INTRODUCTION
A kidney transplant procedure is a surgery in which a healthy kidney is inserted into a person suffering from stage 5 chronic kidney disease (CKD). The donated kidney may come from a living or a deceased person, and this procedure may be performed on a patient who is already on dialysis (either hemodialysis or peritoneal dialysis) or one that has not yet entered a dialytic program, in which case it is called a preemptive transplantation.
Kidney transplantation improves both the patient´s survival and quality of life in comparison with the dialysis treatment. In addition, kidney transplantation is less costly than dialysis in the long run.
These facts are, on their own, strong arguments to consider transplantation as the preferential treatment modality for stage 5 CKD, when patients have no major comorbidities. Given the importance of controlling climate change, it is worth noting that kidney transplantation is more environmentally sustainable than dialysis. This provides another strong argument for increasing the practice of kidney transplantation in renal care.
In the following lines, the benefits of kidney transplantation as well as its constraints will be discussed, focusing on the Portuguese reality. Aspects of the economic and environmental impact of this technique will also be mentioned, as well as some improvement measures that could be implemented in this field.
THE BENEFITS OF TRANSPLANTATION OVER DIALYSIS FOR CKD PATIENTS AND THE PLANET
Although no randomized controlled study can be performed in this specific area, since it is not possible to randomly assign patients to either the transplant or dialysis treatment groups, most observational studies have confirmed that kidney transplantation improves patients’ survival and gives better quality of life than dialysis.1,2,3 In spite of its advantages, kidney transplantation may not be the best treatment option for all stage 5 CKD patients. A recent meta-analysis on cost effectiveness of renal failure treatments showed that kidney transplantation may not be cost-effective for elderly patients with comorbidities, as adverse results are more likely to occur.4 Nevertheless, in large cohorts, kidney transplantation is usually less costly than dialysis.1,4,5
Furthermore, kidney transplantation is a more environmentally friendly modality to our planet in comparison with dialysis - it consumes less plastic, less water, and less energy than either hemodialysis or peritoneal dialysis. Hemodialysis modality requires an installation facility, a water treatment system and dialysis machines as well as a lot of consumables, including dialysis filters, blood and dialysate lines, needles, gloves and all the personal protective equipment for healthcare professionals. Most of these consumables contribute to a large amount of waste that also has to be managed and processed. The large majority of hemodialysis patients have to travel significant distances 3 times a week, contributing to the carbon footprint that is harming planet earth. Peritoneal dialysis, although usually seen as better for the planet and a less costly modality than hemodialysis, is not environmentally harmless - the manufacturing of its solutions is also polluting, the plastic consumables (bags and lines) are significant and the distances to deliver the dialysis solutions at patients’ homes may also be substantial.6 An analysis of the environmental impact of dialysis in comparison with kidney transplantation, concluded that there was no significant difference between hemodialysis and peritoneal dialysis, but kidney transplantation had a 90%-95% lower environmental impact than the aforementioned techniques.7
CHALLENGES AND LIMITATIONS OF KIDNEY TRANSPLANTATION
Several factors limit kidney transplantation implementation. The shortage of organs for transplantation limits the accessibility of this modality of CKD stage 5 treatment.8,9 Additionally, renal transplantation is not the suitable treatment for all CKD stage 5 patients, namely patients with multiple comorbidities, active cancer, advanced cardiovascular or cerebrovascular disease and those with short life expectancy, in whom this surgical procedure and the need of permanente immunosuppression would not bring any benefit and could, in fact, worsen their overall prognosis.
Despite its numerous advantages, the success of this procedure is not free of risks or guaranteed. The recipient is subjected to a surgical procedure, which carries a certain degree of risk by itself. The quality of the organ, the age and health status of the recipient, his adherence to the medication and healthy lifestyle measures, the quality of the medical follow-up and the treatment of the medical complications like infections, drug toxicity, control of cardiovascular and other diseases, all contribute to the outcome of kidney transplantation.10
Additionally, transplantation is a complex and expensive procedure that requires a highly specialized team and infrastructure. It envolves extensive pre-operative evaluations, including laboratory tests, imaging, and immunological assessments to match the donor and recipient.
The post-operative care and follow-up require a multidisciplinary team, including nephrologists, surgeons, nurses, pharmacists, and other healthcare professionals.
A BRIEF SUMMARY OF THE ORGANIZATION AND REGULATION OF ORGAN PROCUREMENT AND TRANSPLANTATION IN PORTUGAL
The organ procurement and transplantation activity in Portugal, is regulated by the Instituto Português do Sangue e Transplantação (IPST), which belongs to the Ministry of Health and is integrated in the National Health System.11 The overall activity is coordinated by the Coordenação Nacional da Transplantação, belonging to the IPST.
