Introduction
Infection by Campylobacter spp., in particular C. jejuni and C. coli, is the main cause of acute bacterial gastroenteritis (ABG) in Europe,1 with a higher prevalence than reported for infections caused by Salmonella spp., Shigella spp., and enteropathogenic Escherichia coli.2,3 According to the latest report of the European Centre for Disease Prevention and Control, campylobacteriosis is the most frequently notified zoonotic disease in humans, with a growing incidence in recent years and the largest number of cases occurring in male children under five years old.4 In Portugal, recent data also shows an increasing prevalence of the disease, with C. jejuni being the most frequently identified etiological agent. Human campylobacteriosis is a compulsory notifiable disease since 2014.5
It is generally believed that Campylobacter acts by direct invasion of the intestinal epithelial cells, inducing an inflammatory process and producing a toxin.1,6,7C. jejuni infection in humans is usually sporadic and more frequent during the Summer months. Most etiological agents come from animal reservoirs (birds, cattle, goats, and sheep) and are transmitted by ingestion of poorly cooked meat (mainly poultry), unpasteurized milk and milk derivatives, and untreated water, with human-to-human transmission being very rare.8,9
C. jejuni causes aqueous diarrhea or diarrhea with mucus and/or blood in about half of cases. Other relatively frequent symptoms include fever, abdominal pain, nausea or vomiting, headache, and myalgia. The disease usually occurs 24-72 hours after ingestion of contaminated food or water and has an average duration of seven to ten days, although recurrences are not rare (25% of cases).9,10
The diagnosis is usually established by isolation of the bacteria in stools and identification of the etiological organism through mass spectrometry or biochemical and molecular methods. It can also be accomplished by direct microscopy/dark-field microscopy, specific antigen detection, identification of the bacterium DNA through polymerase chain reaction, and serology through ELISA technique.1,7,8
Treatment consists of restoration of the fluid and electrolyte balance. Antimicrobial therapy is only recommended in cases of high risk of severe disease, namely presence of dysentery, high fever, extraintestinal disease, symptom worsening or recurrence, symptoms lasting more than one week, concomitant chronic conditions, immunodeficiency, or pregnancy, and in outbreak situations. Macrolides are the first-line treatment.1,10
Campylobacteriosis is a self-limiting disease in most cases, particularly in healthy children, although complications have been reported, such as reactive arthritis, sepsis, Guillain-Barré syndrome, and hemolytic anemia.2,5
The aims of this study were to estimate the prevalence of Campylobacter spp. in the stools of pediatric patients with ABG, and characterize cases regarding clinical and epidemiological features, therapeutic approach, and associated complications.
Material and methods
A case-by-case review of the clinical records of patients evaluated in the Pediatric Emergency Department (ED) of a level II hospital between January 2013 and December 2017 was conducted. All patients with diagnosis of ABG by Campylobacter spp. were included. The diagnosis was established using a selective medium for isolation of Campylobacter spp. from stool samples and subsequent identification from a gallery of biochemical tests (API Campy).
Although the criteria or performing stool tests have some degree of individual variability, in the study hospital they are indicated in cases where the following signs/symptoms are present: frequent/intense abdominal cramps, high fever, prolonged diarrhea or diarrhea with mucus and/or blood, concomitant chronic conditions, immunodeficiency, and admission to the Pediatric Department with a diagnosis of ABG.
The following patient data were retrieved for clinical records: age, gender, date of Pediatric ED evaluation, area of residence, history of recent food intake, epidemiological context, clinical features (stool characteristics, presence of other symptoms), treatment, reason for admission, and disease progression.
Data were analyzed using the Statistical Package for the Social Sciences Program (SPSS Inc., Chicago. IL) version 23, through measures of central tendency and dispersion for quantitative variables and absolute and relative frequencies for qualitative variables.
