Introduction
Scalp swelling is a common clinical condition in the neonatal period and in young infants. It can be caused by cephalohematoma, caput succedaneum, subgaleal hemorrhage, and delayed subaponeurotic or subgaleal fluid collection (DSFC).1
The scalp is divided into five layers: skin, subcutaneous tissue, galea aponeurosis, loose connective tissue, and periosteum.1,2,10,12,14) DSFC is defined as fluid accumulation between the galea aponeurosis and the periosteum and typically manifests beyond the neonatal period.2,3,12,14) It is a recently described entity with fewer than 50 cases reported in the literature. The first cases were described in 2002 in a case series by Hopkins et al.1)
DSFC is usually described as a soft, ill-defined, mobile, fluctuant, non-tender swelling that crosses the cranial suture lines and is located over the superior occiput.3,4,12,14 It usually develops by one to four months of age in healthy and hemodynamically stable infants with no history of recent trauma.3,4,11,12) The exact etiology is unknown, but birth trauma, instrumental delivery, or scalp electrodes leading to disruption of venous drainage, lymphatic drainage, and/or cerebrospinal fluid (CSF) leakage have been implicated as major mechanisms.2,3,10
Other conditions should be considered in the differential diagnosis of DSFC, such as non-accidental injuries, coagulopathies, and other causes of neonatal scalp swelling (cephalhematoma, caput succedaneum, subgaleal hematoma).10
DSFC is a benign condition with a clinical diagnosis. Management is conservative, with spontaneous resolution expected in one to two months.3,4,10
The authors present the first case of DSFC reported in a Portuguese child, with the aim of improving its diagnosis and management, and also present a brief review of the literature on the subject.
Case report
