Introduction
Vitamin D (VD) deficiency is a major health problem, present in around 30%-50% of world population.1 Heart failure (HF) remains a relevant public health disease due to its high prevalence and its major impact on elderly population hospitalizations.2 There is a frequent association between VD deficiency and HF disease, related in 80% to 95% of the cases.3 VD deficiency has been strongly associated to an increased risk of developing HF, also to worst HF-related outcomes and higher risk of HF hospitalization (hHF) consequently to death in these patients.1,2,4-6It has also been correlated with greater incidence of depression and cognitive dysfunction in HF population.5,7
VD is associated to specific anti-inflammatory effects by suppressing the release of inflammatory factors like tumor necrosis factor and increasing serum concentrations of anti-inflammatory cytokines such as interleukin 10 in HF patients. Nevertheless, trials of VD supplementation have shown inconclusive results and this practice is not currently recommended, neither to reduce the risk of heart failure, nor to improve HF-related outcomes.1,3,6,8-10However, the myocardium is considered to be an important target of 25 (OH)D and 1.25 (OH)2D and VD status could influence left ventricle LV structure and function.11,12
These inconclusive data encouraged us to conduct a study on the impact of vitamin D supplementation in heart failure patients with VD deficiency.
The present study aims to evaluate clinical, analytical and functional impact of the VD deficiency in a cohort of HF patients followed-up in a heart failure clinic.
Methods
In this observational retrospective single-center study, we included all patients admitted to our HF clinic from January 2015 to December 2018 with VD deficiency (< 50 nmol/L) at admission. Patients with stage 5 of chronic kid-ney disease by the National Kidney Foundation (NKF) classification, those with incomplete follow-up and those who were previously under VD treatment were excluded.
All patients were enrolled in an outpatient setting and received a prescription of oral cholecalciferol. Data concerning dosage or adherence to treatment were retrieved from electronic medical records. Serum VD (25-OH-vitamin D) level was checked after one-year supplementation and study population was grouped within two groups: VD deficiency corrected [VD (+) group] and VD deficiency maintained [VD (-) group]. A descriptive analysis was carried out to characterize baseline profile of each group. Functional variables and vital outcomes were compared in both groups, before and after cholecalciferol therapy, in order to evaluate the impact of VD deficiency correction: New York Heart Association (NYHA) functional class as a subjective scale of symptoms; N-terminal-pro hormone B-type natriuretic peptide (NT-pro-BNP) as a prognostic serum biomarker; Duke Activity Status Index (DASI) as a self-administered questionnaire that assesses the functional capacity of patients with cardiovascular disease, and Six-Minute Walk Test Distance (6MWD) as an objective measure of functional capacity. We also evaluated hHF and mortality during one year after treatment.
All data were collected from electronic medical records. Descriptive and statistical analysis was performed using IBM SPSS Statistics, version 27.0, IBM Corp, Armonk, NY. Cate-gorical variables are presented as number of cases and percentage. Continuous variables are presented as mean and standard deviation from the mean or median and interquartile ranges as appropriate. One-sample Kolmogorov-Smirnov test, Shapiro-Wilk test, analysis of kurtosis, skewness and normal Q-Q plots were used to access normality of distribution within groups of study. Categorical variables were compared using Fisher’s exact test or chi-square test, as appropriate. For continuous variables, we used Mann-Whi-tney U or t-test for independent samples to compare the initial characteristics between the two groups, and a repeated measures analysis (ANOVA), Wilcoxon signed ranks test or paired t-test as appropriate to compare the evolution of continuous variables within and between groups. All reported p-values are two-tailed and statistical significance was considered if p values were <0.05.
