lntroduction
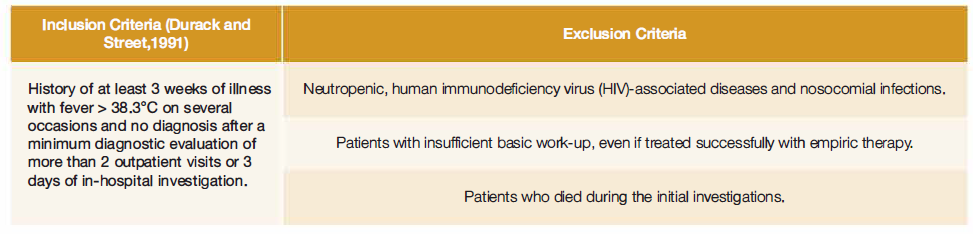
Fever of unknown origin (FUO) was first mentioned in 1930 by Alt and Barker,1 but only in 1961 a standardized clinical definition was made by Petersdorf and Beeson.2 They defined FUO as a body temperature higher than 38.3ºC on three or more occasions, with more than three weeks of disease duration, and with no established diagnosis after one week of inpatient evaluation.2 This definition has changed over the years to better define FUO and to allow an improved diagnostic approach. Durack and Street3 in 1991 changed the study period to 3 days of hospitalization or more than 2 medical visits. Since then, several series have been published with some authors proposing to replace the previously established period time of study with a minimal diagnostic work-up required after which the diagnosis remains unknown.4-6The investigations that should be included in this protocol remain a matter of debate.5 An example of a possible work-up is the proposal defined by Mulders-Manders in 20154 and the recent suggested structured approach by Wright and Auwaerter.7
Durack and Street further classified FUO into 4 categories: classic, nosocomial, neutropenic, and that associated with HIV infection.3
The spectrum of diseases responsible for FUO differs with geographical location, socio-demographic and economic status, age, and other factors.5,8Several factors have been shown to influence the diagnosis but these differences are still poorly understood.5,9
There are more than 200 possible diagnoses, including typical and atypical manifestations of common disorders but also rare conditions, which makes the clinical approach a challenge.4,6,10lnfections, neoplasms, non-infectious inflammatory diseases (that comprises connective tissue diseases, vasculitis syndromes, and granulomatous diseases)11 are the etiologies most frequently observed. However, up to 50% of cases remain unclear.12,13The undiagnosed cases are generally described as having a benign course with eventual resolution of symptoms.6,9,10
Fever is a common condition present in many illnesses. When fever persists and its origin remains unclear after a thorough investigation, it becomes a challenge even to modem medicine.7,8
This study aims to better understand our local epidemiology and which clinical approach is most commonly used. Consequently, we aim to improve the diagnostic approach and clinical care provided to patients with FUO in our setting.
Methods
Study Design and Setting
We conducted a descriptive and retrospective study of patients admitted to an internai medicine department of a tertiary reference university hospital between 1 January 2016 and 31 December 2017.
This is a public hospital which directly serves a population of around 465 000 habitants, and indirectly around 2 million people, according to national data from 2017.
Study Population
The clinical records of all patients admitted during the study period were consulted to select the FUO cases.
lnclusion and exclusion criteria may be seen in Table 1.
The final diagnose registered in the discharge letter or follow-up appointments was assumed as main outcome. The etiologies were divided into 5 types: infections, malignancies, non-infectious inflammatory diseases (NIID), miscellaneous and undiagnosed.
Data Abstraction and Analysis
FUO cases were identified and included in the study after validation by a second author. Clinical data were anonymized and extracted by the main investigator into a Microsoft Excel spreadsheet.
lnformation about the diagnosis, duration of illness, length of stay, and the complementary diagnostic tests performed in each case was collected.
Continuous variables were summarized as mean ± standard deviation (s.d.), or median and standard deviation. Nominal variables were summarized as counts and percentages.
Ethical Consideration
The study was approved by the Ethics Committee of the Hospital. AII identifiable patient information was anonymized.
Results
Between January 2016 and December 2017, 9401 adult patients were admitted to our internai medicine department. Of these, 55 (0.6%) met the criteria for FUO, 35 in 2016 and 20 in 2017.
Of the 55 patients, 32 (58.2%) were male. The patients had a median age of 57.3 years (ranging from 19 to 93 years); 20 patients were 65-year-old or older (36.4%).
The duration of fever of these patients at the time of hospitalization ranged from more than 2 weeks to 4 years in one case.
