Introduction
The COVID-19 pandemic stroke Portugal in March 2020 and a state of emergency was decreed from March 19 to May 2, forcing a mandatory confinement with restrictions on public circulation1. These measures led to an almost 45% nationwide decrease in hospital emergency admissions during the first month of the pandemic.2
In the last decades, an overburden of the Pediatric Emergency Room (PER) activity has been observed, particularly with non-urgent conditions.3-8 The PER of Centro Hospitalar Barreiro Montijo (CHBM) underwent an annual increase in admissions, making it relevant to analyze its activity in a pandemic setting.9
This study aimed to analyze the emergency episodes occurring during the state of emergency and compare them with the previous, pre-pandemic year, as well as to assess patients’ disease severity in both periods.
Material and methods
This was a retrospective analytical observational study of patients admitted to the PER of CHBM during the state of emergency (March 19 to May 2, 2020) and homologous period of the previous year (March 19 to May 2, 2019). Patients’ anonymity and confidentiality were preserved during data collection. This study was approved by the Ethics Committee of CHBM.
Data collection
The study database was provided by the statistics office of CHBM. The following variables were collected for each PER admission: age, gender, admission origin and cause, recurrences during the study period, and discharge destination. Age parameter was clustered into five groups: <1 year old, 1-4 years old, 5-9 years old, 10-14 years old, and 15-18 years old.
Patients’ diagnosis at PER admission was collected by consulting their clinical files. A randomly selected sample of the 2019 period with the same number of admissions as in 2020 was used for comparison. Randomization was performed using a key generated in Microsoft Office Excel® 2010. Diagnoses were coded according to the International Classification of Diseases 10th (ICD-10) and later grouped.
Information regarding SARS-CoV-2 tests performed in 2020 and their results was also collected.
The following markers were considered for assessing patients’ disease severity: number and duration of hospitalizations; Observation Room admissions; transfers to other hospitals; referrals to hospital consultations upon discharge; and deaths.
Statistical analysis
Categorical variables were presented as frequency and percentage, and continuous variables as mean and standard deviation. Descriptive analyses for each year were tabulated. Descriptive statistics for each year and p-values of comparisons between the two years were tabulated. The equality test of two proportions with continuity correction and student’s t-test with Welch correction were used for mean comparisons. P-values lower than 0.05 were considered statistically significant. Analyses were performed using R software version 3.4.2 and Microsoft Office Excel® 2010.10
Results
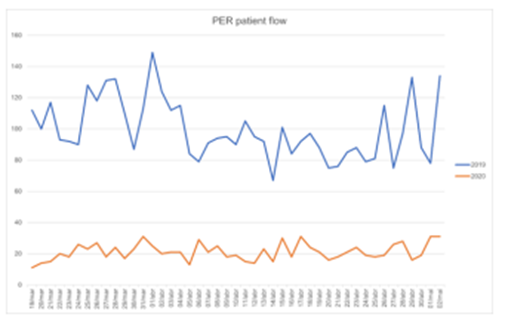
The number of admissions to the PER of CHBM during the considered periods was 4481 in 2019 and 956 in 2020, representing a 78.7% decrease in admissions during the state of emergency (Figure 1).
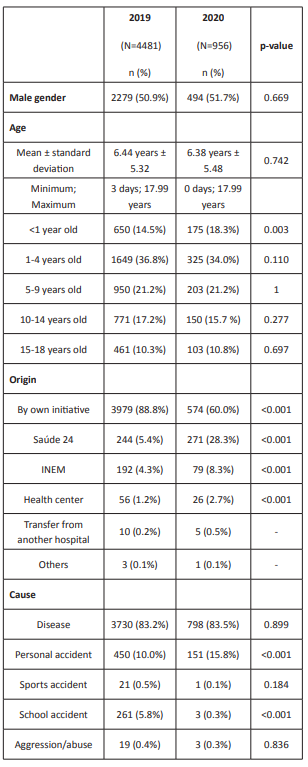
Gender and mean age were similar in both years, as shown in Table 1. The most frequent age group in PER admissions in both periods was the 1−4-year-old group (36.8% in 2019 vs 34% in 2020). There was a statistically significant relative increase in admissions in the <1-year-old group in 2020 (14.5% in 2019 vs 18.3% in 2020; p=0.003), with no significant differences in the remaining age groups.
Most PER admissions were parent/caregivers’ initiative (88.8% in 2019 vs 60.0% in 2020; p <0.001). However, an increase in PER referrals was observed in 2020, namely from Saúde 24 (5.4% in 2019 vs 28.3% in 2020; p <0.001), primary care (1.2% in 2019 vs 2.7% in 2020; p <0.001), and the National Institute of Medical Emergency (INEM) (4.3% in 2019 vs 8.3% in 2020; p <0.001) (Table 1).
In both periods, admissions mostly occurred due to illness (83.2% in 2019 vs 83.5% in 2020). However, a significant reduction in their absolute number was seen in 2020 (3730 in 2019 vs 798 in 2020), corresponding to a 78.6% decrease in PER admissions due to illness (Table 1).
