CLINICAL ASPECTS
A patient must have irreversible kidney failure in order to receive a KT (kidney transplantation). However, not every ESKD patient is a suitable KT candidate and a thorough evaluation must be conducted. Each patient has to undergo a detailed assessment of medical and surgical issues, psychosocial factors, social support availability, financial viability and physical and cognitive abilities to balance the benefits and risks of KT and long-term immunosuppression.1 The criteria to be a candidate are heterogeneous when transplant centers around the world are compared, and many patients fall into a gray area where they are neither definitively eligible nor ineligible.2 Further, there is the matter of potential living donor evaluation, which is the main focus of this article and which demands a whole other set of prerequisites.
With that in mind, the KDIGO (Kidney Disease: Improving Global Outcomes) work group has created guidelines with recommendations in order to establish a more uniform process leading up to the actual KT procedure.3 The guidelines state that transplant programs should, whenever possible, provide customized quantitative estimates of short-term and long-term risks from donation; that each donor candidate should undergo a biopsychosocial evaluation and that it is essential to formulate a donor care plan that includes longterm follow-up.
In Portugal, the need for a structured kidney replacement therapy options plan has been institutionally advocated (DGS Norma nº 017/2011), including renal transplantation, but the actual implementation of such a pathway lags behind, due to many barriers, including lack of effective communication with the patient. A task force on living donor transplantation should be prioritized.
It is known that living donor kidney transplantation (LDKT) is associated with superior patient and graft survival, earlier access to transplant, and improved quality of life when compared with deceased donor KT.1 Furthermore, there are also confirmed benefits to preemptive transplantation, in which KT occurs before commencing dialysis.4 As opposed to cadaver KT, preemptive KT leads to fewer pretransplant blood transfusions, less employment loss, improved long-term graft survival, lower rates of delayed graft function, and fewer episodes of acute rejection, in addition to allowing for greater flexibility in regards to timing.5 In order to decrease patients’ waitlist time and identify a living donor, transplant education should begin as early as CKD stage 3.6 Notwithstanding, there appears to be a mismatch between the value of preemptive KT and its actual use, with undesirable geographical heterogeneity in its access, as expressed by our national registry, and this underlines the importance of creating a task force whose goal is to increase not only LDKT rates, but also preemptive KT rates.4
MEDICINE AND SOCIETY: FROM THEORY TO PRACTICE
Honoring the motto “transplant first” while simultaneously having recognized the lack of high quality, efficient information about KT and all it entails, it made sense to try to create something that could act as a concrete step in the right direction. As such, we developed a website (transplanterenal.icbas.up.pt) (Figure 1) as a tool of promoting literacy and transforming an academic work (an MsC in Medicine) into the effective diffusion of knowledge with social impact. We aimed to create an easily accessible way to educate the population about kidney transplantation, with accurate data explained in a way anyone - from patients to their families and potential donors - could understand.
The website provides, among other things, information about what it takes to receive a KT, the requirements to become a donor, some useful contacts and current statistics, and even testimonies from previous patients. The ultimate goal when designing this modern tool was to improve access to KT, namely preemptive LDKT, thus tackling a lack of health literacy - one of the main barriers identified - and increasing transplant rates, to move towards achieving the potential benefits of investing in this choice of treatment for patients with ESKD.