A seven-week-old male infant was brought to the pediatric Emergency Department with an acute onset of occipitoparietal scalp swelling with five hours of evolution. The swelling was noticed by the parents, who reported that the boy was eating, behaving, and sleeping normally and had no abnormal movements, vomiting, or infectious symptoms. There was no history of trauma or scalp manipulation and no relevant family history (e.g., coagulopathy).
The boy was born at 37 weeks’ gestation by cesarean section after induced labor for fetal growth restriction and failure to progress. No fetal scalp electrodes or instruments were used during labor. No scalp swelling was noted in the scalp in the immediate neonatal period. Medical history was otherwise unremarkable.
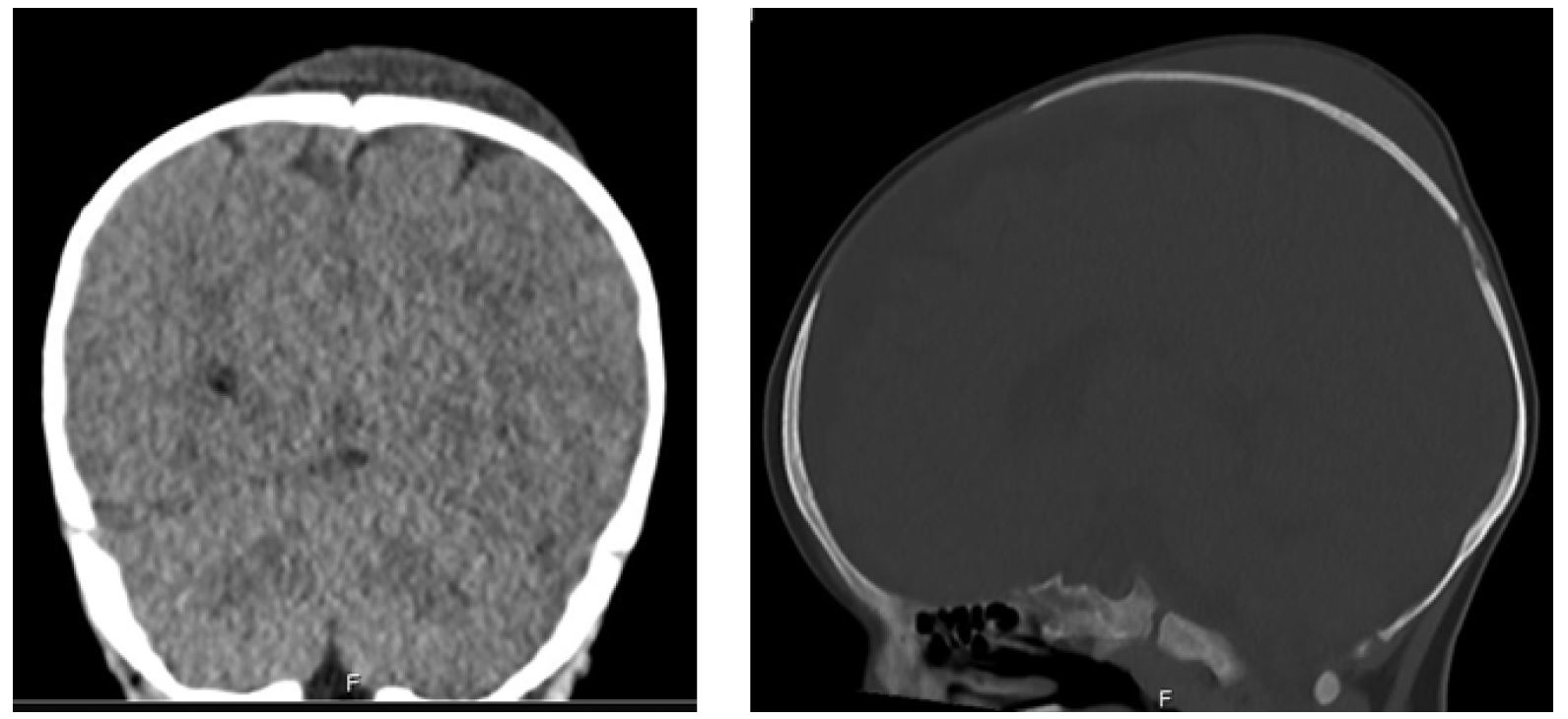
At presentation, the patient was alert and interactive with stable vital signs. Physical examination revealed a large scalp swelling in the occipitoparietal area that was ill-defined, fluctuant, watery in consistency, and not bounded by suture lines (Figure 1). It was non-tender with no overlying skin changes. The systematic examination was normal, including normal anterior fontanelle and normal neurological examination. There was no evidence of physical injury or trauma.
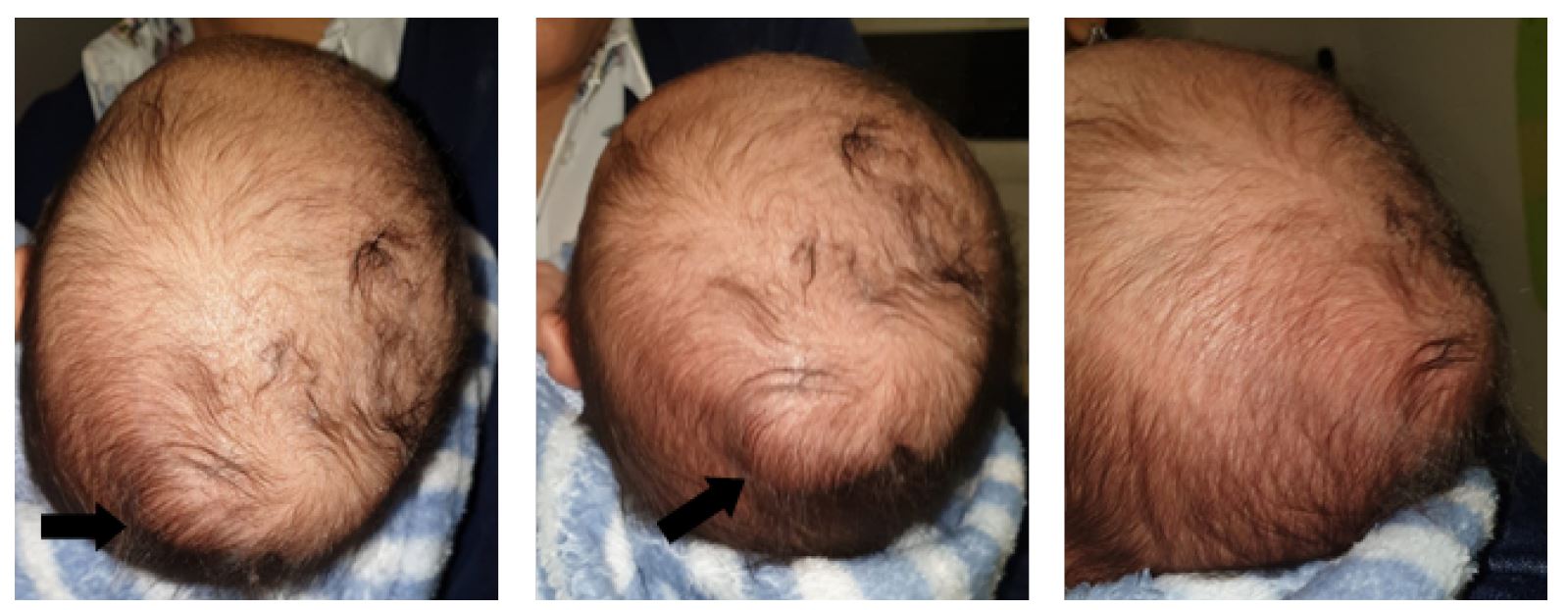
Figure 1 Fluid scalp swelling in the occipitoparietal region without evidence of overlying scalp erythema or injury. The collection does not follow the cranial suture lines
Blood tests, including coagulation, were normal. Cranial ultrasound (US) revealed a compressible, hypoechoic subgaleal fluid collection approximately 7 mm across the suture lines. A non-contrast cranial computed tomography (CT) scan confirmed these findings and revealed no skull fracture or intracranial abnormality (Figure 2).