Results
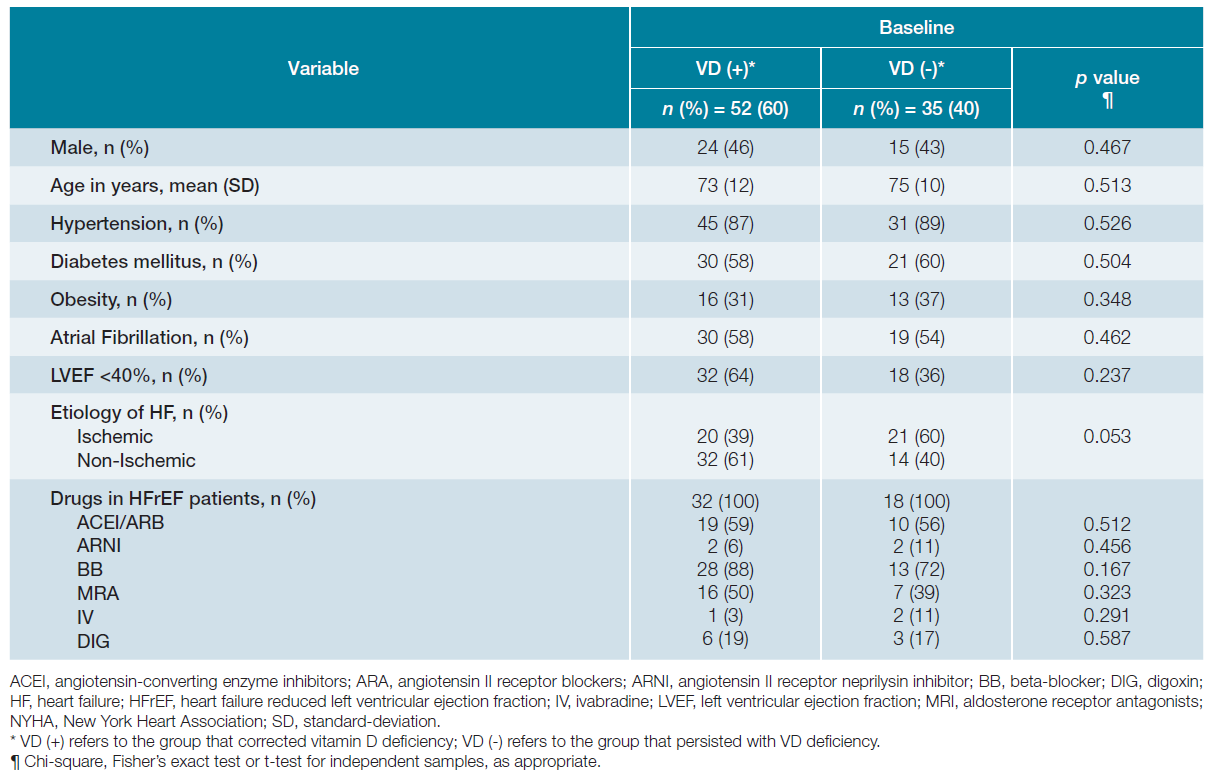
From a total of 239 patients admitted to our HF clinic from January 2015 to December 2018 with VD deficiency, 152 were mostly excluded due to incomplete follow-up (dischar-ge of HF clinic or absence of reevaluation of VD level at 12 months) as shown in Fig. 1. The remaining 87 patients defi-ned the study population. After approximately one-year of oral VD supplementation there were 52 (60%) patients with normal VD level [VD (+) group] and 35 (40%) patients that maintained VD deficiency [VD (-) group]. The baseline characteristics of both groups are depicted in Table 1 and were not statistically different regarding all the variables analysed. This was predominantly an elderly and female population, with a mean age of 74 years-old and with high prevalence of comorbidities such hypertension, diabetes mellitus and atrial fibrillation. In the VD (+) group, the major HF etiology was non-ischemic with reduced (< 40%) left ventricle ejection fraction (LVEF) and in VD (-) group was predominantly ischemic with non-reduced LVEF. Regarding HF medications, in the VD (+) group and VD (-) group respectively, 65% and 67% of patients with reduced LVEF were taking angiotensin-converting enzyme inhibitors/ angiotensin II receptor blockers/angiotensin II receptor neprilysin inhibitor and 88% and 72% were taking beta-blockers.
