharmaceutical care focused on preparing and administering medication and monitoring its effects. Nursing care evolved alongside the nursing profession, and by the end of the 21st century, medication administration as a means to improve the patient’s quality of life was part of health care (Hepler & Strand, 1990). More recently, health care came to include the enhancement of medication use and health outcomes. However, the evolution of nurses’ roles in recent years brought along new responsibilities, including around 60 PC-related tasks (De Baetselier, Dilles, et al., 2022; Dijkstra et al., 2021). These new tasks include obtaining timely, accurate, and complete medication histories, proposing and implementing interventions to prevent drug-related problems, and, the most controversial in Portugal, proposing medication initiation/discontinuation included in the nurse prescriber form. Although the Portuguese nursing regulatory body does not foresee these competencies, it emphasizes new ones, such as medication reconciliation.
Performing these responsibilities requires new competencies: a coherent set of knowledge, skills, and attitudes for use in various care contexts. Competencies in PC are developed from the beginning of the future nurse’s academic education, but it is not clear how prepared nursing students are to provide safe and effective PC (van Mil et al., 2004).
Academic education ensures the quality of care, which means that inadequate nursing education significantly negatively impacts the quality of care, resulting in greater in-hospital mortality (De Baetselier, Dijkstra, et al., 2022). Recent studies show that PC-related nursing education should be improved (Escrivá Gracia et al., 2019; Salehi et al., 2021; Stolic et al., 2022) and that nursing curricula are inadequate (Seguro et al., 2023) and differ between levels of education and countries (De Baetselier, Dijkstra, et al., 2022).
This study is part of the DeMoPhac project (Development of a model for nurses’ role in interprofessional pharmaceutical care), which the European Commission funds. The project is an international collaboration between 14 European countries that seeks to explore the roles and competencies of nurses. To meet the new demands for improving nurses' PC competencies and address any uncertainty about how nursing curricula contribute to attaining this goal, it is imperative to identify the perceptions of Portuguese nursing students regarding the adequacy of nursing curricula to prepare them for PC practice and their competencies in this field.
Therefore, this study aimed to determine how nursing students perceive the adequacy of nursing curricula for developing knowledge, skills, and attitudes in PC and assess their competencies in this area.
1. Methods
1.1 Type of study and sample
A descriptive, cross-sectional study was conducted on 4th-year undergraduate and master’s students from five Portuguese nursing schools, corresponding to 12% of all schools in Portugal. A convenience sample was obtained from known and privileged contacts of the nursing schools who agreed to participate.
Data collection was authorized by the directors’ boards of the nursing schools and the ethics committee of the Health Sciences Research Unit: Nursing (opinion 747/01-2021).
Participants have the option to withdraw at any time without penalty. Anonymity was ensured by not identifying participants in any way. Data will be analyzed as a whole.
1.2. Data collection instrument
For data collection, the instrument developed by De Baetselier, Dijkstra, et al. (2022) was used, which included for the DeMoPhac project three questions specific to the Portuguese context about students’ knowledge. The questions were formulated by all project partners, translated into European Portuguese, and validated through consensus by a panel of seven Portuguese experts. The questionnaire consisted of multiple parts, starting with demographic questions. The second part consisted of questions assessing if nursing curricula adequately prepared individuals for PC practice and the development of knowledge, skills, and attitudes in PC. Another section focused on assessing the students’ competencies in PC, specifically their knowledge, skills, and attitudes. Finally, there was a question asking the students to rate their own PC competencies.
Nurses' roles in PC were assessed through 86 questions utilizing the competence framework proposed by Dijkstra et al. (2021). Knowledge was evaluated using 55 multiple-response questions, consisting of 21 general knowledge questions and 34 questions on medical, surgical, and mental health pathology based on real-life practical exercises in PC. Students' abilities and attitudes were evaluated using a 4-point Likert scale consisting of 16 and 13 items, respectively. The scale ranged from totally disagree to totally agree. The PC competency level was evaluated using a 0-200-point scale with three dimensions: knowledge (0-113 points), skills (0-48 points), and attitudes (0-38 points).
Data collection occurred online from March to April 2021. Students were requested to access a website designed to administer the questionnaire. As the questionnaire was lengthy, respondents had the option to pause and resume it.