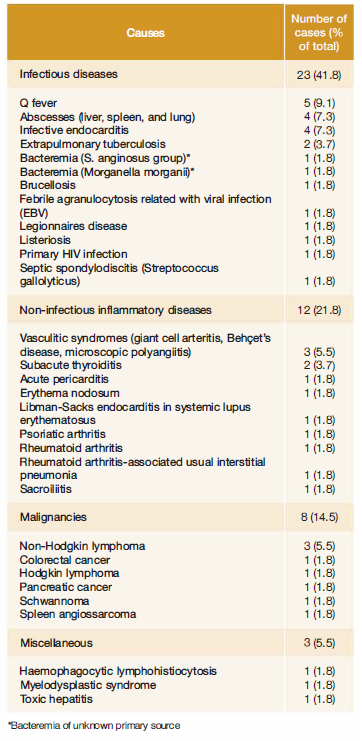
The medium follow-up time used in this study was 12 months. Diagnoses found are listed in Table 2. lnfections were the most frequent cause identified (n = 23; 41 .8%) followed by non-infectious inflammatory diseases (n = 12; 21.8%), malignancies (n = 8; 14.5%) and miscellaneous group (n = 3; 5.5%). However, in 9 cases (16.4%) the diagnosis remained unknown.
ln the older group (:c:65y) infectious diseases remained the principal diagnosis category (n = 10), followed by malignancies (n = 3). NIID was represented by two cases in this age group, one case of temporal arteritis and a rheumatoid arthritis-associated usual interstitial pneumonia. A myelodysplastic syndrome was also diagnosed. There were 4 undiagnosed cases.
ln our study the most common disease causing FUO was Q fever, the infection caused by the bacteria Coxiella bumetii (n = 5; 9.1 %), followed by infective bacterial endocarditis (Enterococcus faecalis, Brucella, Proteus mirabilis and Streptococcus viridans) (n = 4; 7.3%) and abscesses in different locations (n = 4; 7.3%).
During the initial hospitalization three patients died due to complications. The mortality rate during the follow-up was 16.4%.
Among the 9 patients with undiagnosed FUO, none died during follow-up and 5 showed complete recover. There were 4 cases with recurrence of fever in the first 6 months of follow-up. One of them was treated empirically with broad spectrum antibiotics with resolution.
We highlight two cases of fever and polyarthropathy that were described as probable adult-onset Still's disease. Later, after successive episodes of fever recurrence, CNS lymphoma and an autoimmune hepatitis were diagnosed.
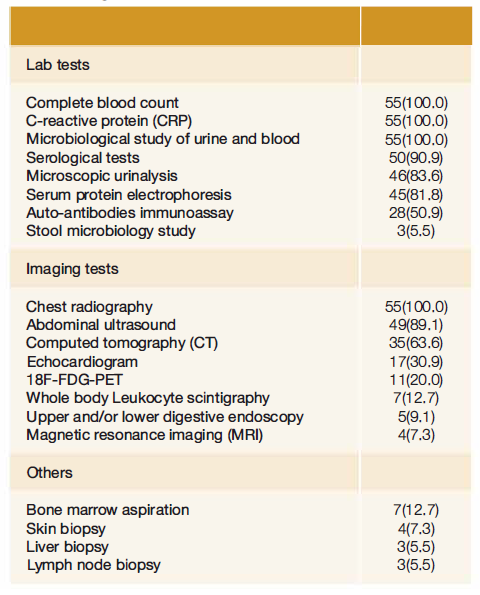
Complete blood count with white blood cell count, routine hematochemical tests with inflammatory markers, including C-reactive protein and/or erythrocyte sedimentation rate were evaluated in all patients (Table 3).
Microscopic urinalysis was evaluated in 46 patients. Microbiological study of urine and blood was performed in all patients, while serological tests showed wider variability.
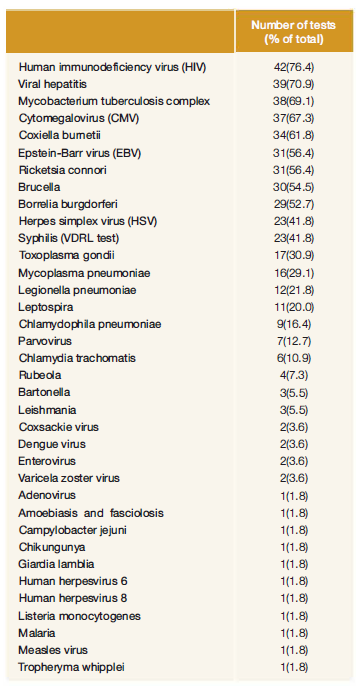
Serological tests have focused more often on HIV (42; 76.4%) and Mycobacterium tuberculosis complex (38; 69.1 %) search through interferon gamma release assay (IGRA). Serological tests were also done for hepatitis (39; 70.9%), cytomegalovirus (CMV) (37; 67.3%), Bruce/la, Ricketsia connori, Borre/ia burgdorferi and Coxiella burnetii. Detailed information can be seen in Table 4.
