INTRODUCTION
Since the first reports of a pneumonia caused by the novel coronavírus (SARS-CoV-2) in December 2019, COVID-19 has achieved global proportions in a short and unprecedented period, with over 650 million cases recorded globally and more than 6.6 million fatalities. Until the end of 2021, different waves of illnesses followed the introduction of new genetic variants that shared a similar pathogenicity and mortality risk. From 2022, however, due to the higher transmissibility, the new variants became predominant, as was observed with the Omicron emergence more recently, which has higher transmissibility than the previous ones. On the other hand, despite being related to a skyrocketing number of cases, the Omicron variant was not associated with a high hospitalization rate and fatality, mainly because of the vaccination coverage observed in some countries. In the first two years, the COVID-19 epidemiological characteristics in Brazil seemed to be similar to what was observed in several countries, but almost 10% of death in the globe occurred in our country.
FIRST MEASURES TO COPE WITH THE COVID-19 PANDEMIC AT HOSPITAL DO RIM, BRAZIL
Hospital do Rim is a health center in the Brazilian state of São Paulo. With an estimated population of 45 million inhabitants, São Paulo is the most populous state in the country, with 19 million people living in the metropolitan region of the capital, São Paulo city. Hospital do Rim, founded in 1998, is a tertiary care institution specialized in kidney transplantation. Over the preceding decade, the hospital performed over 1,000 procedures each year, accounting for 20% of all kidney transplants conducted in Brazil. As of 2020, there were over 10 000 kidney transplant recipients (KTRs) in follow-up and approximately 9000 patients on the waiting list.
Early in January 2020, we initiated an active mobilization plan to disseminate to health professionals and institution patients as much trustworthy information on COVID-19 as possible, with an emphasis on individual protective actions. Since March 2020, we have adopted the use of N95 mask for all healthcare practitioners and hospitalized patients. We also assured the supply of diagnostic tests and medical equipment, and planned access control measures to the assistance units. In the next steps, we organized the telehealth department and carried out the vaccination strategy for all collaborators and patients.1
Thanks to the active cooperation of the Brazilian Association of Organ Transplantation, the National System of Transplantation, and the local transplant regulatory center, several initiatives were made to keep the Brazilian transplant program alive. First, in a strategic decision, the Hospital do Rim was preserved as a COVID-19-free hospital in order to respond to transplantation needs not only for the State of São Paulo, but also for all other regions where the transplantation moratorium was declared due to an increasing number of COVID-19 patients requiring hospitalization.1 Furthermore, there was unprecedented academic community engagement in developing research in several areas of interest, as well as in our center, in order to address multiple issues concerning the influence of COVID-19 among KTRs.
THE IMPACT ON THE NUMBER OF DECEASED DONORS
In Brazil, the rate of deceased donors was 14.2 per million people in 2014, which gradually increased, reaching 18.1 in 2019. With the COVID-19 breakthrough, the rate of deceased donors was reduced by 20%, reaching 15.8 between 2020 and 2021. After the peak wave provoked by the Omicron variant between January and April 2022, the donors’ rate had an additional reduction to 12.1, mainly because of the number of potential donors diagnosed with COVID-19. For instance, in the Organ Procurement Organizations coordinated by Hospital do Rim, in the period of original and first variants predominance, only 68 of 1394 donors (5%) had a positive COVID-19 test, while after the Omicron predominance, this number raised to 20% (36 in 176 donors). Despite being associated with a low fatality, Omicron posed several difficulties to organ transplant programs, with a high impact on the number of potential deceased donors. Of note, from March 2022, the National recommendations were updated to allow the utilization of donors with a positive SARS-CoV-2 test under straight safety criteria.
THE IMPACT ON THE NUMBER OF KIDNEY TRANSPLANTS
Between 2011 and 2019, the number of kidney transplants increased by more than 20% in Brazil, reaching 6296 transplants in 2019. Between 2020 and 2021, this rate decreased by 24%, with 4750 kidney transplants in 2021 and an additional impact in the first 2022 months because of the number of Omicron variant-infected potential donors. Besides the reduction in deceased donors, the impact on the number of living donor transplants was higher, plummeting 56% from 1077 to 581 between 2019 and 2021. Depending on the epidemiological situation, several centers declared the total interruption of the transplantation with living donors, justified by the elective nature of this modality, protecting donors from potential harm, as well as the recipients, postponing the surgery to periods when the COVID-19 number of cases was lower, which was observed after the protection derived from the spreading vaccination. In our center, living donor transplantations were completely interrupted between April and May 2020, from when there was a gradual resumption from June, reaching normalization in October of the same year.
Many Brazilians States joined in sustaining the country’s transplantation program as possible. However, due to the pandemic migratory pattern and the continental characteristic of our country, the impact
on the health systems was different among the States.2 Thus, when the transplants could not be performed in a State, the organs were transferred to another that sustained the transplantation. Furthermore, as the Hospital do Rim was dedicated to kidney transplants and considering the strategical decision to be a COVID-19-free health center, which had a central role in keeping the viability of the national transplantation program by the national cooperation for organ allocation and distribution between States, most organs could be engrafted, reducing the potential for discard. Until March 2022, the Hospital do Rim received organs from 23 of 27 States in Brazil, totaling 838 kidneys, from which 616 (73%) were transplanted in our center, 114 (14%) were transplanted for other teams, and 108 (13%) were discharged. Therefore, we worked as a hub to allocate organs distributed from other States when the diferente stages impacted the health system during the pandemic breakthrough.