The patient’s history, physical examination, and imaging findings were consistent with the diagnosis of benign delayed subaponeurotic fluid collection (DSFC), which was confirmed by the pediatric neurosurgeon. Conservative management was decided, and the child was discharged home after 14 hours of surveillance in the hospital.
At the first follow-up five days later, blood tests were unchanged. Cranial US showed the same fluid collection, now with approximately 11 mm. Fifteen weeks later, a control cranial CT was performed and showed a decrease in the subaponeurotic fluid collection. At the next visit, growth and developmental milestones were normal and the scalp swelling continued to decrease in size, resolving completely within 19 weeks of onset.
Discussion
DSFC is a rare disorder with no clear etiology.3,5,10,11 It is characterized by the spontaneous development of a head swelling in early infancy in a healthy patient.4,11 The literature identifies the typical age of onset at one to four months.2-4,6,11,12 DSFC is described as a soft, ill-defined, mobile, and non-tender swelling that crosses the skull sutures lines.3,4,6,10,12,13 Infants are well-appearing. The scalp area overlying DSFC has a normal appearance, without warmth, erythema, tenderness, or signs of trauma.3,4,12) It is typically located over the superior occiput.4
The unexplained development of scalp swelling in infancy may raise suspicion of non-accidental injury or coagulopathy.3,8 Although no published case has been linked to acute or non-accidental injury or other conditions, these causes should not be forgotten.3,4,10,11,12
The exact etiology of DSFC remains unknown.3,6,9,11,12),U14) However, prolonged or traumatic labor, instrumented delivery, or fetal scalp electrode monitoring have been identified as common features in affected infants.3,5-8,11,12,14 In fact, most DSFC cases have a history of instrumented delivery or emergency cesarean section (mostly due to failure to progress).