Auto-antibodies immunoassays were done in 28 (50.9%) cases.
Regarding imaging tests, all patients underwent chest radiography and 49 (89.1 %) abdominal ultrasounds. Other imaging methods were used depending on the clinical case such as computed tomography scan (CT), magnetic resonance imaging (MRI), echocardiogram, and upper and lower digestive endoscopy.
The use of 18F-FDG-PET in 11 (20.0%) cases stands out. Patients performed 18F-FDG-PET in situations where the diagnosis was still unclear. 18F-FDG-PET revealed the presence of an underlying neoplasm in 4 patients; 18F-FDG-PET was not useful in NIID (2 patients), miscellaneous (1 patient), infectious (1 patient) or in undiagnosed situations (3 patients).
ln some cases, biopsies and bone marrow aspiration were performed (n = 17; 30.9%).
Discussion
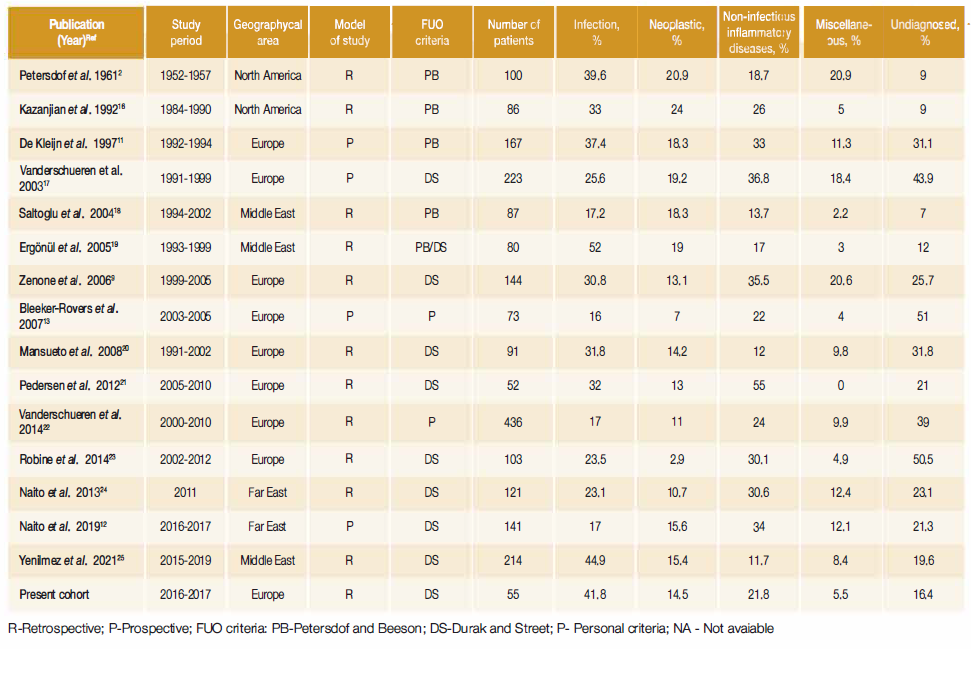
FUO etiologies in our study are comparable to other published studies {Table 5) despite the smaller sample. We found a greater number of infectious diseases and a smaller number of NIID. This finding was not expected if we consider that infectious diseases are more common in developing countries while in developed countries there is a higher prevalence of NIID.4 ln more recent series, infections continued to comprise a significant percentage of FUO cases, and still represent the first cause of FUO globally.5
Although the diagnostic approach can be influenced by several factors, like the incarne of the country, the distribution of diagnostic categories is relatively similar among developed versus developing countries.7,12,14Differences in the definition of FUO used, study design, use of a minimal diagnostic work-up and healthcare systems may be responsible for part of the differences shown in the published studies.
Comparing recent case series with older ones, from 70 years ago, infections and miscellaneous categories are now less common. Simultaneously, the NIID and undiagnosed conditions have risen.5,8A recent systematic review5 showed a change in the distribution of etiologies over time. There were trends toward a higher prevalence of infectious diseases in Southern Asia compareci to Europe.
The most common cause of infection in our study was Q fever. This can be explained based on local epidemiology factors: our population is mostly from rural areas, and they have frequent contact with domestic animais. Q fever is considered an endemic zoonosis in Portugal and is a mandatory notifiable disease. A recent evaluation shows that in Portugal C. Burnetii circulates among several domestic and wild animals.15
Medical evaluation of older adult patients requires a different approach from that used in younger ones.