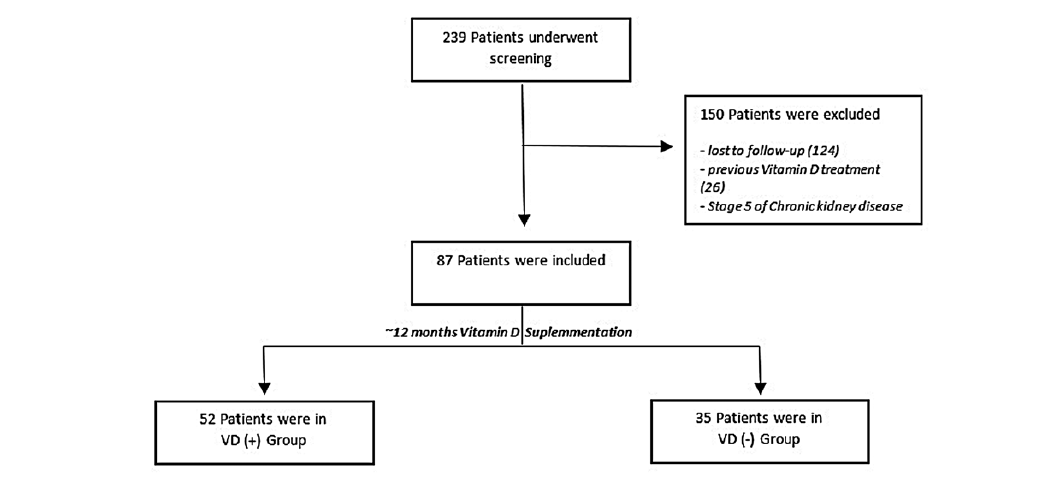
Figure 1: Study enrollment and follow-up. VD (+) group: patients whose vitamin D deficiency has been corrected; VD (-) group: patients whose vitamin D deficiency maintained after supplementation
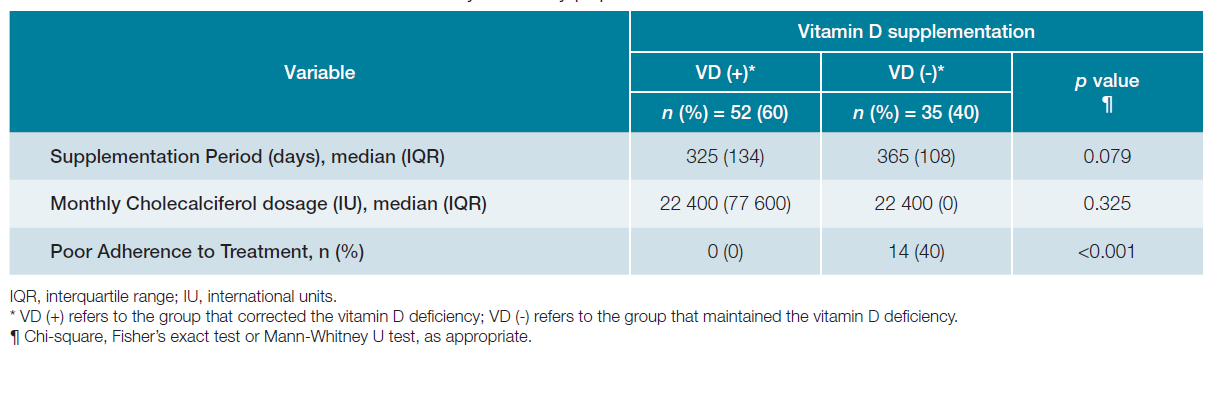
As shown in Table 2, the supplementation period (median of 12 months) as well as VD monthly intake were similar in both groups (median of 22 400 International Units). According to clinical records, VD (-) group had poor compliance. Exclusion of the non-compliant patients of VD (-) group did not alter the following results (data not shown).