2. Results
2.1 Demographic characterization
A total of 57 students, aged between 19 and 62 years, with a median age of 23 and an IQR of 16, completed the questionnaire. The majority (73.7%) were women aged 42. Undergraduate students accounted for 59.6% (34) while master students accounted for 40.4% (23). Work experience in health care ranged from 1 to 41 years with a median of 2 and an IQR of 10.5. Twenty-two students worked in health (38.6%). Weekly workload in health ranged from 1 to 48 hours, with a median of 35 and IQR of 15.25.
2.2 Perception of the adequacy of nursing curricula to prepare students for PC practice
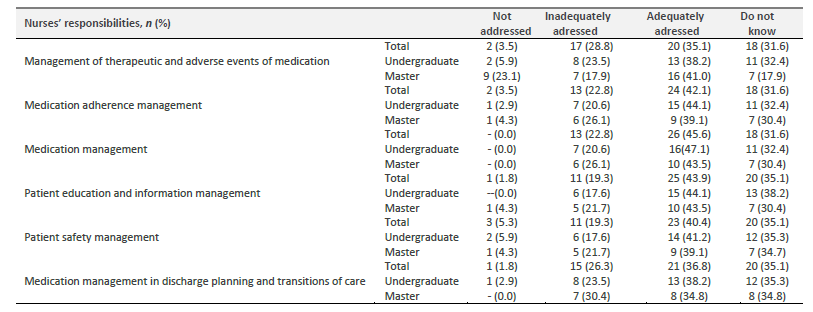
Participants were asked whether nurses’ responsibilities in PC are adequately addressed in the current nursing curricula. Using a scale of 0 to 5, where 0 corresponds to not adressed at all and 5 to adequately addressed, responses ranged from 0 to 5 with a median of 2.5 and an IQR of 1. Responses from both undergraduate and master students had a median of 2.5.
Undergraduate and master students identified medication adherence management (24; 42.1%) and patient education and information management (25; 43.9%) as adequately addressed responsibilities. Sixteen undergraduate students (47.1%) referred to medication management while 16 master students (41%) mentioned management of therapeutic and adverse events of medication.
Participants were asked whether they felt adequately prepared by the current curricula to develop PC competencies. Using a scale of 0 to 5, where 0 corresponds to not prepared at all and 5 to adequately addressed, responses had a median of 3 and an IQR of 2. Undergraduate students showed a greater perception, with a median of 3 and IQR of 2, than master students, with a median of 2.5 and an IQR of 2.
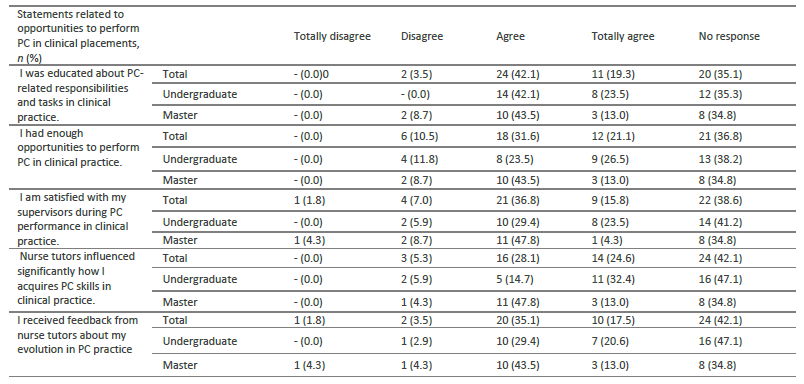
Most students did not respond to the question about opportunities to perform PC in clinical placements. Twenty-four students (42.1%) indicated that they were educated about PC-related responsibilities and tasks, and 21 were satisfied with their supervisors (36.8%). Fourteen undergraduate students (42.1%) indicated that they were educated about PC-related responsibilities and tasks, and 11 master's students were satisfied with their supervisors (47.8%).
