Imaging Cases
Caso clínico imagiológico
1. Department of Pediatrics, Hospital de Braga. 4710-243 Braga, Portugal. affmorais@gmail.com; a.luisacarvalho@live.com.pt; margaridareismorais@sapo.pt
2. Department of Pediatric Surgery, Hospital de Braga. 4710-243 Braga, Portugal. catabarroso@gmail.com
3. Pediatric Intermediate Care Unit, Hospital de Braga. 4710-243 Braga, Portugal. mariapitxitxica@hotmail.com; verabaptista1@sapo.pt; liliana.abreu@gmail.com
Abstract
Congenital diaphragmatic hernia (CDH) results from incomplete closure of the pleuroperitoneal canal during fetal development, allowing herniation of abdominal contents into the thoracic cavity. It usually presents in the neonatal period with respiratory distress, but can also manifest later in life.
The diagnosis of late-onset CDH should be kept in mind in the differential diagnosis of children with acute or recurrent nonspecific symptoms, especially respiratory or gastrointestinal symptoms or both. Clinical suspicion and plain radiography remain the key to diagnosis. Early surgical correction of the diaphragmatic defect is crucial to prevent possible passage or strangulation of abdominal viscera and severe respiratory problems.
In the present report, the authors present a typical case of late-onset CDH with acute presentation of gastrointestinal symptoms (e.g., abdominal pain and vomiting). Thoracoscopic repair was performed, with reduction of the abdominal contents (small bowel and colon) and suturing of the posterior diaphragmatic defect.
Keywords: abdominal pain; children; congenital diaphragmatic hernia; late-presentation
Resumo
A hérnia diafragmática congénita (HDC) resulta do encerramento incompleto do canal pleuroperitoneal durante o desenvolvimento fetal, permitindo a herniação do conteúdo abdominal para a cavidade torácica. Apresenta-se tipicamente durante o período neonatal sob a forma de dificuldade respiratória, podendo no entanto manifestar-se mais tarde na vida.
O diagnóstico de HDC tardia deve ser considerado no diagnóstico diferencial de crianças com sintomas agudos ou recorrentes inespecíficos, principalmente respiratórios ou gastrointestinais, ou ambos. A clínica e a radiografia simples continuam a ser os elementos-chave para o diagnóstico. A correção cirúrgica precoce do defeito diafragmático é crucial para prevenir uma possível passagem ou estrangulamento das vísceras abdominais e problemas respiratórios graves.
Neste artigo, os autores apresentam o caso de uma HDC de apresentação tardia, caracterizada pelo início agudo de sintomas gastrointestinais, como dor abdominal e vómitos. Foi realizada correção toracoscópica com redução do conteúdo abdominal (intestino delgado e cólon) e sutura do defeito diafragmático posterior.
Palavras-chave: apresentação tardia; criança; dor abdominal; hérnia diafragmática congénita
A previously healthy three-year-old girl presented to the Emergency Department with acute severe abdominal pain refractory to oral analgesia and persistent vomiting with one hour of evolution. She also had anorexia and reported no bowel movements for the past two days.
No fever, dyspnea, or other relevant symptoms were reported.
On admission, the girl complained of persistent severe pain and was agitated and pale. Vitals were stable. On physical examination, she had no signs of respiratory distress. Vesicular breath sounds were decreased on the left inferior pulmonary field, the abdomen was flat, and there was no pain on palpation.
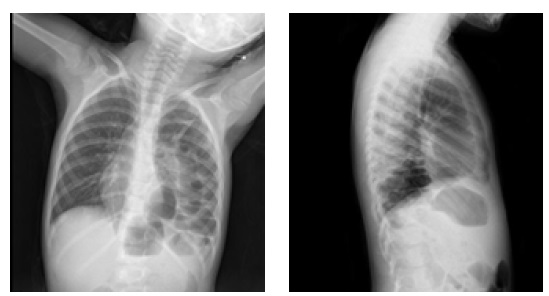
Laboratory studies, including complete blood count, chemistry panel, and urinalysis, were normal. Abdominal and thoracic radiographs were performed (Figures 1a and b). Abdominal ultrasound showed no abnormalities.
What is your diagnosis?
