INTRODUCTION
Currently, kidney transplantation faces challenges related not only to the growing prevalence of end-stage kidney disease (ESKD) but also to the aging of the population. It is the best therapeutic option for selected patients with ESKD, with proven benefits in mortality and quality of life. However, elderly ESKD patients are more disadvantaged by their medical complications and lower predicted post-transplant survival, which makes their access to transplantation still limited.1 Living kidney donation, including from older living donors, provides benefits for all transplant candidates, and, especially for older ones, can be the only chance to get transplanted.2 Although older age is not a contraindication for donation, the acceptance remains controversial due to the high incidence of comorbidities, greater risk of surgical complications in the donor, and possible lower graft survival in the recipient.1,2
We report a case of living kidney transplantation between an older donor and recipient, both over 70 years old, who evolved to a stage 3 chronic kidney disease (CKD), without proteinuria, hypertension, or other complications in the post-transplant period.
CASE REPORT
A 71-year-old Caucasian female with CKD secondary to autosomal dominant polycystic kidney disease underwent a living kidney transplant from her older sister in 2018. The patient was on a regular hemodialysis program for 14 months and she had a personal relevant history of right hemicolectomy for a colon malignancy (T3, N0, Mx, R0) over six years ago, with no signs of recurrence at the time of transplantation. There was no need for chemo or radiotherapy. She also had a history of chronic gastritis and dyslipidemia. As sensitizing events she had two pregnancies and transfusion of red cell concentrates in the postoperative period of hemicolectomy (calculated panel reactive antibody (PRAc): 0%). The candidate was submitted to a right nephrectomy two months before transplantation, without complications.
The living donor was her older sister, a 76-year-old Caucasian female, without kidney disease, hypertension, diabetes mellitus, cancer history, or other comorbidities that would contraindicate donation.
The pre-donation urinalysis revealed no erythrocyturia (red blood cells 0-2/high power field) and insignificant proteinuria was confirmed by 24 hours urine analysis (130 mg/24h). The abdominal and pelvic computerized tomography excluded polycystic disease, showing “kidneys in usual topography, normal dimensions and morphology with smooth contour”. The pre-donation cystatin-C (cyst-C) was 1.06 mg/L and serum creatinine (SCr) was 0.93 mg/dL (estimated glomerular filtration rate (eGFR) calculated by CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) creatinine-cystatin C (creat/cyst) equation of 67 mL/min/1.73 m2). DTPA technetium-99 renogram showed a left kidney differential function of 46.8% (24.3 mL/nn) and a right kidney differential function of 53.2% (27.7 mL/nn). The risk of ESKD pre-donation calculated by ESRD Risk Tool for Kidney Donor Candidates was 0.06%.
A living donor kidney transplant was scheduled. It was a haploidentical transplant (4 mismatches at HLA A, B, C e DR), without donorspecific antibodies. The flow cytometry and complement-dependent cytotoxicity crossmatch were negative. The induction immunosuppression was performed with basiliximab 20 mg (at day 0 and day 4 after transplantation), tacrolimus 0.1 mg/kg/day, mycophenolate mofetil 1000 mg twice a day, and methylprednisolone 500 mg. The left kidney was implanted in the right iliac fossa and warm ischemia time was three minutes and thirty-four seconds. Pre-implantation kidney biopsy was not performed. The surgery was uneventful and the patient evolved with immediate diuresis. She was discharged eight days after transplantation with an SCr of 1.86 mg/dL (eGFR CKD-EPI: 29 mL/min/1.73 m2). There were no major complications in the posttransplant period, namely infections, acute rejections, or hospitalizations related to kidney graft, and no biopsy was performed during the follow-up period.
Three years later, the recipient evolved to stage 3a CKD (eGFR CKD-EPI creat/cyst: 46 mL/min/1.73 m2; SCr: 1.04 mg/dL; cyst-C: 1.59 mg/L), without proteinuria, arterial hypertension, overweight or diabetes. The donor evolved to a stage 3b CKD (eGFR CKD-EPI creat/cyst: 47 mL/min/1.73 m2; SCr: 1.29 mg/dL; cyst-C: 1.32 mg/L), also without proteinuria, hypertension, overweight or diabetes (Fig. 1).
Discussion: Along with the general population, patients with ESKD are aging and the fastest-growing group worldwide is over 65 years old.3,4Even in these patients, several studies have shown that kidney transplantation is the best therapeutic option.5 In selected candidates, it offers a better survival and significantly improves the quality of life, compared to the time spent in dialysis.3,5-8 However, the management of these patients is complex, and many nephrologists remain reluctant to register elderly patients on waiting list for kidney transplantation.3 They usually have several comorbidities which may complicate the postoperative course and increase the risk of ESKD. In addition, the widening gap between the organ supply and demand makes the access of elderly patients to transplantation even more difficult.9
To enlarge the number of available organs the donor criteria have expanded to non-heart-beating donors, dual kidney transplantation and elderly donors (living and deceased), allowing the use of kidneys that would be wasted before.5,9,10 The kidneys from older living donors are progressively being used for transplantation, reflected by the increase in the number of living donors over 60 years during the last decade.1 Even though, the use of kidneys from older living donors remains controversial in many centers. There are concerns about recipients’ graft and global survival and donor’s long-term risk after donation, associated with age-related decline in kidney function.5,9
In Portugal, from December 2011 to December 2019, 532 living donor kidney transplants were performed. The average age was 54.3±10.3 years for donors and 47.0±14.0 years for recipients. Among donors aged ≥60 years (n=170; 31.9%), only 38 (7.1%) were aged ≥70 years. Regarding recipients, 109 (20.5%) were aged ≥60 years, of which 27 (5.1%) were aged ≥70 years. The Kidney Transplantation Unit from Santo António’s Hospital, in Porto, contributed to 43% (n=223) of living kidney transplants performed in this period. Overall,5 donors and 3 recipients were aged ≥70 years and, in addition to the reported case, there was only one more case of elderly living kidney transplantation in the Unit.