Results
During the study period, 1990 stool tests were carried out in the Pediatric ED, 637 (32%) of which were positive for the presence of bacteria. Campylobacter spp. was identified in 459 cases (72%), followed by Salmonella spp. in 144 (22.6%), Yersinia enterocolitica in 37 (5.8%), and Shigella spp. in only one case (0.2%). No cases of Aeromonas spp. or Escherichia coli 0157 were detected. Bacterial coinfection was identified in four cases, one by Campylobacter spp. and Yersinia enterocolitica, one by Yersinia enterocolitica and Shigella spp., one by Campylobacter spp., Yersinia enterocolitica, and Salmonella, and one by Campylobacter spp. and Salmonella.
In addition to stool tests, virological stool examination was performed in 90.7% of patients with Campylobacter spp. isolated in stools, being positive in 7%: 4.1% for rotavirus, 0.7% for adenovirus, and 1.8% for both viruses.
From the 459 Campylobacter-positive stool tests, 18 were excluded for lack of data, making up a final sample of 441 patients, with a mean age of 3.2 years (standard deviation ± 4.2; range 1 month─17 years) and male predominance (57.8%).
The infection was predominant in the months of Spring to Autumn, with 11.1% of cases occurring in May, 10.9% in August, and 10% in October. C. jejuni was the main species identified (372 cases; 85.3%), followed by C. coli (21 cases; 4.8%), and C. upsaliensis (2 cases; 0.5%). No newborn was admitted to the Pediatric ED with ABG due to Campylobacter spp. infection.
Children included in the study were stratified by age group into infants (<1 year old), one-to-five-year-olds, six-to-10-year-olds, and older than 10 years old. The highest incidence of infection was observed in children aged one to five years (n=243, 55.1%), followed by infants (n=110, 24.9%) and children aged six to 10 years (n=49, 11.1%), and the lowest incidence was seen in children older than 10 years (n=39, 8.8%). Differences in incidence rates were statistically significant (p=0.042). Infants were further stratified according to age group into one-to-three-month-olds and four-to-twelve-month-olds, with the highest incidence reported in the latter (n=86, 78.2%).
Most patients had no data about consumption of suspicious food (n=367, 83.2%), and 39 denied its intake (8.8%). In cases with identification of a possible bacteria food source, untreated water was the most frequent (3.6%). Epidemiological causes were identified in 12.7% of cases, through reports of concomitant cases of diarrhea in the family, with no data available for 55.1% of cases.
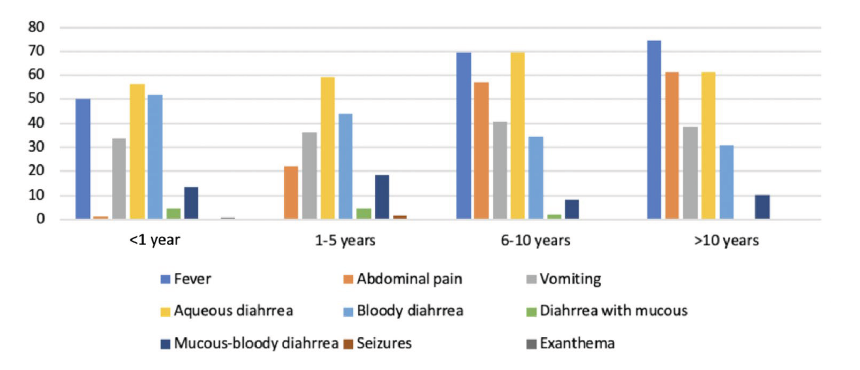
The forms of presentation included aqueous diarrhea (n=263, 59.6%), bloody diarrhea (n=193, 43.8%), mucous-bloody diarrhea (n=68, 15.4%), diarrhea with mucous (n=17, 3.9%), vomiting (n=160, 36.3%), abdominal pain (n=107, 24.3%), fever (n=278, 63.0%), seizures (n=4, 0.9%; all in the context of fever), and exanthema (n=1, 0.2%). Clinical presentation according to age group is depicted in Figure 1.
No statistically significant differences were found in clinical presentation across age groups, except for seizures, which mostly occurred in feverish context in children between one and five years old.
