Leishmaniasis is an endemic disease in Portugal, affecting immunocompetent and immunosuppressed patients.1 The gold standard of diagnosis is demonstration of parasites in stained tissues - bone marrow, spleen, lymph nodes, liver, and skin (cutaneous forms) - or in culture. We report a case of accidental discovery of Leishmania in peripheral blood of an immunocompromised patient with several comorbidities.
A 53-years-old man, Caucasian, homeless, with active inhaled drug addiction and a history of heart failure due to the abuse of substances, was admitted into the Department of Infectious Diseases from our Hospitalar Center with a productive cough, dyspnea and diarrhea. Physical examination showed: poor hygiene, emaciated, tachycardia, wheezing at pulmonary auscultation and oral candidiasis; without fever, palpable organomegaly, adenopathy or skin lesions.
Analytically: hemoglobin 99 g/L; white blood cells 4.73 x109/L (neutrophils 76%, lymphocytes 21%); platelets 115 x109/L; Dimer D- 3607 µg/L (RV: < 230); C-reactive protein 31.1 mg/L (RV< 5.0); urine examination positive for cannabinoids, cocaine metabolites and opiates. VIH1 positive: viral charge - 6140000.0 copies/mL, T Helper lymphocytes (CD4+) - 50.1 cells/ µL. Angio-CAT showed ground glass densification areas throughout the lung, suggesting the hypothesis of drug inhalation pneumonitis.
During hospitalization, he was diagnosed with: inaugural HIV/AIDS infection, pneumocystis jiroveci respiratory infection, colitis to Clostridium difficile. He was treated with trimethoprim, sulfamethoxazole, vancomycin, prednisolone and anti-retroviral therapy.
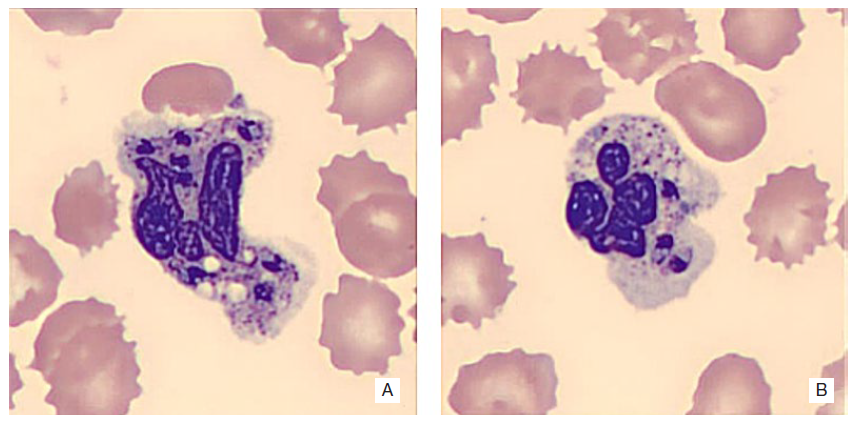
In a routine blood count order, and by observation of the peripheral blood smear, forms of amastigotes of Leishmania spp. were unexpectedly observed (Figs. 1 and 2).
His condition progressed unfavourably with acute hypertensive pulmonary edema, heart failure and progressive renal failure. The patient died on the 21st day of hospitalization.
The appearance of Leishmania in peripheral blood is rare and is indicative of marked and prolonged immunodeficiency, in this case due to HIV infection.
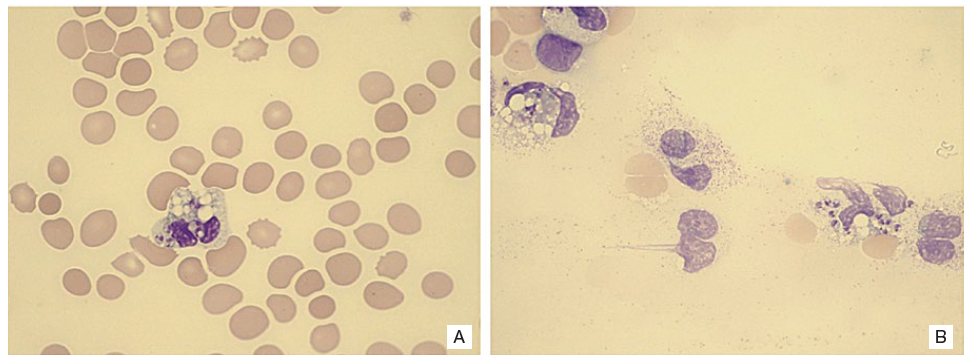
Figure 1: Peripheral blood smears showing amastigotes of Leishmania spp. in the neutrophyls (A) and near to destroided cells (B). May-Grunwald-Giemsa staining, 1000x magnification.