We report a case of a successful kidney transplant between na older living donor and recipient, both over 70 years old, with no complications, either surgical or in the post-transplantation period. Both evolved to a stage 3 CKD, without proteinuria or hypertension. During the follow-up period, there were no episodes of rejection or other graft-related complications.
The superior outcomes for recipients of living kidney donors compared to deceased donors were demonstrated in previous research.11
However, the benefits of using older living ones remain less clear, given the increased risk of ESKD and graft failure among recipients, already reported in some studies.12,13
The surgical procedure is relatively safe. The mortality estimated rate is low and a longitudinal study, during a 15-year follow-up period, showed no increased mortality risk after living kidney donation compared to age and comorbidity-matched individuals from the general population.14 Limited data are available regarding living donors older than 70 years, but there is evidence showing that nephrectomy is safe and associates with a recovery and survival post-donation similar to younger donors.15
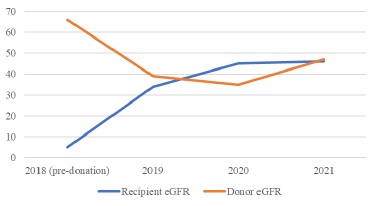
Figure 1 eGFR evolution in the donor and recipient before donation and in the first 3 years post-transplant (eGFR calculated by the CKD-EPI creat/cyst equation)
Acceptance of a potential living donor is often subjective. Absolute and relative contraindications to living donation vary greatly across transplant centers.9 Several risk factors with impact on long-term allograft outcome have been proposed, like donor and recipient age and gender, acute rejection episodes, HLA mismatch, ABO incompatibility, and functional renal mass.5 However, the parameter that seems to affect more significantly the allograft survival in living donor kidney transplantation is the age difference between donor and recipient.5
When this difference increases, the graft survival rate gets worse. Even though, more than age itself, donor kidney function, their comorbidities, and overall health should be the more important factos deciding if an older living donor should be accepted or not.9
The risk of rejection is increased when kidneys from elderly donors are transplanted into younger recipients, however, in older-to-older kidney transplantation, this risk seems to be attenuated, possibly because of the immunosenescence.8,16-18 More than fear of rejections, the main concern in using older living donors for kidney transplantation is the possibility of a greater progressive decline in donor and recipient kidney function, associated with age-related renal senescence.4 The eGFR in a healthy population remains stable until aged around 40 years and then declines each decade at a rate of 6.6 mL/min/1.73 m2 for men and 7.7 mL/min/1.73 m2 in women.19 According to the British Transplantation Society guidelines for Living Donor Kidney Transplantation (2018), the advisory threshold eGFR considered acceptable for a 75-year-old living donor female is 54 mL/min/1.73 m2.19 A safe threshold level of pre-donation kidney function allows sufficient function after donation to maintain the donor in normal health, or minimal absolute reduction of health, without impairinglifetime.19
Based on cohort studies, ESKD in living donors is a rare event - ranges from 0.2% to 0.6%, similar to that of the general population - and occurs in a median of 20 years after donation.1,20 Living donors with normal age and gender-specific kidney function before donation, as demonstrated in our clinical case, are at no greater risk of ESKD than the general population.20
After nephrectomy there is a sudden loss of approximately 50% of the nephron mass, corresponding to an eGFR decrease. However, the remaining healthy renal parenchyma is capable of restoring some lost function and, in short term, there is a recovery of 70% of the pre-donation eGFR.1,21 Recovery in the older donor is expected to be lower, even so, Velosa et al evaluated 140 living donors (105 were <35 years and 35 were >55 years old) and showed that post-donation percentage change of eGFR was similar in both groups (68±8 and 65±8 in younger and older groups, respectively).22 Generally, outcomes are acceptable among carefully selected older living donors and studies are showing no difference between death and cardiovascular disease compared to healthy nondonors.23 Even though, it is important to ensure that donors are extensively evaluated and properly informed about the potential risks of donation. Although it is a relatively safe procedure with limited long-term risks, they must recognize that lifetime risks are real and, in some cases, may be difficult to predict.9
Regarding the recipients, it was already demonstrated that decreased graft function of the donor does not reflect a worse patient or graft survival. Berger et al24 found no significant differences in short-term graft failure or recipient survival of living donors 70 years or older when comparing these patients to recipients of 50- to 59-yearold deceased donors. Conversely, Gill et al25 found similar graft failure for recipients from living donors aged 55 to 64 years compared to deceased donors less than 55 years old. More recent research reinforced previous reports, showing favorable outcomes of older living donors, when compared to standard and expanded criteria deceased donors.2 Although recipients from living donors 70 years or older had significantly increased graft failure, the overall survival was not worse, probably due to decreased time spent on dialysis.2
In carefully selected elderly candidates, kidney transplantation can restore autonomy, physical and mental well-being to enjoy life and fulfill ambitions that would otherwise be difficult to achieve. This way, they will feel more motivated to better preserve the graft’s function and their overall health.7 In general, several studies are supporting older living transplantation as an acceptable alternative to avoid dialysis, offering better survival, favorable long-term outcomes, and qualityof- life benefits.2,4-7
Our clinical case supports the already proven benefits of older kidney transplantation. The careful selection of the donor, the short time spent on dialysis, and the little age difference between donor and recipient probably contributed to the favorable outcomes verified.
It is important to enhance that older age is not a contraindication for living kidney donation and in carefully selected patients it can offer better survival and quality of life to recipients, without significantly harming donor’s long-term kidney function.