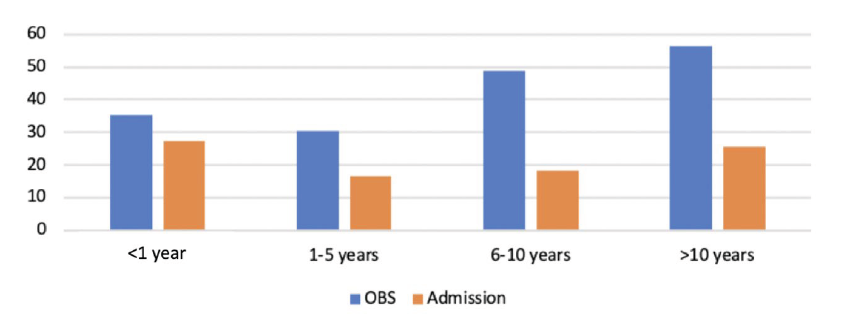
Among children observed in the Pediatric ED, 108 required a short hospital stay, and 104 were admitted to the Pediatric Department (PD; Figure 2). Admissions occurred mostly among infants younger than three months.
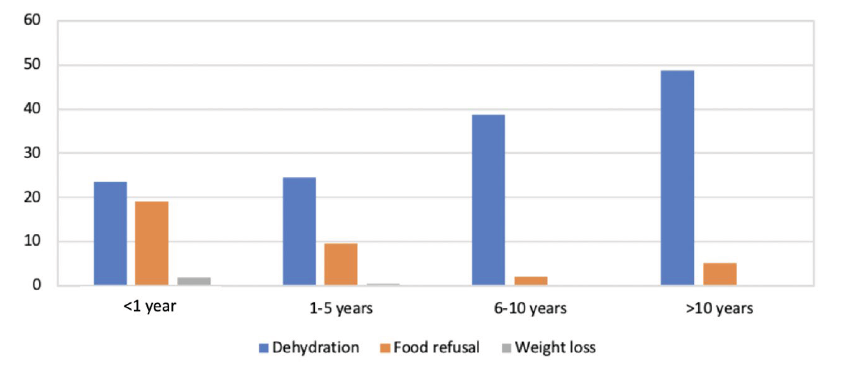
A total of 125 children (28.3%) were readmitted to the Pediatric ED for persistence or worsening of symptoms, 27 of whom (21.6%) were hospitalized (Figure 3).
Of all patients admitted to the PD, 28.8% (n=30) were younger than 12 months. The average duration of hospital stay was 3.2 days (range 1─10 days). During hospital stay, 94.4% received some form of treatment, including intravenous fluids in 92% (n=82) and antibiotic therapy in 12.4% (n=11; azithromycin in nine and clarithromycin in two). Four patients received antibiotic therapy directed at other coinfections.
A total of 143 samples were randomly selected for the study of antibiotic resistance patterns in the reference laboratory, with results showing resistance to quinolones in 93.7%, to tetracyclines in 83.2%, to macrolides in 11.9%, and to aminoglycosides in 0.7%.
A total of 156 children (37.9%) developed complications, mostly dehydration (n=120, 67.4%), but also food refusal (n=44, 24.7%; Figure 4).
After hospital discharge, 280 children (63.5%) were revaluated in outpatient setting. Control stool tests were carried out in 43.5%, with negative stool test results in 85.6% of these cases. A total of 15 children (3.4%) had more than one episode of ABG by Campylobacter spp. in the considered study period.