The percentage of accidents was similar in both periods (16.3% in 2019 vs 16.2% in 2020). But a difference was observed in their typology, with a decrease of school accidents (5.8% in 2019 vs 0.3% in 2020; p <0.001) and an increase in personal accidents (10.0% in 2019 vs 15.8% in 2020; p <0.001) in 2020. A global reduction of 78.9% in all types of accidents was also noted. It should be highlighted that school accidents in 2020 occurred prior to the implementation of the state of emergency. Also of note, there was a decrease in the absolute number of PER admissions for aggression and abuse in 2020 (19 in 2019 vs 3 in 2020).
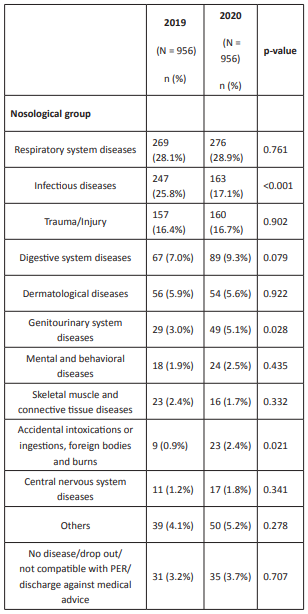
According to the ICD-10 classification system, most diagnoses concerned the respiratory system or were due to infectious and trauma/injury causes in both periods (Table 2). A statistically significant difference was found between both periods regarding the diagnosis of infectious diseases (decreased from 25.8% in 2019 to 17.1% in 2020; p <0.001), genitourinary diseases (increased from 3.0% in 2019 to 5.1% in 2020; p=0.028), and accidental intoxications or ingestions, foreign bodies, and burns (increased from 0.9% in 2019 to 2.4% in 2020; p=0.021).
During the state of emergency, 266 SARS-CoV-2 tests were performed by real-time polymerase chain reaction (RT-PCR) on nasal and oropharyngeal exudates (corresponding to 33.3% of admissions due to illness). Of these, 6.4% (n=17) were positive, with only one patient hospitalized for reasons unrelated to COVID-19 (acute pyelonephritis in a teenager with uropathy).
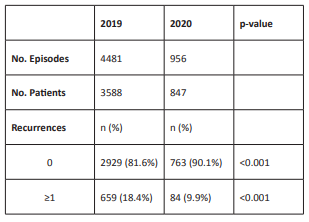
Analyzing the number of patients (and not admissions), a statistically significant reduction was observed in the number of recurrences in 2020 (18.4% in 2019 vs 9.9% in 2020; p <0.001) (Table 3).
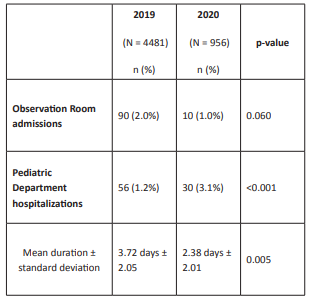
The number of Observation Room admissions decreased from 2019 to 2020 (90 in 2019 vs 10 in 2020; p=0.060) (Table 4).
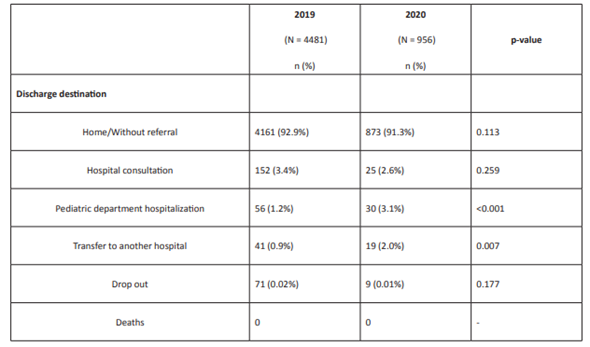
Concerning the discharge destination (Table 5), most patients were discharged home without referral in both years (92.9% in 2019 vs 91.3% in 2020). Despite the decrease in absolute numbers (41 in 2019 vs 19 in 2020), a relative increase was found in transfers to other hospitals (0.9% in 2019 vs 2.0% in 2020; p=0.007), mainly due to the need for specialized evaluation. Pediatric Surgery accounted for most transfers (39% in 2019 vs 47.4% in 2020), followed by Ophthalmology (12.2% in 2019 vs 5.3% in 2020), Orthopedics (12.2% in 2019 vs 5.3% in 2020), Otorhinolaryngology (9.8% in 2019 vs 10.5% in 2020), and Child and Adolescent Psychiatry (4.9% in 2019 vs 15.8% in 2020). Similarly, the absolute number of Pediatric Department hospitalizations decreased (56 in 2019 vs 30 in 2020), with an increase in relative numbers (1.2% in 2019 vs 3.1 % in 2020; p <0.001). However, a statistically significant reduction was found in the duration of hospitalizations in 2020 (mean of 3.72 days in 2019 vs 2.38 days in 2020; p=0.005) (Table 4). No differences were found in hospital consultation referrals, and mortality rate was zero in both periods.
