INTRODUCTION
Healthcare facilities are one of the most polluting facilities worldwide.1,2 In particular, Nephrology, mostly due to hemodialysis (HD), is one of the most polluting medical areas. Thus, healthcare professionals should contemplate innovative ways of achieving more sustainable HD provision and kidney care delivery.3
HD, when initiated, is most often performed in a standard prescription of 4-hour treatments thrice weekly, regardless of patient’s residual kidney function (RKF).4 Incremental hemodialysis (iHD) has gained attention due to the possibility of personalizing kidney care by adapting the treatment to the RKF. This might have several clinical advantages such as preservation of both RFK and vascular access4,5and increasing patients’ quality of life. Accelerated RKF loss with more intensive dialysis might reflect glomerular hypoperfusion.4-6 Fewer vascular access punctures might lead to longer preservation of the vascular access but there is no robust study comparing vascular access outcomes with twice versus thrice weekly treatments.7 It also brings additional benefits such as mental health management since it allows patients to become familiar with the treatment and gradually adapt to the new reality.
Beyond the clinical benefits, by decreasing the number of sessions while the patient still has RKF, this regimen might also be more environmentally friendly and more economical. The aim of this study was to evaluate the potential reduction of resource consumption, waste generation and carbon footprint and its savings associated with the implementation of an iHD program.
METHODS
We conducted a 1-year retrospective single-center study including all incidental HD adult patients in our centre in 2019 (pre-pandemic), that underwent conventional HD. Patients were divided in two groups according to their potential eligibility for the iHD program.
- iHD group: those that would have been eligible to iHD at our center.
- Standard group: those that would not have met the criteria for our iHD program.
All the patients included in the study were receiving treatment in a hospital hemodialysis unit with 15 beds, using either the AK 200 Ultra or the Artis Physio machines.
Differences among groups were calculated for 12 months. This timing was based on previous literature, including randomized clinical trials, that showed high rates of persistence on iHD at one year.8,9 CO2 equivalent (CO2-eq) emissions related to transportation to and from hospital HD sessions were calculated through ViaMichelin website,10 using the models of the ambulances affiliated to our hospital as a reference.
Waste generation and carbon footprint related to HD treatment (table 1) were calculated based on published data from our center.2
Table 1 Cost and waste generation in our facilities, on average, per HD treatment per patient2,4,11,12.
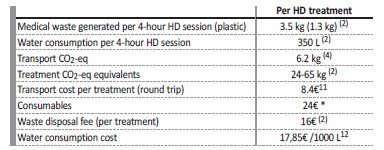
* unpublished data, from our center
iHD protocol
Criteria to be included and to remain in iHD program was interdialytic weight gain of less than 2.5 kg or 4% of the patient’s dry weight. The exclusion criteria were persistent hyperkalemia (K>5.5 mmol/L) and/or hyperphosphatemia (P>5 mg/dL) resistant to medical therapy, symptomatic hypotension during HD sessions or uncontrolled hypervolemia and/or hypertension.
RESULTS
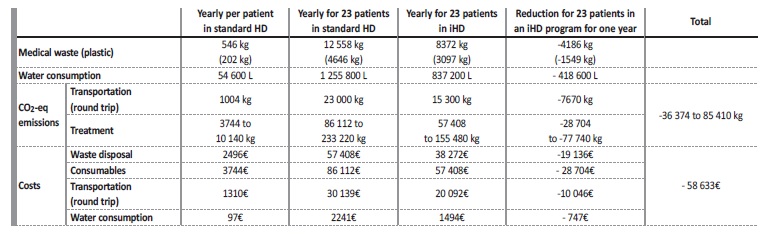
The study included 157 patients. Twenty-three patients (15%) would have been eligible for iHD (iHD group) and 134 (85%) would have remained on a standard HD prescription (standard group). The implementation of an iHD program, in our unit, would have resulted in a decrease of 4186 kg of waste per year, with 1549 kg of that being plastic waste. The associated waste disposal fee of 16€ per session would have resulted in savings of 19 136€ per year.