Discussion
Acute diarrhea remains a very common cause of ED admission, making ABG a condition with relevant epidemiological, economic, and social impact in pediatric age. Acute gastroenteritis usually has a benign and self-limited progression and viral origin. However, the prevalence of bacterial infection is significant.3,11,12
Campylobacter spp. was the main bacteria isolated in the present study, accounting for 72% of positive stool tests, followed by Salmonella spp. (22.6%). The higher prevalence of Campylobacter spp. compared to other bacteria has been reported in national and international studies.8,13,14,16
Four studies focusing on acute gastroenteritis in pediatric age in Portugal with a similar methodology to the present one have been previously published. Three of these had comparable findings to this study: a multicenter study carried out in the north of Portugal in 2005, a study carried out in Lisbon and Tagus Valley in 2016, and a study carried out in the central region of Portugal in 2014.8,9,13-16 In the fourth study, Salmonella spp. was the most frequent etiological agent (found in 54% of positive co-cultures), followed by Campylobacter spp. (23%).9 In another study assessing only hospitalized patients, Escherichia coli was the most frequent etiological agent (43%), followed by Campylobacter spp. (37%).15 However, this study had a different methodology from the current one, precluding the comparison of results.15 Regarding Campylobacter species, C. jejuni was the most frequently associated with ABG, with an increase in the number of cases diagnosed over the years, in agreement with other studies.2,5,8,13
The percentage of viruses and bacteria coinfection in this study was 7%, a value similar to the one found in the literature.13 A higher number of cases was found in children aged between one and five years, but also a high number of cases in children under one year, in agreement with the recently published national report5 and three of the above-mentioned national studies.9,13,14 In the study conducted only in patients admitted to the PD,15Campylobacter spp. was the most frequent pathogen detected in patients aged 12 months and older, and particularly in those over five years. However, this study included a small sample size and hospitalized patients, a population with different clinical characteristics from the one included in the present study. Regarding gender distribution, this study found a predominance of Campylobacter spp. in males, also verified in two national studies.8,13
This study has as main limitations its retrospective nature, the use of clinical criteria for performing stool tests, and the scarcity of data available in some clinical records, which hindered the identification of the probable source of infection in some cases and the presence of family cases in others.
Clinical manifestations at presentation were similar between this study and two of the national studies available in the literature.9,14 The presentation during the first year of life was similar to other age groups, but seizures were only present in children aged one to five years. According to the literature, aqueous diarrhea is found in about half of cases, which was also observed in this study.2,7 The high frequency of cases of diarrhea with blood or mucous in this sample likely represents a data bias related to the fact that stool tests are much more often required in presence of this type of presentation.
Although undeniably relevant from an epidemiological point of view, etiological study is recommended in cases where targeted therapy is indicated or to aid in the differential diagnosis.3 The isolation rate of pathogens in stools in the present study was 32%, similar to that registered in other studies.8,9,15
Importantly, 89 patients (20.2%) were hospitalized in the PD, on average for 3.2 days, 82 of whom required intravenous hydration. Other studies reported hospitalization rates between 10% and 55%.8,9,13,14 As per recommendations, antimicrobial treatment was prescribed in selected cases. Only 11 patients (12.4%) received directed antibiotic therapy (nine azithromycin and two clarithromycin). The very low prescription rate of antibiotics is justified by the fact that treatment of this enteritis is unspecific, and the evolution of bacterial diarrhea is generally self-limited. The choice of medication was mostly empiric, taking into account the most frequently isolated pathogens and their susceptibility. In the group of samples submitted to antibiotic sensitivity test (AST), a pattern of antibiotic resistance similar to the one described in the literature was found, although with a higher rate of quinolone resistance.17,18
At the time of ED discharge, caregivers were educated about warning signs that should be monitored and those requiring prompt medical reassessment. The clinical course was generally favorable, with a low rate of complications and PD admission.
Conclusion
ABG in children remains one of the most common causes of hospital admission and a major public health concern in Portugal. Campylobacter spp. is currently the most frequent cause of acute bacterial diarrhea in developed countries. An increase in the number of new diagnoses has been reported in recent years for reasons yet to be clarified. Although ABG is mostly a self-limited disease with favorable clinical course, the occurrence of associated complications and/or other forms of more serious and potentially fatal infections should be considered. Stool test enables the etiological identification, which is crucial in cases requiring directed therapy.
The increase in the number of cases diagnosed over the years suggests the need to raise awareness of professionals in primary health care for appropriate hygiene measures in the manipulation and preparation of meals to be conveyed to their patients.