INTRODUCTION
Autologous arteriovenous fistulas (AVF) are the preferred vascular access for patients requiring hemodialysis treatment. When planning AVF, distal fistulas, mostly radiocephalic fistulas (RC-AVF), have demonstrated the lowest complications and longer patency rates, requiring less interventions.1-3 In selected patients, where a distal AVF is intended, anastomosis of the radial artery with the basilic vein of the forearm, at the wrist, may be an option.
The authors present a case report of a RC-AVF with drainage problems that was recovered using the forearm basilic vein.
CASE REPORT
We describe a case of a 60-year-old male with end-stage renal disease secondary to IgA nephropathy. A history of arterial hypertension, coronary artery bypass grafting with saphenous vein, and prosthetic mechanical aortic valve replacement was reported. Chronic medication included vitamin K antagonists. He referred angor in the months prior to AVF creation. Cardiology deferred cardiac catheterization until dialysis initiation. A RC-AVF with side-to-end anastomosis was created on his left arm in June 2018. In the preoperative evaluation, the radial pulse was present, the Allen test was negative and ultrasound examination detected vascular calcification of the radial artery. Three days later, he was admitted to the Intensive Care Coronary Unit with unstable angina. He underwent coronary artery stenting; upon discharge, haemodialysis with na internal jugular vein tunnelled catheter was initiated. The fistula was cannulated in August 2018. The patient reported tolerable hand pain during dialysis and grade II steal syndrome was noticed. The physical examination revealed a present radial pulse. The ultrasound evaluation detected an anastomotic connection of 4.1 mm and a flow of 800 mL/min in the brachial artery. Access monitoring and surveillance were decided.
In September 2018, we detected a venous stenosis. A thrill and a hyperpulsatile pulse in the draining vein the RC-AVF (forearm cephalic vein) until the elbow were noticed. The ultrasound evaluation found that the median cephalic vein had morphological and hemodynamic significant stenosis at the junction of the middle third with the upper third of the forearm. The brachial artery flow was 350 mL/min., with a resistance index of 0.6. The patient underwent successful endovascular angioplasty. Although well tolerated, this further increased the hand access-induced distal ischaemia (HAIDI), with inconstant pain at rest.
In November 2018, the patient exhibited venous cannulation problems and a relapse of the venous stenosis was observed. Physical examination and ultrasound assessment were like those described in the evaluation carried out in September. The dialysis unit decided not to intervene, due to the risk of worsening the HAIDI. This also posed an important limitation when considering the step to proximal AVF construction. By this time, the patient was extremely resistant to additional AVF intervention and a tunnelled central venous cateter (CVC) was placed.
The patient was referred to our vascular access center, in August 2019, to reassess the AVF patency. A thrill and a hyperpulsatile pulse in the draining vein, up to the middle third of the forearm were noticed.
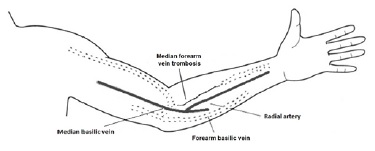
Ultrasound evaluation showed a long and occlusive stenosis at the proximal third of the median cephalic vein of the forearm, and the patency of AVF was maintained preferentially through collaterals of the forearm basilic vein (Fig. 1). The brachial artery flow rate was 400 mL/min, with a resistance index of 0.6.
As the stenosis was not suitable for endovascular angioplasty, the group decided to proceed with surgical repair. The forearm basilic vein with a diameter superior to 5 mm was dissected and rotated toward the median forearm vein, already arterialized due to the RCAVF, and a side-to-end anastomosis was created (Fig. 2). The RC-AVF outflow was directed through the median forearm vein into the forearm basilic vein, which in turn drains into the basilic vein of the arm.
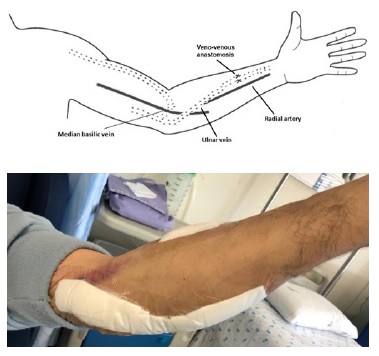
Figure 2: Radiocephalic fistula with rotation of the forearm basilic vein toward the median forearm cephalic vein
After this approach, in ultrasound assessment, the brachial artery flow was 1000 mL/min. The patient started double cannulation, one month later, without major complications. No significant steal syndrome was reported. The drainage vein maintained a length of 20 cm. Rope-ladder cannulation technique was applied and the tunnelled CVC was removed.