2.3 Knowledge, skills, and attitudes in PC addressed in nursing curricula
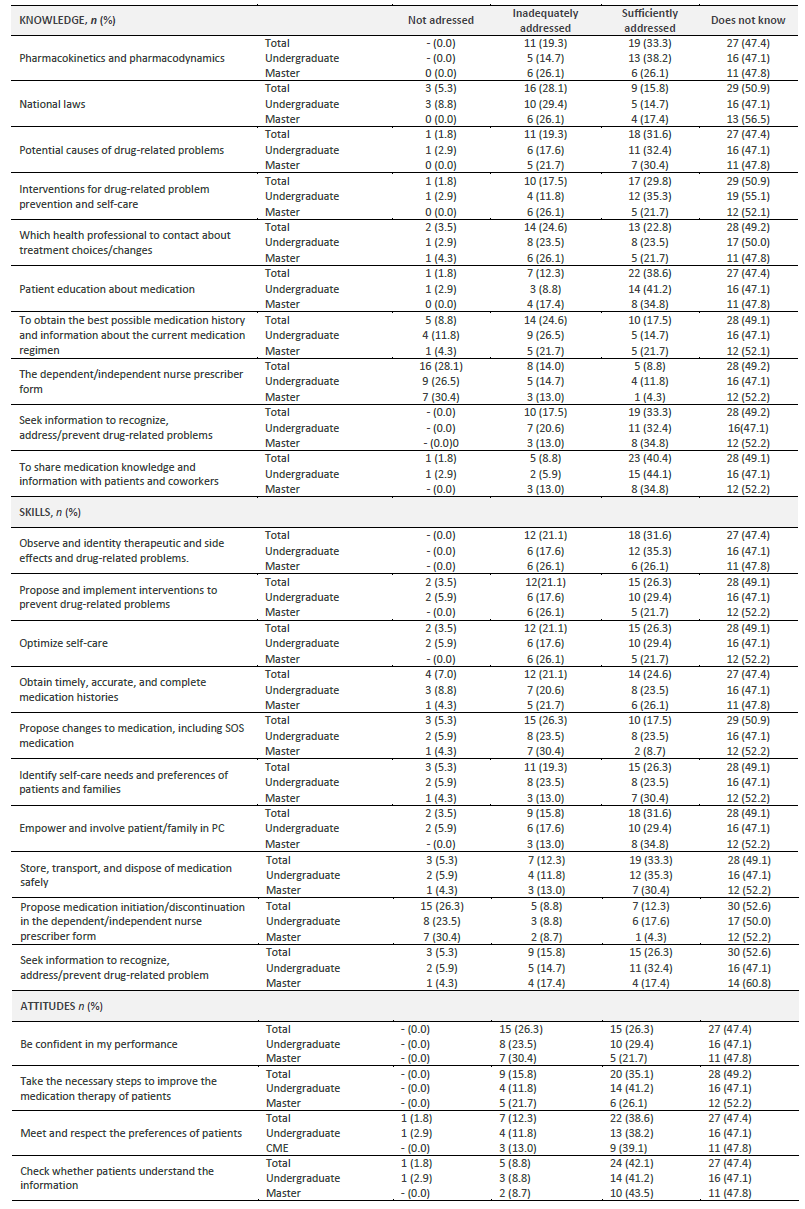
Most respondents were not aware if PC competencies (knowledge, skills, and attitudes) were addressed in nursing curricula.
However, the following PC competencies were mentioned as being addressed adequately in nursing curricula:
Knowledge to share medication knowledge with patients and coworkers (23; 40.4%) and provide medication education to patients (22; 38.6%);
Skills to store, transport, and dispose of medication safely (19; 33.3%), observe and identity therapeutic and side effects and drug-related problems (18; 31.6%), and empower and involve the patient/family in PC (18; 31.6%);
Attitudes to check whether patients understand information (24; 42.1%); meet and respect the preferences of patients (22; 38.6); and take steps to improve the medication therapy of patients (20; 35.1%).
Undergraduate students identified these competencies:
Knowledge to share medication knowledge with patients and coworkers (15; 44.1%) and provide medication education to patients (14; 41.2%);
Skills to observe and identity therapeutic and side effects and drug-related problems (12; 35.3%) and store, transport, and dispose of medication safely (12; 35.3%);
Attitudes to check whether patients understand information (14; 41.2%), take the necessary steps to improve the medication therapy of patients (14; 41.2%), and meet and respect the preferences of patients (13; 38.2%).
Master students identified these competencies:
Knowledge to provide medication education to patients (8; 34.8%), seek information to recognize, address/prevent drug-related problems (8; 34.8%), and share medication knowledge with patients and coworkers 8 (34,8%);
Skills to empower and involve the patient/family in PC (8; 34.8%) identify self-care needs and preferences of patients and families (7; 30.4%) and store, transport, and dispose of medication safely (7; 30.4%);
Attitudes to check whether patients understand information (10; 43.5%) and meet and respect the preferences of patients (9; 39.1%).