Schoberer et al. reported that β2-transferrin and β-trace protein, which are specific markers of CSF, were found in the aspirated fluid of three affected infants.9 Etiologic hypotheses generated from these findings suggest delayed CSF leakage into the subaponeurotic space through skull microfractures caused by traumatic birth or fetal scalp electrodes not detectable by imaging.3,4,6,7,9-12,14 Another hypothesis is disruption of the emissary veins connecting the intracranial venous sinuses to the superficial scalp veins or disruption of scalp lymphatic drainage within the subaponeurotic connective tissue layer during traumatic labor.3,5,7,9-12
Traumatic delivery can cause three different types of scalp swelling in newborns: caput succedaneum, cephalohematoma, and subgaleal hematoma.2,12 Scalp swelling is common in newborns, but uncommon after the perinatal period.2,5,13
Caput succedaneum is caused by fluid extravasation within the subcutaneous layer of the scalp due to excessive pressure on tissues in the presenting part of the fetal head during delivery.5,10,12 The edematous tissue in patients with caput may extend across the suture lines and resolve over hours to days after delivery.5,10,12,14 Cephalohematoma refers to bleeding in the subperiosteal space associated with traumatic birth and is easily distinguished from DSFC because it does not cross the suture lines.3-5,10,12,14 These two types of scalp swelling occur in the immediate neonatal period, whereas DSFC has a delayed onset, occurring weeks to months after birth.3,5,10,12 Finally, subgaleal hemorrhage is caused by bleeding into the same anatomic space as DSFC, crosses the suture lines, and may have a similar fluctuant, boggy mass on physical examination.4,5,10,12,14) Blood from a subgaleal hemorrhage may travel down the head or neck, producing the Battle sign, whereas DSFC tends to remain localized at the top of the head or occiput.5,10,12 The subaponeurotic layer between the aponeurosis and connective tissue is highly vascular, increasing the risk of massive bleeding in this large space, which can lead to life-threatening hypovolemic shock in young infants.1,3-5,10,12,13 Although most subgaleal hemorrhages develop in the immediate neonatal period in association with birth trauma, they may also occur in older infants after head injury, sometimes in association with coagulopathy, vascular abnormalities, or non-accidental trauma (shaken baby syndrome), and may present acutely with hemorrhagic shock.3,5,10,12-14 Conversely, infants with DSFC are usually well-appearing and do not experience adverse impact on their health, feeding, or behavior.10,12
The diagnosis of DSFC is primarily clinical, based on history and physical examination.3-5,7,12) The classic presentation is a well-appearing infant with an acute, large, soft, fluctuant subcranial fluid collection that freely crosses suture lines, without report or evidence of associated head injury, and with a history of difficult or instrumented delivery.12 Laboratory tests or head imaging study (US, CT scan, or magnetic resonance imaging [MRI] scan) may be considered in the differential diagnosis to confirm the anatomic location of the fluid collection and screen for skull fracture or associated intracranial injury.3-5,7,8,10,12,14) Aspiration and analysis of fluid contents are not recommended and may lead to infection or injury.1,6-8,10,12 Usually, cranial US shows a mobile and hypoechoic fluid collection within the subgaleal space that crosses suture lines, and CT or MRI do not reveal skull fracture or intracranial pathology.4,8,11-13 If trauma, child abuse, or coagulopathy disorders are of concern, further assessment should be performed.3,10,13
The literature unanimously recommends a conservative approach to DSFC, as it usually resolves spontaneously within two weeks to five months of diagnosis without sequelae or recurrence.2-4,6,7,11,12 Lesion drainage has invariably resulted in fluid re-accumulation.5,6,8,10,11,14)
Follow-up consists of assessment of clinical evolution and should be performed by primary care providers.8,12)
In conclusion, the authors presented a case of DSFC, a rare condition in which the clinical history, scalp swelling, and delivery outcome were similar to the few cases described in the literature. Spontaneous resolution was achieved with conservative management.
DSFC should always be considered in the differential diagnosis of scalp swelling in infants. The increasing awareness of this benign and rare entity will help physicians (pediatricians, emergency room physicians, and neurosurgeons) and parents in the diagnosis and management of the condition.