Six months after the surgery, the fistula had significantly prolonged haemostasis. The ultrasound revealed a morphological and hemodynamic stenosis with 2.8 mm diameter at the elbow level, corresponding to the forearm basilic vein anastomosis (used to recover the fistula).
A brachial artery flow of 550 mL/min was present. Endovascular angioplasty of the stenosis was performed, and the fistula was successfully cannulated on the day after the intervention.
No further complications were reported in the follow-up period, and the fistula currently remains functional, with a secondary patency (post-intervention cumulative patency) of 32 months.
DISCUSSION
RC-AVF remains the closest to the “ideal access”. The malfunction of an AVF due to thrombosis or stenosis is not a reason for discarding the access when endovascular treatment is not an option. It is very important to analyse the vascular network with ultrasound, to identify veins that can be used to solve the access dysfunction.
We report a case of a patient with cardiovascular comorbidities and ischemic complication, possibly induced by recent construction of an RC-AVF. The RC-AVF presented stenosis of the median vein of the forearm, and it was decided to use the forearm basilic vein as outflow.
Endovascular intervention may be a good option to solve this problem, with or without stent placement. On ultrasound examination, the long stenosis had echogenic characteristics compatible with nonrecent occlusion. This situation precludes endovascular angioplasty. We decided to rotate the forearm basilic vein to drain the AVF.
The use of an arteriovenous graft was also considered, but this option is associated with an increased risk of complications such as infection and thrombosis,4 and requires two anastomoses; such anastomoses are future points for stenosis.
The use of the forearm basilic vein is not a usual procedure, with the literature suggesting the use of this technique in only approximately 1.5% of all fistulas created.5 In 2018, Norton de Matos et al6 reported their experience and presented three cases of construction of distal AVF, with outflow into the forearm basilic vein, through rotation of the forearm basilic vein toward the cephalic vein in the forearm.
The authors suggested that this procedure is appropriate when the forearm basilic vein has a diameter ≥4.0 mm and can be rotated towards the forearm cephalic vein.
In our case, the option allowed the patient to keep a functional RC-AVF and withdraw the CVC, avoiding all the associated complications and improving the quality of haemodialysis. On the other hand, this surgical technique enables arterialization of the arm basilic vein and facilitates its future transposition in a single step.
Moreover, the creation of a fistula in other sites, namely a proximal AVF, was delayed. Proximal AVF have a higher flow rate than RC-AVF7-10 and therefore leads to a greater risk of cardiovascular complications and may worsen the HAIDI syndrome.
Our patient’s fistula had a post-treatment primary patency of 6 months and a secondary patency of 32 months. This outcome was previously reported in similar AVF. In a review published in 2018, the post-treatment primary patency ranged between 5 and 18 months, and the secondary patency between 20 and 60 months.6
Besides the importance of having a distal AVF, it is of major importance that dialysis staff develop strategies to optimize cannulation. In this type of access, it is essential to identify the site of veno-venous anastomosis (forearm basilic vein with cephalic vein), avoid cannulate, in order to delay future stenosis.6,11In our case, we identified the site where the veno-venous anastomosis (forearm basilic vein with cephalic vein) was carried out and flagged it to prevent it from being cannulated.
Monitoring and surveillance programmes should be implemented by the dialysis unit for early recognition and treatment of vascular access dysfunction, resulting in increased patency rates.1-3 We considered important to fulfil a systematic assessment (every two months) of the flow of the fistula with ultrasound, in addition to the physical exam on a regular basis.
CONCLUSION
Although the experience with the use of the forearm basilic vein as outflow of the RC-AVF is still limited, this surgery has proven to be a good option when the forearm basilic vein has an appropriate diameter and allows the rotation toward the cephalic vein. This procedure allows the recovery of the fistula without the use of the upper arm veins and avoids the placement of a CVC.
We believe that this approach could be used more often to salvage RC-AVF with outflow occlusion, maintaining a functional access, in selected patients.