The immunological analysis of the waitlist candidates and the potential organ donors, which is essential for determining histocompatibility and reducing transplant rejection, is performed within the three Centros de Sangue e da Transplantação (located in Lisbon, Coimbra, and Porto) that nowadays are also integrated within the IPST.12 There are 5 offices that coordinate the organ procurement and support its logistics - these are named Gabinetes Coordenadores de Colheita e da Transplantação (GCCT). Two of these are located in Porto; one is in Coimbra and the other two are located in Lisbon. Within each hospital, there is a donation coordinator (Coordenador Hospitalar da Doação).13
This medical doctor is responsible for the detection and signalling of potential deceased organ donors to the GCCT (Fig. 1). When a donor is signalled, there are a series of complex procedures that must be performed in order to ensure the success and quality of the harvesting, and that culminate, after retrieval, in the delivery of the organ to the transplantation unit. Nowadays there are 7 kidney transplantation centres in Portugal - two in the north region (Porto), one in the central (Coimbra) and 4 in the Lisbon area. Portugal has adopted a presumed consent model for organ donation since 1993, which means that every citizen is considered a potential donor unless they explicitly opt out.
This model, along with the efficient organization of the organ donation and transplantation system, has contributed to the high donation rate and the successful outcomes of transplantation in Portugal.14,15
After transplant surgery, most of the kidney transplant recipientes are followed by the same transplantation centre where this procedure took place for as long as their kidney graft is functioning.
The evaluation and selection of CKD patients to the transplant waiting list is performed within the 7 kidney transplantation centres. Most patients are referred to the pre transplantation evaluation by their nephrologist from the pre dialysis medical appointments or, more frequently, from their dialysis Unit. Given that most patients evaluated for transplantation have several comorbidities, they may need a multidisciplinar approach and multiple diagnostic exams. So, for most patients, the inclusion within the active waiting list is not immediate and it often takes months, for a patient to have their medical evaluation complete. Most centres carry out face-to-face consultations (video consultation is very rare). Most of the diagnostic exams are carried out under the responsibility of the transplant centre, which poses a significant burden to the Hospital. Each patient may be registered and evaluated within 2 transplantation centres. In order not to duplicate diagnostic exams and evaluations, it is fundamental to have a good communication system among the different institutions/ hospitals of the national health system. Unfortunately, that is still not the case in Portugal, although there have been some efforts towards this purpose in the last years. In conclusion, the process of the medical evaluation for a kidney transplant candidate in Portugal is not simple or easy - not to the patient or the highly differentiated medical team committed in this activity.
As previously mentioned, after a successful transplant procedure, the long-term follow-up of most of the kidney transplant recipientes is performed within the same institution. This is because in Portugal, the peripheral follow-up of these patients within the National Health System, is not allowed. In fact, only a small number of kidney transplant recipients are medically accompanied outside the transplanting centre. This is true for patients living in Madeira Island, in some Azores islands and in two regions in the center and north of Portugal.
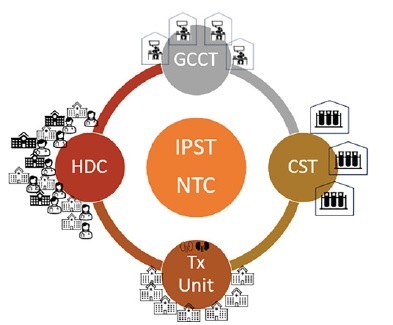
Figure 1 Simple representation of the Portuguese donation and transplant organization (see text for details)
All the other patients are followed within the transplanting centres. As the population of kidney transplant recipients is constantly growing, one can imagine the challenge and the burden this poses to the limited medical teams of those hospitals. This is not a sustainable policy in the long run. In order to make matters worse, carrying out diagnostic exams, including laboratory tests, such as assessment of immunosuppressant levels or cytomegalovirus or BK virus viral load, which are common evaluations in this population, can only be performed in the institution where patients are followed. Thus, these patients have to travel to the hospital, sometimes traversing hundreds of kilometres and losing a day of work, just for a routine medical evaluation.
NEW APPROACHES TO EVALUATE AND FOLLOW-UP KIDNEY TRANSPLANT CANDIDATES AND RECIPIENTS
According to a study about the use of telemedicine in kidney transplantation, using video clinical visits might help to overcome the obstacles faced by individuals seeking kidney transplants who encounter difficulties related to location, finances, and logistics when trying to engage with a transplant centre and maintain post-transplant care.16 By utilizing synchronous video visits, telemedicine could enable transplant centres to initiate the evaluation process for potential recipientes and donors who could not easily visit the centre in person or when the institution itself faces limitations on clinic capacity, such as during a pandemic. Furthermore, telemedicine might allow transplant centres to provide ongoing follow-up care for transplant recipients, eliminating the need for travel and the associated expenses. This article shows a possible scheme for the implementation of such a program either in pre and post-transplant care for both kidney recipients and living donors. However, the expansion of telemedicine-based kidney transplant services depends on the availability of telemedicine infrastructure, which may not yet be easily available - as is the case of Portugal’s Health System. Regardless, the use of such tools could help reduce costs in the evaluation and follow-up of patients involved in kidney transplantation.
