A nine-year-old girl presented to the Emergency Department with a 1-month history of limping and thigh pain that had recently worsened. There was no history of trauma or recent infections. The girl had a past medical history of obesity and subclinical hypothyroidism.
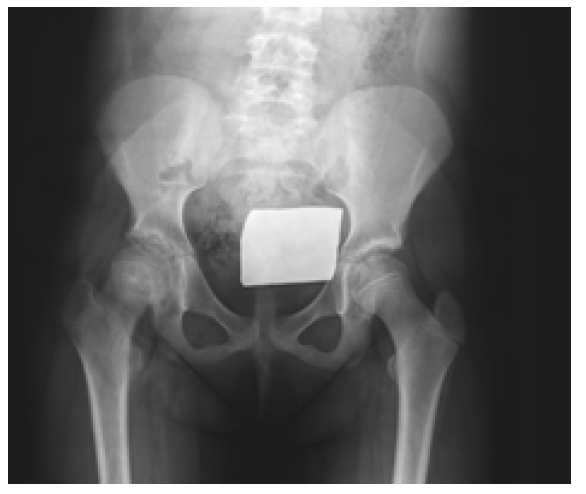
On objective examination, no fever or other systemic signs of infection were observed. The girl had increasing pain with right hip rotation and flection, and therefore bilateral hip radiographs with anteroposterior and lateral frog-leg views were performed (Figures 1and2).
Discussion
Slipped capital femoral epiphysis (SCFE) is a condition of the proximal femoral physis that results in a slippage of the epiphysis relative to the metaphysis.1,2 It is also called slipped upper femoral epiphysis (SUFE) and is the most common hip disorder in preadolescents and adolescents (between 8 and 15 years of age).1-3 However, it is not commonly observed in routine clinical practice and the diagnosis can be challenging in early stages of disease.1,4
The incidence of SCFE is approximately 10/100,000, ranging from 0,33/100,000 to 24,8/100,000 depending on sex and ethnicity.1,2
The single most significant risk factor for SCFE is obesity (present in 51-77% of cases). Other risk factors include male sex, periods of rapid growth, and prior radiation therapy.5 The average age of onset is 11,2 years in females and 12,0 years in males.6
Ann association has been reported between the development of SCFE and endocrine disorders (including hypothyroidism, hyperthyroidism, hypopituitarism, and growth hormone deficiency) and renal disorders.3,5,6
Approximately 25% of SCFE cases are bilateral, but when unilateral, the left hip is more commonly affected.5,6 Most cases are idiopathic 3,5,6 and often there is no history of trauma or injury prior to symptom onset.3,5,6
The exact underlying mechanism remains uncertain, but it is hypothesized that displacement occurs due to a high physiologic axial load transmitted across a relatively weak physis.6 Conditions such as obesity increase the mechanical weight and force transmitted, while certain endocrine or renal disorders may contribute to weakening of the physis.6
The diagnosis of SCFE is based on symptoms and imaging findings. The most common symptoms are limping and pain that is poorly localized to the hip (52%), thigh (35%), knee (26%), or groin (13,9%).1,3 Distal thigh or knee pain may additionally occur, but the condition most commonly presents as an isolated symptom (15% of cases), which often delays the diagnosis.1
Restricted range of motion of the hip joint is a relevant finding on physical examination, and flexion and medial rotation are often limited. A well-known diagnostic finding is Drehmann's sign, which refers to abduction and lateral rotation of the hip joint in response to flexion.1
To avoid missing the diagnosis of SCFE, a thorough physical examination in the supine position should always be performed on patients who complain of symptoms around the hip joint, thigh, or knee joint. In addition, the mobility of the hip and knee joints should be compared bilaterally.1
The diagnosis is confirmed by bilateral hip radiography, which must include anteroposterior and frog leg lateral views.3
After the diagnosis is established, the correct classification of the disease is required1. SCPE is classified as stable or unstable based on the patient’s ability to bear weight.1-3,9 Classification is very important for prognosis and there is a significant relationship between the delay in diagnosis and an increased severity of dislocation1. The delay in diagnosis is associated with an increased severity of physeal slippage at presentation, and thus poorer long-term outcomes.1,8
The goals of treatment are to prevent slippage progression and complications such as avascular necrosis and chondrolysis.3,4
Stable SCPE is usually treated with in situ screw fixation. Treatment of unstable SCPE usually involves in situ fixation, but there is controversy about the timing of surgery, the need for reduction, and the use of traction.3 Open epiphyseal reduction and fixation may also be performed in these cases.3
In the present case, a prepubertal girl with obesity and subclinical hypothyroidism presented with limping and thigh pain of gradual onset that aggravated with hip rotation and flexion, without history of trauma. This suggested the diagnosis of SCPE, which was subsequently confirmed by radiographic examination. In situ fixation of the affected slippage was performed, as well as prophylactic fixation of the contralateral hip. The patient had a good recovery, with gradual improvement.