Introduction
Tuberculosis (TB) remains the most common cause of death from infectious diseases worldwide.1 Although its incidence is decreasing, the prevalence of the condition remains a substantial concern.2 Extrapulmonary TB with musculoskeletal involvement occurs in about 10-15% of cases, mainly affecting joints and bones.2,3 Of these, only 1-5% reportedly manifest as synovitis of the flexors of the hand, and even these cases are more commonly attributed to non-tuberculous mycobacteria.4,5 Nonetheless, mycobacterium tuberculosis involvement has been described in some cases of isolated tenosynovitis. The majority of cases occur in adult patients, with few reports in children or adolescents. Since this is an unusual TB presentation in the pediatric setting, frequently with an insidious onset and non-specific clinical signs, it is often misdiagnosed and mistaken for other more common clinical conditions, as wrist ganglion, De Quervain’s disease, or carpal tunnel syndrome.3 Prompt diagnosis and treatment are often delayed, and if left untreated chronic synovitis may lead to tendon rupture. The aim of this report was to highlight the importance of early symptom recognition in adolescents with chronic pain suggestive of a less common condition, especially when both medical and surgical management options appear ineffective.
Case report
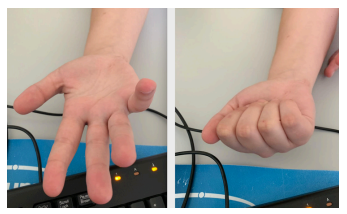
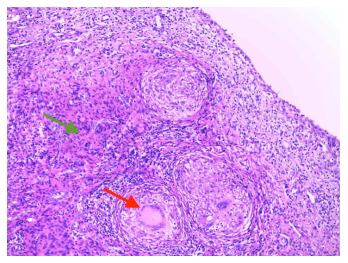
Herein is reported the case of a 15-year-old female adolescent followed at the Orthopedic Outpatient Clinic due to chronic hand pain following trauma to the right hypothenar region and flexor carpi ulnaris one year before. She was admitted to the Pediatric Emergency Department (PED) at the time of trauma and conservatively managed. In the following months, the girl returned to PED with similar pain complaints. X-ray imaging revealed no signs of additional hand injury, but the girl was referred to the outpatient clinic for further study. Magnetic resonance imaging (MRI) showed tenosynovitis of the common flexors of the right hand and rupture of the superficial flexor tendon of the small finger (Figures 1 and 2). The patient initially underwent physical therapy with no significant relief. She was ultimately proposed for surgery and underwent pulley release and synovectomy of the flexor tendons in a private clinical facility, being lost to follow-up. Five months after surgery, she returned to PED with persistent right hand pain. She shared the histopathological report previously performed, which evidenced severe chronic synovitis of the flexor tendons of the right wrist and caseous central-necrotic granulomas, highly suggestive of tuberculous disease. Acid-Fast stain was negative. Personal history was again carefully retrieved, but no known contacts with active or past disease or recent traveling outside the country were identified. The etiological study was continued, with no relevant findings in chest radiography but positive results in both Tuberculin Skin Test and Interferon-Gamma Releasing Assay. At this point, tuberculous involvement of the flexor tendons of the right hand with concurrent chronic synovitis was assumed. The patient complied with 12-month anti-tuberculous chemotherapy with isoniazid, rifampicin, pyrazinamide, and ethambutol for two months, followed by isoniazid and rifampicin for ten months. Five years after the initial hand trauma, the patient remained under clinical surveillance, with persistent chronic pain and intermittent paraesthesia of the right hand, although less severe than before treatment. Additionally, functional limitation of flexion of the 4th and 5th fingers of the right hand persisted as a chronic synovitis complication (Figure 3).
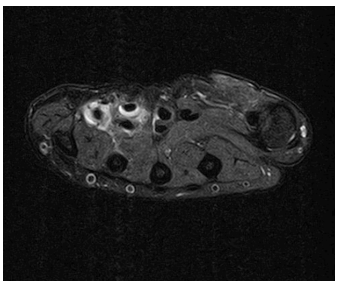
Figure 1 Magnetic resonance imaging of the wrist. Axial T2 fat saturation image showing hyperintense signal surrounding the flexor tendons of the 4th and 5th fingers, with partial rupture of the 5th finger tendon, suggesting traumatic tenosynovitis.