2.4 Student competencies in PC
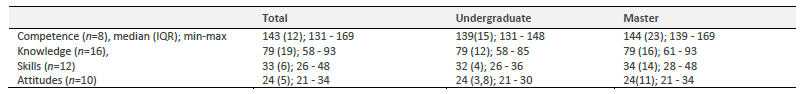
Only a few students answered the questions about assessing their competencies in PC. Nevertheless, the competencies reported by the respondents ranged from 131 to 169 points, with a median of 143.0 (IQR of 12.0). Of note, master's students had a slightly higher median score (144.0; 23.0) than undergraduate students (138.5; 15.0).
In the competence dimensions analyzed, all students showed an equal median of 79 in knowledge, an equal of 24 points in attitudes, and an equal median in skills ranging from 32 points among undergraduate students and 34 points in master students.
Participants were asked how they rated their competencies in PC (their performance in healthcare to enhance medication use and health outcomes. Using a scale of 0 to 5, where 0 indicates not competent and 5 very competent, the 30 responses had a median of 3 points and an IQR of 1, with scores ranging from 1 to 5 points.
3. Discussion
The results are discussed in the same order in which they are presented: Adequacy of nursing curricula to prepare students for PC practice; Knowledge, skills, and attitudes in PC addressed in nursing curricula; and Student competencies in PC. This section first addresses the characterization of the sample and ends with the limitations of the study.
All institutions invited to participate in the study concurred, yet there was a low rate of student involvement in comparison to the total potential respondents. The reasons behind this include students' sense of being evaluated and subsequent fear of failure, little available time, limited familiarity with nursing curricula, and possible miscommunication during the implementation of the data collection plan by responsible parties at each institution. However, the primary reason is likely associated with the length of the questionnaire, which, despite permitting pauses, is rather extensive. Few students responded to all questions. Consequently, future applications of this questionnaire should be divided into multiple parts, using only one section at a time. To avoid losing pertinent information, it is recommended that participation be expanded to a broader range of institutions.
Although the population of master's students is comparatively smaller than that of undergraduate students, nearly two-fifths of the respondents were master's students. This indicates that these respondents possess greater understanding and maturity in reflecting on the practice of care and the skills needed for PC.
3.1 Adequacy of nursing curricula to prepare students for PC practice
Students perceived nurses' responsibilities in PC as being sufficiently addressed in nursing curricula. However, the majority feel that the responsibilities are neither addressed or inadequately addressed in the international literature (De Baetselier, Dilles, et al., 2022). This finding is noteworthy and requires our attention and reflection, as it potentially jeopardizes the education that ensures the necessary quality of care. Moreover, these challenges hinder the ability of nurses to achieve the desired level of mobility both in Europe and globally. Furthermore, it undermines the desired identity of the nursing profession and its position in fulfilling specific roles within the healthcare team. Undergraduate and master’s students identified medication management and management of therapeutic and adverse effects as the most important tasks in their curricula but noted that such limited engagement does not ensure quality healthcare.
Nevertheless, students felt that current curricula provided adequate preparation for acquiring competencies related to PC. This perspective may be influenced by the fact that nurses believe that their competencies are related to the preparation and administration of medication, as identified by Luokkamäki et al. (2021). However, the majority of students do not provide answers when asked about their opportunities to perform PC in clinical placements. One cannot help but wonder if they do not answer because they are unaware of these opportunities or do not know their competencies in PC. Thus, the question remains unanswered.
3.2 Knowledge, skills, and attitudes in PC addressed in nursing curricula
The vast majority of students did not know whether their nursing curricula addressed nurses’ roles in PC (knowledge, skills, and attitudes).
Less than three-fourths of those who believe nurses’ roles were adequately addressed in nursing curricula cited the roles of checking whether patients understood information, sharing medication knowledge with patients and colleagues, providing medication education to patients, and meeting and respecting the preferences of patients. Both undergraduate and master’s students perceive these teaching roles in a similar manner. They also believe the following roles are not addressed: obtaining timely, accurate, and complete medication histories; seeking information about current medication regimen; and proposing medication initiation/discontinuation. In reality, prescribing medications is not part of their roles in Portugal, although it may be allowed in the future in certain contexts and circumstances (Martiniano et al., 2015;) as is already the case in some countries (Maier, 2019).