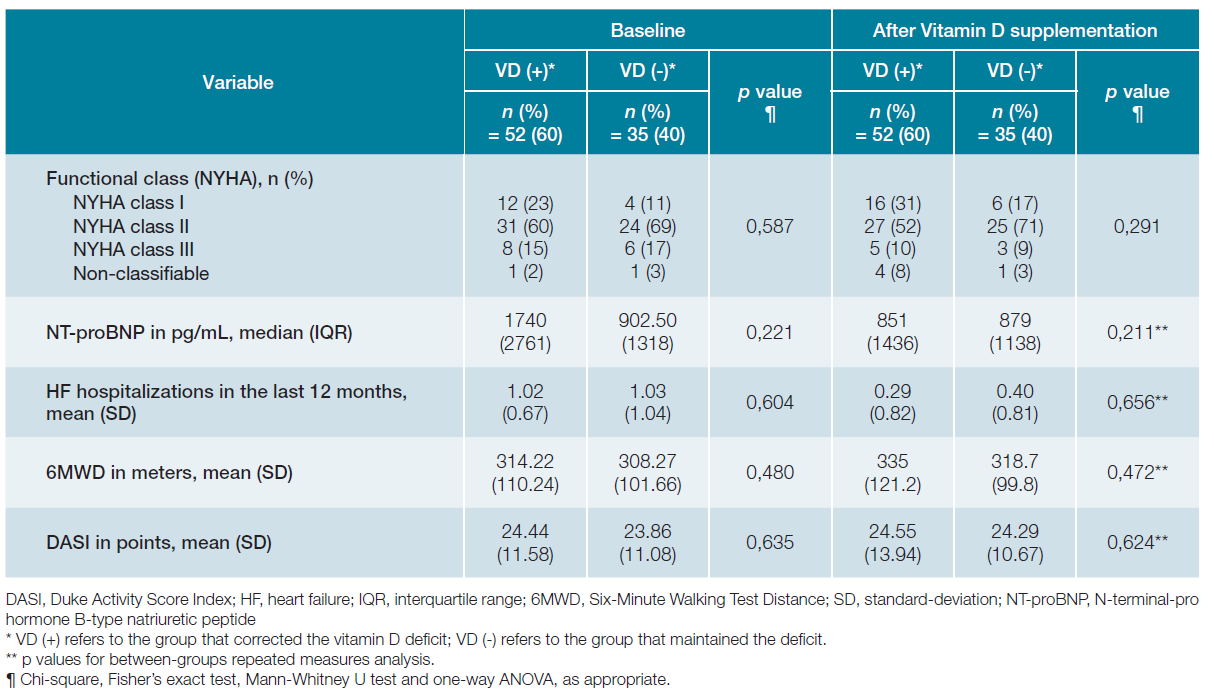
Comparison of clinical variables between the two study groups before and after VD supplementation are exhibited in Table 3. Before VD supplementation, both groups were similar in terms of NYHA class, NT-proBNP, DASI and 6MWD. There was also no difference in number of hHF in the 12-month period before enrollment.
There was a higher number of patients in NYHA class I after 12-month follow-up in both groups, but the difference between groups was not statistically significant (p = 0.291) - Table 3.
As seen in Fig. 2, after one-year of VD supplementation, both groups showed a decrease in median levels of NT-proB-NP with VD treatment; (VD (+) group: 1740 ± 2761 pg/mL to 851 ± 1436 pg/mL, p = 0.001 vs VD (-) group: 902 ± 1318 pg/mL to 879 ± 1138 pg/mL, p = 0.272). The slope was steeper and had statistical significance in VD (+) population but not be-tween groups (p=0.221), as depicted in Table 3.
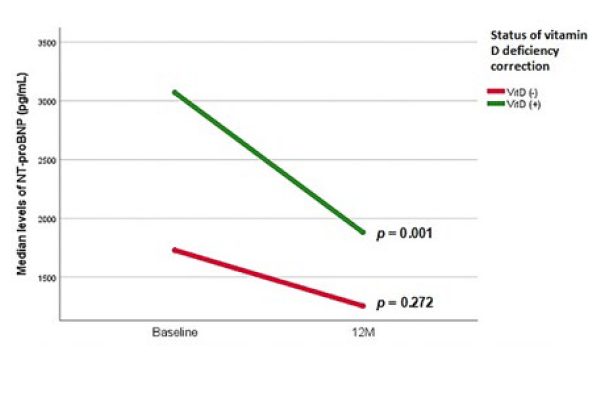
Figure 2: Evolution of median NT-proBNP levels in pg/mL before and after vitamin D supplementation therapy for both groups.