The water footprint of HD is also a matter of concern since it is estimated that each 4-hour HD session requires 350 L of water. Implementation of iHD would have reduced water consumption in 18 200 L/patient/year, or 418 600 L for the 23 patients that would have been included in the iHD group. The estimated cost savings for the hospital would have been 747€ per year, based on the fixed water price for the city in 2019.
This program would also mean, in our unit, the potential to achieve an annual reduction of 36 to 85 tons of CO2-eq emissions. Most of the CO2-eq emissions are related to materials and logistics of the treatment, with only up to 21% of the calculated CO2-eq emissions attributable to transports to HD sessions.
Overall, our center would have attained annual cost savings of almost 60 000€ with this program, with the most important contributors being the waste disposal fee and the consumables, accounting for almost 80% of the costs’ reduction. The consumables used during the treatment represent an expenditure of about 24€ per session per patient, totalizing around 3744€ spent in a year for only one patient.
Thus, if this program had been implemented this would represent a cost reduction of 28 704€. For the cost savings, we also took into consideration the water consumption, which was previously mentioned, and the transport costs, which would represent a cost reduction of 260€/patient/year. If all the eligible patients had been enrolled, 10 046€ in transport would have been saved in one year. If the program was adopted on a larger scale, the potential environmental and economic benefits would be substantial (table 2). For every 1000 patients under iHD for a year, we estimate that water consumption could be reduced by 18.2 million liters, medical waste production by 182 tons, CO2 equivalents by 3.7 million tons, and generate savings of 2.5 million euros. Scaling up the program would result in notable resource conservation and economic efficiency.
DISCUSSION
Up to our knowledge, our study was the first to evaluate the environmental impact of an iHD program in Portugal. Our results show that 15% of the incidental HD patients would have been eligible to begin HD with an iHD program.
iHD implementation in our unit would have reduced 36 to 85 tons of CO2-eq emissions and more than 4 tons in waste yearly, of which 1.5 tons is plastic.
An estimated 58% of continental Portugal’s territory is vulnerable to desertification,13 thus water-saving measures are warranted. In terms of water consumption, we would have been able to save 418.600 L in a year and cut money spendings in 60 000€ in one year. This amount could further contribute to the green transition in our hospital.
To better distribute iHD patients throughout the week and still maintaining the appropriate intervals between HD sessions, patients could be allocated as follows: Monday-Thursday, Tuesday-Friday and Wednesday-Saturday, allowing to dialysate 3 patients/slot with only one HD machine5 and also allowing for na easier human resources’
In terms of transport costs, we have only considered the price of the fuel and did not consider the human resources’ cost. Thus, cost saving should be higher than our projection.
HD’s carbonic footprint goes beyond medical waste handling. In this study, we did not incorporate the environmental impact of production and supply chain of drugs and HD consumables.
Another limitation was that electricity consumption was not included in the calculation of the carbon footprint. We do not have data about the indirect impact of the energy source (i.e. renewable energy sources). It represents a significant limitation, as electricity generation is a major contributor to greenhouse gas emissions. As a result, the study’s findings may underestimate the true environmental impact of adopting an iHD program. Further research is required to address this limitation and provide a more comprehensive assessment of the ecological footprint. This study has also not considered the impact on patients’ absenteeism in the workplace.
Due to the retrospective nature of the data, we cannot ensure these 23 patients would have been able to be maintained in an iHD program throughout 12 months.
CONCLUSION
Kidney care poses a growing challenge to the sustainability of medical care. The increasing prevalence of patients with kidney disease put further pressure on the system. Innovative ways to cut energy and water consumption, CO2-eq emissions and costs are warranted.
Beyond several clinical advantages and the opportunity to put into practice patient-centered medicine, our study shows that iHD significantly attenuates the environmental and economic impact of HD. iHD program implementation must follow a healthcare Provider strategy and must adhere to strictly outlined inclusion and maintenance criteria. These findings should encourage physicians to think greener while never conditioning the clinical decision of referencing a patient to iHD.
Prospective studies are needed to evaluate the real environmental and financial impact of an iHD program, where other areas associated with the ecological footprint of HD should also be considered.