Furthermore, besides the organ utilization improvement, the Hospital do Rim performed transplants for patients referenced from other hospitals, consequently sustaining the number of transplants higher than in other countries.
THE IMPACT ON THE KIDNEY TRANSPLANT RECIPIENTS HEALTH
In our center, the first case of COVID-19 was diagnosed in March 2020. From then, the number of cases raised in the following weeks, reaching a plateau in the epidemiological week number 44 in 2021.
The plateau shape persisted during the predominance of the original SARS-CoV-2 (February 2020 to March 2021), Beta (August 2020 to January 2021), Gama (January 2021 to August 2021), and Delta (July 2021 to February 2022), which was similar in the general Brazilian population. Thus, among 10 341 KTRs followed in our center, 2269 patients were diagnosed with COVID-19 between March 2020 and
December 2021. With the Omicron emergence and predominance, between December 2021 and April 2022, 1235 new infections were diagnosed, representing 35% of all cases since the pandemic began two years before (Table 1).
Table 1: Distribution of COVID-19 cases and outcomes by the virus genetic variant predominance among kidney transplant recipients at the Hospital do Rim, Brazil
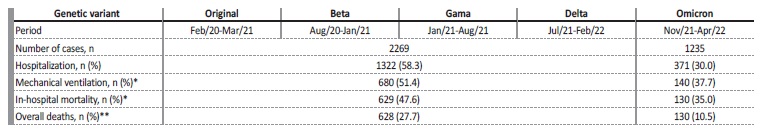
Footnote: the period is estimated according to the predominance in the Brazilian general population.
* among the hospitalized patients
** considering all patients diagnosed with COVID-19
Contrarily the number of cases, the fatality rate was constant at almost 27% between the first 2269 cases, independently of the pandemic phase and the vaccination coverage.3 After the Omicron, the fatality reduced to 10.5% among the 1235 subsequent patients. Similar differences were observed in the intermediate outcomes between pre- and post-Omicron predominance: hospitalization rate from 58% to 30, and among in-hospital patients, the mechanical ventilation requirement rates from 51% to 38%, and death from 47.6% to 35.0% (Table 1).
In additional action, our center matrixed the efforts for COVID-19 diagnosis in Ipaussu, a city in the countryside of São Paulo with 14,506 inhabitants. We adopted the same criteria to test people in both populations: for inhabitants in the Ipaussu city, and KTRs in the Hospital do Rim. The weekly number of cases in the Ipaussu city was similar to what was observed in Hospital do Rim, with total cases of 2486 in the pre-Omicron predominance, with a peak of 156 cases in a week. After the Omicron, the weekly cases peak increased more than twice, reaching 375 cases in a week, totaling 1680 cases.
Despite the similar number of cases, we observed disparities in the fatality rates, including in the Omicron predominance. Among the first 2468 diagnosed patients in the Ipaussu city in the pre-Omicron period, there were 48 deaths (1.9% vs 27.6%, compared with KTRs), while in the Omicron predominance period, there were only 8 deaths in 1680 patients (0.5% vs 10.5%), all of them high risk or non vaccinated patients.
In addition, we also compared the age-adjusted risk of death among KTRs followed at our center with people living in the State of São Paulo. Among people aged 20 and 30 years, a range with a low rate of comorbidities, the fatality among the KTRs was 23-fold higher (8.5% vs 0.37%), underscoring the prolonged immunosuppressive exposure as a determinant role in the severity for transplanted patients.3
THE RESPONSE TO THE VACCINATION
In the Hospital do Rim, we carried out a phase IV trial to evaluate the 28-day seroconversion rate among kidney transplantation using CoronaVac, an inactivated whole-virion vaccine. After the first and second shots, the seroconversion rates were 15.2% and 43%, respectively.4 Furthermore, we extended the trial to offer a third homologous dose for patients who were IgG anti-SARS-CoV-2 negative after two doses. In those patients, the serological response was only 20.3%. In another study, we enrolled patients who had received two CoronaVac doses, and the seroconversion rate was compared between patients who received a third homologous dose with those who received a third heterologous mRNA BNT262b2 dose. We observed a higher seroconversion rate for patients in the heterologous group (49% vs 32%), which reached a higher seroprevalence at the end of the study (67% vs 55%).5
CONCLUSION
The COVID-19 pandemic posed a dramatic reduction in the number of transplants, but the concepts of transplantation were not impaired, and the transplant activity resisted in our center and country. Compared with the general population, the fatality rate among KTRs was 10-fold higher, underscoring the impact of the immunosuppressive exposure and the cumulative number of comorbidities in the negative results among COVID-19 patients. Finally, the immune response to all vaccines for KTRs was limited, demonstrating the requirement for extra doses for those patients. Looking back on the first two years of this unprecedented global health threat, we concluded that coordinating efforts to keep the transplant activity in the country with the largest public transplantation system was a correct decision to sustain the soul of the transplantation.