3.3 Student competencies in PC
Few students completed the 86 questions to assess their competencies in PC, likely due to their length. For future research, it will be crucial to develop a simpler instrument to assess nurses' roles in PC or to reduce the number of items in the current instrument.
It was found that the respondents had good competencies (which was in the third quartile), with master’s students having slightly higher competency scores. Although this result may be surprising due to how inadequately PC is addressed in curricula, it is important to note that the students with the greatest difficulty were likely those who did not complete the questionnaire. This observation highlights the importance of developing a valid, reliable, and accurate tool to assess nurses' roles in PC. In addition, the tool should be designed to assess the difficulty of the responses to allow for differentiation of students based on their skill level. This could be one reason why the skill gap between undergraduate and master’s students is not larger. The second possibility is that the curricula do not promote differentiated training for students in different cycles of study, as required. Assessing competencies in higher education is complex, as many authors have pointed out (Sáez-López et al., 2021; Zlatkin-Troitschanskaia et al., 2015). It is impossible to measure competence through a one-time evaluation or a written instrument. While these methods may provide some insight, a valid and reliable assessment can only occur within a contextualized setting. (Sáez-López et al., 2021). These authors point to self-observation as one of the techniques for assessing competencies in higher education (Sáez-López et al., 2021), where the student becomes the main actor in knowing themselves and assessing their competencies throughout the teaching-learning process.
Student perceptions of competencies appear to be lower than demonstrated competencies. This could indicate that the instrument used to assess competencies has a low level of difficulty or that the few students who responded were the most competent. In addition, the development of competencies in students requires contextualized competency assessment.
3.4 Limitations
This study is limited by a small number of questionnaire responses and the long instrument used to assess PC competencies. The length of the instrument negatively affected the completion rate of students despite prior notice and the option to pause the questionnaire. The difficulty level of the questionnaire items was evaluated by experts. However, it may be important to conduct an assessment with students in advance to determine the difficulty of each item. This will help to eliminate the items that are too easy and too difficult, which could hinder the ability to differentiate in the assessment. Another limitation is the assessment of competencies using questionnaires, which ideally require contextualized assessment, which was not feasible in this study.
The lack of substantial elaboration in the creation of skill-based curricula may have impacted students' understanding of necessary health care skills. In addition, traditional nursing practice revolves around such mundane tasks as educating about medication preparation and administration, monitoring the effectiveness of treatment, and patient education.
The high number of students who dropped out of the questionnaire calls for future research to explore alternative reasons behind their withdrawal.
Conclusion
Students perceived that nursing curricula sufficiently prepared them for PC practice and the development of knowledge, skills, and attitudes in PC.
None of the specific nurses’ roles were considered sufficiently addressed in their curricula by more than half of the respondents. The roles most represented were medication regimen management and patient education and information.
The assessment of PC competencies was positive, although it is important to consider the limited number of respondents and an assessment framework that focuses on the cognitive dimension.
This study is valuable in highlighting weaknesses in pharmaceutical nursing education. Weaknesses include curricula that focus on topics rather than competencies, limited content related to PC, and failure to meet the current PC model that ensures quality patient care.
Immediate curricular changes are recommended with an emphasis on PC and skill-based teaching. Further research is needed to develop additional tools to assess nurse competencies in PC while ensuring that assessment occurs in a practice setting.
Current standards for pharmaceutical nursing education have not been studied in depth, so further research is needed to understand the growth and social recognition of this education.
Author contributions
Conceptualization, L.B., P.F., M.I.F. e J.S.; data curation, L.B.; formal analysis, L.B., P.F., M.I.F. e J.S.; funding acquisition, L.B., P.F., M.I.F. e J.S.; investigation, L.B., P.F., M.I.F. e J.S.; methodology, L.B., P.F., M.I.F. e J.S.; project administration, L.B.; resources, L.B., P.F., M.I.F. e J.S.; software, L.B., P.F., M.I.F. e J.S.; supervision, L.B., P.F., M.I.F. e J.S.; validation, L.B., P.F., M.I.F. e J.S.; writing-original draft, L.B., P.F., M.I.F. e J.S.; writing-review and editing, L.B., P.F., M.I.F. e J.S.