Additionally, there was a statistically significant reduction in the mean number of hHF within both groups; (VD (+) group: 1.02 ± 0.67 to 0.29 ± 0.82, p< 0.001) vs VD (-) group: 1.03 ± 1.04 to 0.40 ± 0.81, p = 0.001) - Fig. 3 - but not between groups (p= 0.656) - Table 3.
There was an improvement of 6MWD in the 2 groups; (VD (+): 314.22 ± 110.24 m to 335.00 ± 121.20 m, p = 0.397 vs VD (-): 308.27 ± 101.66 m to 318.70 ± 99.80 m, p=0.076) but with no statistical significance, neither within nor between groups - Fig. 4 and Table 3. Several patients were not able to perform the test: 8 patients in VD (+) group and 5 patients in VD (-) group.
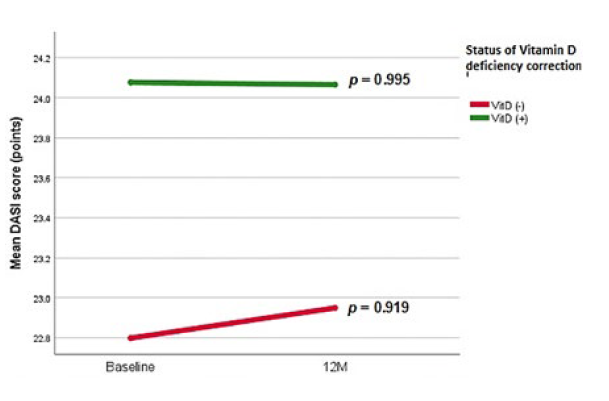
Regarding DASI evolution, we report a slight increase within both groups; (VD (+): 24.44 ± 11.58 points to 24.55 ± 13.94 points, p = 0.995 vs VD (-): 23.86 ± 11.08 points to 24.29 ± 10.67 points, p = 0.919), greater in VD (-) population, that was independent of VD deficiency correction status - Fig. 5 and Table 3.
There were no deaths in either group during the follow-up period.
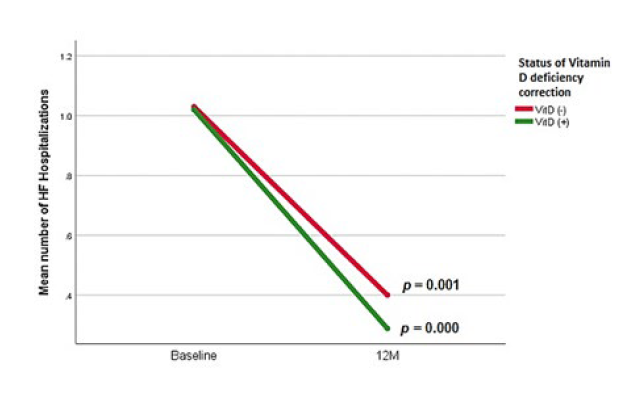
Figure 3: Evolution of mean number of hospitalizations before and after vitamin D supplementation therapy for both groups.
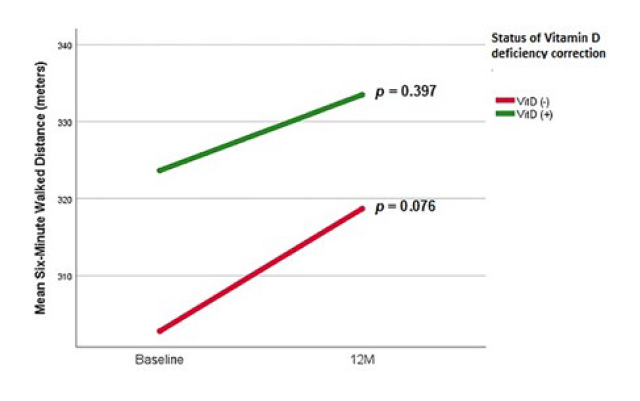
Figure 4: Evolution of mean distance (in meters) walked on Six-Minute Walking Test Distance; before and after vitamin D supplementation therapy for both groups.