A low NIID prevalence (21.8%) may be due to an inadequate work-up, consistent with a low nuclear medical imaging, autoimmunity and immunological tests, compareci to serological and microbiological studies. Cognitive bias, i.e., the idea that fever is synonymous of an underlying infection, cannot be excluded.
The number of cases with no diagnosis (16.4%) was comparable to that found in literature in similar studies (Table 5). The risk of having an undiagnosed FUO is higher in Europe.5 ln these cases it was expected that up to 50% will present spontaneous remission and the prognosis is good.4 ln our cohort 44.4% of patients with undiagnosed fever experienced recurrence of symptoms in the first 12 months of follow up and none died in that period.
ln our institution, there is not a standardized protocol for initial assessment of FUO, but a cluster of tests is commonly ordered: complete blood count, CRP, microbiology study of urine and blood, serological tests (including tuberculosis and HIV), chest radiography and abdominal ultrasound. Many papers support the use of a standard initial assessment. Though this can potentially lead to an excessive amount of tests performed it can also increase the diagnostic accuracy.4,6,11,13We emphasize that a good clinical history and physical examination must be carefully done, looking for "potentially diagnostic clues".
Local epidemiological data is also of utmost importance, especially in lab test selection. A random serological test per se has a low diagnostic yield and a fishing strategy should be avoided.4 But the use of serological tests aimed towards endemic and frequent infection is effective. ln our study 18.1 % of the diagnoses were supported in serological tests.
ln Portugal tuberculosis is still a public health issue, despite the significant reduction in the last decade. This explains that an IGRA test was ordered in 69.1 %. This test indicates a cellular immune response to Mycobacterium tuberculosis, but it cannot distinguish between an active or latent infection. ln Mediterranean countries, Middle East, and related geographical area6 infections by Brucella, Leishmania, and Q fever have a higher incidence.26
The knowledge of local epidemiology is also frequently used in empirical antibiotic selection, especially when an infection is suspected, and microbiological and serological tests are still ongoing. ln our cohort, we observed that many cases were treated with tetracyclines (particularly doxycycline) in the first days after hospital admission. The treatment decision was generally based on a suspicious clinical history and aimed to improve clinical outcomes.
The availability of radiopharmaceutical scans can improve the work-up. Particularly 1 SF-FDG-PET can locate the potential cause with greater sensitivity (about 85%)27,28without loss of specificity compared with other nuclear medicine imaging or other anatomic imaging.6,7,11lt has the potential to identify focal inflammatory or infectious processes, and so it is especially useful for localizing areas for further evaluation.29 ln our sample, an 1 SF-FDG-PET scan was conclusive in 36.4% of the cases, where it supported a diagnosis of malignancy. Though it failed to provide or point to a probable diagnosis in the remaining, no neoplasm was misdiagnosed.
This study has several limitations: the number of FUO cases is small which can have under represented some etiologies. FUO cases were identified based on the information described in the discharge letter, some of whom did not had a well-defined period of symptoms; it is possible that some FUO cases were missed. lt included only patients admitted to the Internai Medicine Department; patients admitted to other departments (e.g., lnfectious Diseases, Rheumatology) or followed as outpatients may yield different causes.
We would like to underline some of the strengths of this study: we found that FUO is more common than we expected (0.6% of all admissions), and that the FUO clinical algorithm is useful and should be applied in every situation where the etiology of the fever is not obvious. As far as the authors know, this is the first study on Portuguese patients and it helps to describe local epidemiology. AII the patients were admitted to hospital so this study improves the knowledge about the more complex conditions and more severely ill patients.
Conclusion
FUO is still a challenging problem, being responsible for 0.6% of all admissions in our department. lnfections were the most frequent cause, particularly 0 fever. Despite extensive work up a large number of cases remained undiagnosed (16.4%). FUO aetiologies found in our study are comparable to other cohorts published.
We consider that the medical history and physical examination are crucial to approach FUO patients. An initial basic standardized laboratory and imaging study can be useful but it should be directed based on clinical features, organ involvement and local disease prevalence to avoid excessive initial testing. We think that the increase of imaging tests at disposal, of which 1 SF-FDG-PET /CT stands out, and new laboratory methods will contribute to the reduction of undiagnosed cases.
We hope this article helps to fulfil the gap in the Portuguese medical literature on this topic, its prevalence, causes and diagnostic approach. The diagnostic spectrum of FUO is changing over time. Constant re-evaluation of clinical data is essential considering the dynamic change in disease patterns.