Diagnosis
Left posterolateral congenital diaphragmatic hernia
Discussion
Congenital diaphragmatic hernia (CDH) results from incomplete closure of the pleuroperitoneal canal during fetal development, allowing herniation of abdominal contents into the thoracic cavity.1 The condition has a prevalence of 1 in 3000-5000 children. Currently, CDH is diagnosed prenatally by ultrasound and only a minority of small and mostly right-sided hernias are missed.2,3)
CDH usually presents in the neonatal period with respiratory distress, but in 5-25% of cases it manifests later in life. The wide clinical spectrum of late-onset CDH seems to be influenced by the timing of the intrathoracic herniation and the type of displaced viscera.4,5 Failure to thrive is the most common manifestation, with gastrointestinal and respiratory symptoms, or a mixture of both, potentially also present. In some cases, the diagnosis is made incidentally through analysis of radiographic images obtained for other reasons.
The left hemithorax is the most commonly affected side and often determines a more acute presentation in older children where abdominal symptoms predominate. Presentation on the right side is more common in younger patients and typically has an insidious pattern in which respiratory symptoms predominate. The most important factor responsible for chronic or acute presentation seems to be related to the type of herniated viscera.4
Early surgical correction of the diaphragmatic defect is crucial to prevent possible passage or strangulation of abdominal viscera and severe respiratory problems.6
This case represents a typical late-onset CDH with acute onset of gastrointestinal symptoms including abdominal pain and vomiting.
The patient underwent thoracoscopic repair, with reduction of the abdominal contents (small bowel and colon) and suturing of the posterior diaphragmatic defect. No intraoperative complications occurred. Postoperative care was uneventful, and the child was discharged home three days later.
She currently remains on outpatient pediatric surgery follow-up, without any symptoms or imagiological recurrence of the hernia.
The overall prognosis of late-onset CDH is better than that of CDH diagnosed prenatally or in the early postnatal period. There is a lower risk of pulmonary hypoplasia and pulmonary hypertension and an also a lower association with malformations.7 However, misdiagnosis is much more common in late-presenting CDH and may result in increased morbidity and mortality.6
In summary, the diagnosis of late-onset CDH should be kept in mind in the differential diagnosis of children with acute or recurrent non-specific symptoms, namely respiratory or gastrointestinal symptoms or both. Clinical suspicion and plain radiography remain key to diagnosis. Early accurate diagnosis and timely surgical repair are crucial to prevent life-threatening complications.7
Authorship
André Morais - Conceptualization; Investigation; Writting - original draft; Writing review & editing
Ana Luísa Carvalho - Conceptualization; Investigation; Writting - original draft; Writing review & editing
Catarina Barroso - Conceptualization; Investigation; Writting - original draft; Writing review & editing
Maria João Magalhães - Writing review & editing
Vera Baptista - Writing review & editing
Liliana Abreu - Writing review & editing
Margarida Reis Morais - Writing review & editing
References
1. Tovar JA. Congenital diaphragmatic hernia. Orphanet J Rare Dis. 2012;7:1.
[ Links ]
2. Karmazyn B, Shold AJ, Delaney LR, Brown BP, Marine MB, Jennings SG, et al. Ultrasound evaluation of right diaphragmatic eventration and hernia. Pediatr Radiol 49, 1010-1017 (2019). Doi: https://doi.org/10.1007/s00247-019-04417-1.
[ Links ]
3. Badillo A, Gingalewski C. Congenital diaphragmatic hernia: treatment and outcomes. Semin Perinatol. 2014 Mar;38(2):92-6. doi: https://doi.org/10.1053/j.semperi.2013.11.005.
[ Links ]
4. Baglaj M. Late-presenting congenital diaphragmatic hernia in children: a clinical spectrum. Pediatr Surg Int. 2004;20(9):658-69.
[ Links ]
5. Kim DJ, Chung JH. Late-presenting congenital diaphragmatic hernia in children: the experience of single institution in Korea. Yonsei Med J. 2013;54(5):1143-1148. doi: https://doi.org/10.3349/ymj.2013.54.5.1143.
[ Links ]
6. Cigdem MK, Onen A, Otcu S, Okur H. Late presentation of bochdalek-type congenital diaphragmatic hernia in children: a 23-year experience at a single center. Surg Today. 2007;37(8):642-5.
[ Links ]
7. Rygl M, Pycha K, Stranak Z, Melichar J, Krofta L, Tomasek L, et al. Congenital diaphragmatic hernia: onset of respiratory distress and size of the defect. Pediatr Surg Int. 2007;23(1):27-31. doi: https://doi.org/10.1007/s00383-006-1788-3.
[ Links ]