Discussion
This study reports one-year outcomes of a HF patients’ co-hort with VD deficiency treated with VD, and it shows that the correction of VD deficiency did not correlate statistically with improvements in functional capacity measured by NYHA class, DASI score or 6MWD neither with reduction of NT-proBNP level or number of hHF.
NYHA classification is a simple and widely-used tool to stratify dyspnea and its impact on daily activities of HF patients, being considered an unreliable predictor of outcome.13 We found more patients on class I NYHA in both groups at the 12-month evaluation after VD supplementation, which can be considered as an improvement symptom in this population. Patients who corrected VD deficiency showed a statistically significant decrease of NT-proBNP levels over time, within group effect, that was not seen in patients who did not correct VD deficiency. This result is clinically significant since NT-proB-NP is a strong prognostic factor with higher values predicting higher risk of death and hospital readmissions.14-16Although, as no difference was seen between groups after one year of VD treatment, the greater decrease of NT-proBNP levels is probably a consequence of others interventions, possibly to a better adherence to drug treatments and non-pharmacological interventions of the VD (+) group of patients.
Vitamin D deficiency has been shown that correlates with an increased risk of hHF in various studies and, independently, with higher overall mortality, but some randomized studies failed to show an impact of VD supplementation on mortality of HF patients.1,3,5,6,10,17-19One of these studies is the EVITA study17 that evaluated a very distinct HF population, mainly male, two decades younger than those of the present study and with reduced LVEF, waiting for heart transplantation. Notwithstanding, the significant reduction in hHF over time that we found in both groups, could reflect the impact of the multidisciplinary care in preventing such events, since we did not find any correlation between hHF and normalization of VD levels and research shows that interventions with VD did not reduce the first hospitalization rate in heart failure.20
DASI has been validated as a functional tool with prognos-tic implication in stable HF patients.19,21Likewise, 6MWD has been considered a highly reliable and independent predictor of hospitalization and mortality in chronic HF patients.22,23We found no impact of VD deficiency correction in these functional tests. The 6MWD results could have been influenced by the fact of several patients not being able to perform the test. However, the change in 6MWD between baseline and 12 mon-ths after VD supplementation was the primary endpoint of the VINDICATE study, which was also neutral.11
Overall, we found a functional and clinical improvement in both groups over time that may be due to a regular follow-up in a multidisciplinary HF clinic and the consequent optimization of HF care. The effect of VD supplementation in hHF, 6MWD and NT-proBNP was neutral, in line with the overall results of the previous studies.11,24Although the association between VD deficiency and poor outcome seems real, the supplementation did not seem to have impact in the usual outcomes of the HF trials, supported by study that demonstrated that VD supplementation of VD-sufficient subjects does not provide any benefit in terms of cardiovascular health in general population.25 Probably, the VD deficiency in HF patients reflects advanced disease and poor overall health status that do not change by correcting VD levels.12,24
Ejection fraction (EF) after treatment was not evaluated in this study, which could be an overall relevant data, since study results indicate that prescribing VD for patients with HF, especially in LVEF < 50%, enhances myocardial EF.26
This study has limitations. First, the retrospective nature and consequent difficulty to control adherence to VD treatment. Second, the exclusion of a relevant number of non-followed-up patients which reduced considerably the number of study patients. In spite of these, we expect to highlight an underexplored topic and to trigger future randomized prospective studies with larger populations in order to achieve more conclusive results.
Conclusion
The correction of VD deficiency in this population of HF patients did not have impact in NYHA class, NT-proBNP levels, hHF, DASI score or 6MWD. The improvements reported within both groups may reflect the impact of a HF clinic optimized care. Randomized prospective studies with larger populations are needed in order to achieve more conclusive results.