Discussion
During the state of emergency, an approximately 80% decrease in PER admissions in CHBM was noted. This can be explained by a reduction in the frequency of the main reasons for attending PER, such as infectious diseases, sports/school injuries, and car accidents.2 Social distancing, with longer periods at home, can justify this, by breaking the chains of infection and reducing the number of accidents.2,11 Another factor that can explain the decrease in admissions is the low number of COVID-19 cases in pediatric age and the fact that, even when infected, most children had mild or no symptoms.12-14 Moral conscience for preventing overload of health services, as well as limitations in transportation and fear of COVID-19 may also have contributed for this reduction.2 A statistically significant drop in recurrences was also observed during this period, what can be understood as a direct consequence of the above-mentioned reasons.
Data regarding gender and the higher proportion of children with 1−4 years observed are consistent with previous reports.6,7,15-17 The relative increase in infant admissions during the state of emergency can be attributed to the restricted access to primary care and pediatric consultations, particularly relevant in these ages.18 Greater parental concern, as well as a reduction in admissions in the remaining age groups, may also be contributing factors.19
The statistically significant increase in hospital referrals by Saúde 24, healthcare centers, and INEM during the state of emergency reflects a compliance with DGS-recommended measures regarding the use of pre-hospital health care.1 It should be noted that the decrease in PER admissions during the state of emergency was mainly due to a reduction of patient attendance by their own initiative/without referral.
In both periods, the number of episodes due to illness was higher than due to accidents, aggressions, or abuse, which is in accordance with data in the literature.15,16 A variation in their proportion (illness vs accidents) was not found, with absolute numbers decreasing in about 80%. Thus, contrary to what was hypothesized, an increase in the number of admissions due to accidents was not observed during the state of emergency.2
Regarding accident typology, the decrease in school and sport accidents in 2020 was expected, due to closure of schools, daycare centers, and kindergartens, as well as sport associations and gyms.2 This reduction led to a subsequent increase in the percentage of personal accidents, without an increase but rather a decrease in absolute numbers. The increase in accidental intoxications or ingestions, foreign bodies, and burns can be explained by longer periods at home, increasing the possibility of domestic accidents2. Also teleworking, with parents having to divide their attention between professional duty and parenting and paying less attention to children, potentially enhanced these accidents.20
It should also be noted that an increase in domestic abuse was not seen during the state of emergency. This result was unexpected, considering the potentially longer coexistence between aggressor and victim.2 Nevertheless, this may not represent the reality, but instead victim isolation and abuse perpetuation, which is particularly worrisome given the current pandemic situation.
Regarding diagnoses upon discharge and respective nosological groups, a significant drop in diagnoses of infectious diseases during the state of emergency was observed, possibly due to the break in chains of infection due to school, daycare center, and kindergarten shutdown.2,11 The increase in genitourinary disease diagnoses may be justified by the significant drop in infectious disease diagnoses.
In both periods, patients were mostly discharged home without referral, and hospitalization rate was low, which is in agreement with the literature.5,6,21 The increase in the percentage of transfers to other hospitals and hospitalizations seen during 2020 could represent an increase in patients’ disease severity. However, this should be interpreted with caution. Structural changes imposed by the pandemic were made in CHBM, making it impossible to have an observation room for patients with respiratory symptoms or fever. As so, hospitalization rates in the Pediatric Department in 2020 may be overestimated due to short-term hospitalizations (that would normally only occur as Observation Room admissions), which is supported by the decrease in the mean duration of hospitalizations (p=0.005). It should also be noted that this refers to a relative increase and that the actual absolute number of hospitalizations and hospital transfers decreased in 2020. Referrals to hospital consultations upon discharge did not increase, and no deaths occurred in both periods. Therefore, the global analysis of indicators considered for assessing patients’ disease severity suggests that no significant increase was seen in disease severity during the state of emergency and that patients who actual met criteria for using PER continued to do so.
This study has some limitations and possible biases that should be acknowledged, including: a 2019 sample was used for comparing diagnoses, which may not be representative of that year; the interpretation of patients’ disease severity did not take into account the clinical priority (color tags in medical triage); the presence of chronicity was not evaluated; the study considered a short period of time; the comparison was made for two periods with different characteristics regarding population and health care structure and organization, which are difficult to measure and were not taken in account. The state of emergency changed the normal functioning of CHBM services and primary health units on the dependency of PER, as well as the population itself, which was affected by confinement and border and air connection closure, characteristics that have not been explored.
Conclusion
In conclusion, compliance with DGS isolation measures and recommendations appears to have been met during the state of emergency. There was a significant reduction in PER admissions, particularly from patients without referral and recurrences, with no increase in patients’ disease severity. This highlights the importance of healthcare education programs, together with optimized links between primary and secondary care to help reduce PER overflow/misuse. Lessons from this pandemic should be used to build a bridge to a new and better paradigm of use of the National Health Service. In the future, it would be interesting to carry out additional studies focusing other confinement periods.