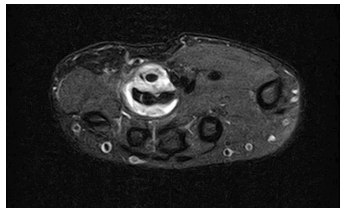
Figure 2 Magnetic resonance imaging of the wrist. Axial T2 fat saturation image showing hyperintense signal surrounding inflammation of the flexor digitorum superficialis and profundus of the 4th finger.
Discussion
The global burden of TB in children and adolescents remains a public health challenge, not only because a definite diagnosis is difficult to establish but also due to the frequency of extrapulmonary disease. Musculoskeletal involvement represents a rare extrapulmonary TB manifestation, especially in children. Nevertheless, tendon synovitis can cause chronic inflammation of all tendon sheaths around the hand and wrist, resulting in median nerve compression.6,7 Flexor tendons of the dominant hand are much more involved than extensor tendons. The diagnosis is challenging due to the insidious nature of the condition and is often suggested when symptoms like swelling and mobility limitation become apparent. Local inflammatory signs can also be scarce.4
When synovitis is diagnosed, further study is warranted to establish the origin, especially when an infectious cause is suspected. Exams such as tendon sheath aspiration/biopsy, subsequent microbial cultures, and histopathological examination are important to confirm the diagnosis. Imaging studies as MRI may be useful to define the anatomic extent of infection, guide surgical planning, and exclude other complications11. Plain radiographs are usually normal in these cases. In our case, an invasive surgical procedure by imaging alone was performed soon after diagnosis to prevent further functional hand disability. Synovitis was thought to have a traumatic rather than infectious origin, thus no further initial investigation was performed. Although contagion sources could not be determined in this patient, the initial infection may result from direct or hematogenous inoculation from either an active or sleeping pulmonary source. Infections caused by mycobacteria continue to pose a diagnostic challenge due to their paucibacillary nature on musculoskeletal disease and fastidious growth pattern.5
Factors like trauma can also be responsible for tuberculous reactivation in as much as 30% of cases.4 Considering that trauma to the right hand was the initial symptom trigger in this case, it can be speculated that this flared up the otherwise slowly progressing disease. Moreover, it is possible that tuberculosis may be transmitted from the environment to humans, since Mycobacterium tuberculosis superfamilies are also isolated from soil and water (8).
Regarding disease progression, Kanavel described a three-stage histological evolution pattern in tuberculous tenosynovitis.9 The present case has characteristics of thresholds of both stage 2 (granulation tissue with or without the appearance of “rice bodies”) and stage 3 (fungosities associated with extensive caseous necrosis; Figure 4) histology. Bacteriology is positive in direct examination only in 20% of cases and cultures are negative in up to 45%.4 This was a downside in this case, since surgery and surgical specimen processing were not undertaken due to the delayed availability of such procedures. Despite the lack of microbiological evidence, the diagnosis was inferred due to high clinical and anatomopathological suspicion.
Once the condition is diagnosed, prompt medical management with antituberculous chemotherapy (ATC) should be started. According to Sbai et al., induction therapy consists of a combination of drugs including rifampicin, pyrazinamide, and ethambutol for two months.4 After this initial period, patients should remain on ACT treatment for an additional four to ten months, ideally with isoniazid and rifampicin, but ultimately depending on clinical and radiologic evolution.5 Still, the minimum treatment duration for TB bone and joint involvement remains to be defined. Surgical treatment is usually performed for diagnostic or therapeutic purposes related to disease complications, but surgical debridement is controversial.2,10 Although modern surgical and medical treatments improve recovery of the condition, significant long-term morbidity can still occur, as in the present case.5
In conclusion, though isolated tuberculous tenosynovitis of the hand is a rare condition, all orthopedic surgeons should consider it in the differential diagnosis of chronic hand pain. A delay in diagnosis, ACT initiation, and surgical treatment can severely limit the sensory and motor function of the hand, which is why this condition remains a clinical challenge in daily practice, especially in the pediatric setting.