A single centre randomized controlled trial, prospectively followed for 12 months, a group of 46 living donor kidney transplant recipientes that were approached according to the standard of care (23 patients) or by that mode and telemedicine (23 patients).17 According to the paper, telemedically supported case management was associated with better adherence to immunosuppressive medication and better clinical outcomes, compared to standard care. Specifically, the telemedicine group had a higher proportion of patients with good adherence to immunosuppressive medication (91.7% vs 70.8%) and a lower proportion of patients with poor adherence (8.3% vs 29.2%). In addition, the telemedicine group had fewer hospitalizations (0.5 vs 1.2 per patientyear) and fewer emergency department visits (0.3 vs 0.6 per patientyear) compared to the standard care group. Only the intervention group achieved their pre-agreed levels of adherence, disease-specific quality of life, and return to employment.
In 2022, six Italian transplant surgeons and nephrologists convened via teleconference to develop a consensual model of video visits for the follow-up of kidney transplant recipients.18 The video visit was consensually recognized as the most relevant for the follow-up of kidney transplant recipients. Eligible patients should have basic electronic devices and the skills to correctly use them and be in clinically stable condition. With the exception of physical and instrumental examination, and kidney biopsy, the authors considered that all other described assessments were feasible during a video visit and could be implemented by specific training and use of supporting tools. This video visit model was simple and assumed to be adaptable to most transplant patients. It did not intend to replace face-to-face examinations but could be an additional tool for improving the intensity of follow-up of kidney transplant recipients, which could be integrated into current monitoring protocols.
A report from a group based in Philadelphia (Thomas Jefferson University), states that the kidney transplant program rapidly adjusted workflows to convert 98% of transplant clinics into telemedicine sessions successfully.19 The ability to access telemedicine platforms through simple mobile applications, increased patient participation by removing technological barriers and enabled seamless virtual patient and provider interaction. This rapid deployment of resources resulted in a dramatic institution-wide increase from 50 telemedicine visits a day to more than 3000 visits a day. The article also describes an “agile listing model” for pre-transplant evaluations, that entailed virtual education and consenting, followed by history taking and medication reconciliation by the transplant coordinator. From there, a telemedicine physician evaluation was conducted followed by evaluations by a social worker, dietician and financial coordinator over a secure video-conferencing platform. This model has increased the inactive status of listings from 30% to 33% in just six weeks. In addition, the kidney transplant program was orchestrating at-home phlebotomy for waitlisted and post-transplant patients. The article concludes that telemedicine delivered through a Health Insurance Portability and Accountability Act (HIPAA)-compliant platform is na effective care delivery model that could be used to care for immunocompromised transplant patients in the safety of their homes while observing social distancing.
SUGGESTIONS TO MAKE KIDNEY TRANSPLANTATION MORE SUSTAINABLE AND CONVENIENT FOR PATIENTS AND CLINICIANS
Apart from the long-asked possibility of exporting the follow-up of kidney transplant recipients, other solutions, of easier implementation, could be available that would facilitate both patients and their specialized medical team’s daily life. As previously described, telemedicine could be one of those measures - it could be used in a complementary way to in-person visits. But this would only be of help if the possibility of performing medical exams, such as laboratory tests (including kidney function tests and levels of immunosuppressants), at an institution located nearby the patient’s home, would become a reality. The availability of home-use devices allowing analysis of these parameters may be a reality in the future and would be of much help for the transplant community.20
Another measure, necessary to put in action the approach of longdistance virtual follow-up, would be the possibility of delivery of medication at the community pharmacy, in a patient’s nearby health institution or even at patients’ homes. Although some Portuguese Hospitals are already performing the first or the last of these measures, these are not yet the general way of providing the specialized medication to the kidney transplant recipients.
As a final statement I can say that there is no doubt that kidney transplantation is the most sustainable modality for stage 5 chronic kidney disease treatment. It is worth noting that it can become even more sustainable, if measures that facilitate the assessment and follow-up of transplant candidates and kidney transplant recipients in a more convenient way, both to patients and their clinicians, are implemented.
These include the use of telemedicine, conducting medical exams and medication delivery in a nearby place of patients’ homes. In order to become a reality, a dialogue between the health care professionals that are committed to kidney transplantation, hospitals boards of directors and health authorities are needed. In my view, the Portuguese Society of Transplantation and patients’ associations should also be involved in such a project.















