Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.20 no.6 Lisboa dez. 2013
https://doi.org/10.1016/j.jpg.2013.03.006
ENDOSCOPIC SPOT
Endoscopic resection of esophageal granular cell tumor
Ressecção endoscópica de tumor de células granulares do esófago
Manuela Canhotoa,∗, Sandra Barbeiroa, Filipe Silvaa, Bruno Arrojaa, Cláudia Gonçalvesa, Isabel Cotrima, Cristina Amadob, Maria Fernanda Cunhab, Helena Vasconcelosa
a Department of Gastroenterology, Centro Hospitalar Leiria-Pombal, EPE, Leiria, Portugal
b Department of Anatomopathology, Centro Hospitalar Leiria-Pombal, EPE, Leiria, Portugal
*Corresponding author
Granular cell tumor (GCT) was first reported by Abrikossoff by the name of granular cell myoblastoma.1
These tumors are found mainly in skin, oral cavity and digestive tract. Most are benign lesions, but there are reports that malignancy may occur in 1-2%.2
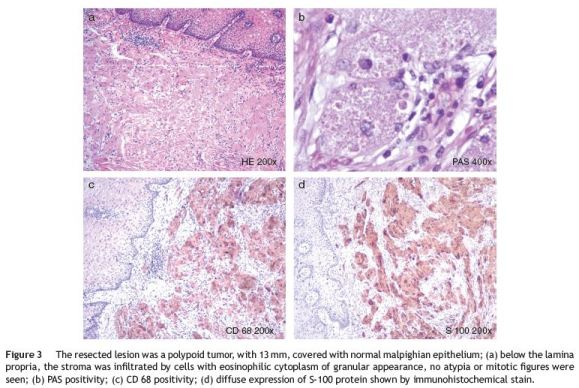
The diagnosis is made by histopathology. GCT has eosinophilic cytoplasmatic granules and positivity for S-100 protein and neuron specific enolase. Although their celular origin remained controversial for years, currently it is thought that GCT originates from Schwann cells.2
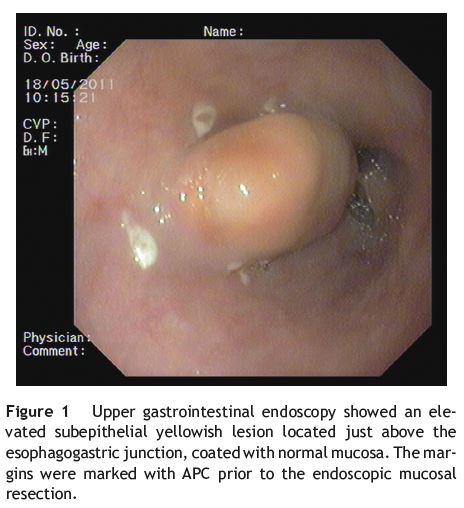
A 54-year-old man presented with epigastric pain and was submitted to upper endoscopy. The endoscopy revealed a 10mm subepithelial esophageal lesion above the esophagogastric junction. The lesion had a yellowish-white appearance, covered with normal mucosa, and was firm when prodded with the biopsy forceps. Although these characteristics are typical of CGT, it is not possible to make an accurate differential diagnosis from other subepithelial lesions such as lipomas by endoscopy.3
Biopsies (bite-on-bite) were performed and histopathological evaluation was suggestive of GCT.
The lesion was characterized by ecoendoscopy as hypoechoid, heterogeneous and limited to the submucosa. Ultrasonography evaluation was important in the pretreatment evaluation to confirm that the tumor was limited to the submucosa and presented minimal risk of perforation during resection.4
The patient was being evaluated for an aortic aneurysm and a thoracoabdominal computed tomography was performed with no other lesions.
Due to the most likely benign nature of the lesion, anual follow-up3 or endoscopic resection of the lesion were discussed with the patient, who agreed with the endoscopic approach.
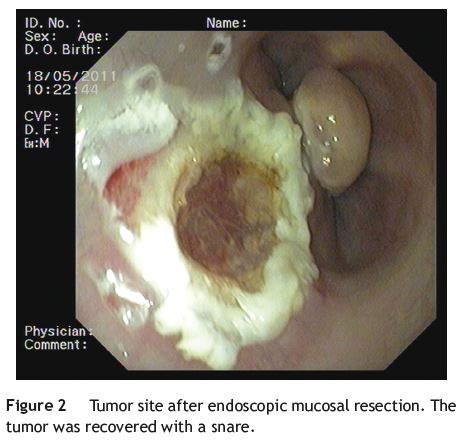
The lesions borders were marked with Argon-plasma coagulation (Fig. 1), and submucosal injection (10 ml) of sodium chloride 9% solution and adrenaline (1:100 000) elevated the lesion that was completely removed (Fig. 2) with a snare (Endocut® mode 2, ICC200, ERBE Elektromedizin GmbH, Germany). There were no procedure related complications.
The histopathological evaluation confirmed the diagnosis (Fig. 3) and the surgical margin was tumor-free. The tumor site was reviewed six months later, with no lesion.
There are no current guidelines for the treatment of GCT. Two different approaches are possible: endoscopic follow-up for lesions <10mm or removal of larger lesions (>20 mm), specially when symptomatic or suspicious of malignancy.4 Malignant lesions are usually larger than 4 cm, with rapid growth and tend to recur after resection. Endosonography allows evaluation of the tumor, its extent and suitability for endoscopic resection.4
Fanburg-Smith and colleagues5 proposed six histological criteria to determine possible malignancy. If none of these criteria are present, the tumor is benign, and additional treatment or follow-up is not considered necessary by these authors,5 but no data exists to determine the cost effective approach in the management of GCT, and the risk/benefit of each approach must be considered case by case, involving the patient in decision making.
References
1. Abrikossoff A. Uber Myome, ausgehend von der quergestreiften wilkuerlichen muskulatur. Virchows Arch Pathol Anat. 1926;260:215-33. [ Links ]
2. Aoyama K, Kamio T, Hirano A, Seshimo A, Kameoka S. Granular cell tumors: a report of six cases. World J Surg Oncol. 2012;10:204. [ Links ]
3. Zhong N, Katzka DA, Smyrk TC, Wang KK, Topazian M. Endoscopic diagnosis and resection of esophageal granular cell tumors. Dis Esophagus. 2011;24:538-43. [ Links ]
4. Nakajima M, Kato H, Muroi H, Sugawara A, Tsumuraya M, Otsuka K, et al. Esophageal granular cell tumor successfully resected by endoscopic submucosal dissection. Esophagus. 2011;8:203-7. [ Links ]
5. Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG. Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol. 1998;22:779-94. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
*Corresponding author
Correio eletrónico: manela_vc@yahoo.com (M. Canhoto).
Received 16 January 2013; accepted 22 March 2013