Contrary to popular belief, patients prefer to start this discussion at an earlier phase of their disease, thus having more time to learn about transplantation, finding a living donor, completing the required evaluation steps and eventually getting on a KT waitlist. Additionally, donor quality of life is at least equal to that of the general population, and often returns to pre-donation levels after the procedure.7 Recognizing the existing barriers associated with KT, with multilevel expression that includes the patient, the healthcare provider and the system itself is the first step on a long road to their resolution (Figure 2). We view education and accessibility as the pillars to achieve real improvements in the short term and, thus, as the main focal points to invest in, going forward. (Figure 3)
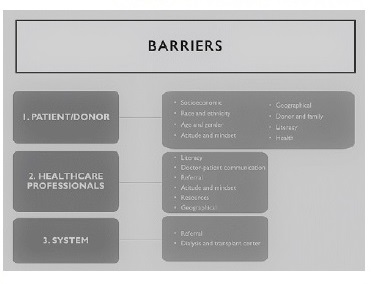
Figure 2 Summary of identified barriers in transplantation-first policies (complementary discussion available from https://repositorio-aberto.up.pt/handle/10216/134691)
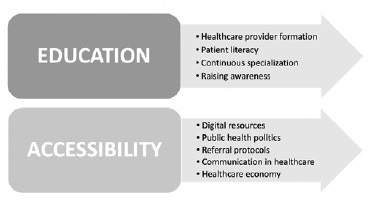
Figure 3 Plan of action and process of intervention (complementary discussion available from https://repositorio-aberto.up.pt/handle/10216/134691)
Clinicians need education as well as time and resources to progresso towards a transplantation-first policy. A general approach to those barriers and recommendations to overcome them are summarized (Figures 2 and 3), as a detailed discussion can be accessed in the content of the thesis referred to.
Considering literacy, it is vital that patients and their families get the opportunity to consider KT as a potential treatment in a timely manner, procuring education through reliable culturally and demographically conscient sources, using simple and straight-forward language.
In addition, it is of extreme importance that they have healthy, communicative relationships with their healthcare providers and, whenever possible, multidisciplinary teams, in which they feel the safety and confidence to inquire about and explore this option realistically. Between 2015 and 2020, the median waiting time for a deceased donor transplant was 4.8 years. In contrast, the same statistic regarding living donor transplants was 0.8 years, which shows the importance of investing in LDKT to improve patient outcomes. Globally, Portugal has some of the highest percentages of deceased donor transplants, but also of patients requiring RRT. In 2019, 514 kidney transplants were completed, translating to a total of 49.9 transplants per million population (pmp). However, among those, only 75 (14.6%) were from living donors. Over the last 10 years, Centro Hospitalar e Universitário do Porto (CHUP) performed close to 50% of all LDKTs in Portugal, with nearly one third of those part of the living donor program.
In 2020, due to COVID-19 pandemic, there was a decrease of 21% of the global transplant activity in the country. By the end of 2020, we recorded 24.7 deceased donors pmp, 9.1 fewer donors pmp than in 2019. Organ donation after uncontrolled circulatory death (Category II of the Maastricht classification) saw the most visible impact, with 60% fewer donors than the previous year.
Living donor transplantation decreased about 45% (from 75 to 41 transplants) to 4.02 living donors ppm. The programs were suspended March through May 2020, and for the rest of the year, the number of living donor transplants remained at lower levels. It can be explained by logistical issues, seeing as it is an elective surgery, as well as due to professional and patient fear of the increased risk of infection. The referral to living donor consultation has also decreased substantially and some potential donors declined donation during pandemics. One patient underwent ABOi transplant and 6 patients were transplanted in kidney paired transplant program, one of them included in the South Alliance for Transplant, an exchange between CHUPorto and Fundació Puigvert.
Notwithstanding, at the end of 2020, the waiting list for transplant decreased slightly to 1951 patients, probably related to increased death rates on the waiting list (http://ipst.pt/files/TRANSPLANTACAO/DOACAOETRANSPLANTACAO/DadosAnuais_AtividadeDoacaoTransplantacao2020_atualizado.pdf). So far, in June 2021, CHUP has performed approximately 50 KTs, of which 11 were LDKT and 2 were kidneypancreas transplants. There has been a steady recuperation of transplantation rates, particularly of LDKTs, but there is a need to improve the process of patient and donor referral, effective communication between the hospitals, and implementation of best practices.8
The strategy of investing in communication and continuous education between nephrology departments, transplantation and dialysis units, converging as a whole in a task force promoting living donor renal transplantation, must not be overlooked. This task should be performed by all the stakeholders in the nephrology system, preferably reinforced by the Ministry of Health, by including the percentage of preemptive kidney transplantation and live donor transplantation as a quality indicator and benchmarking of the hospitals with transplantation programs, supporting allocated resources.
Only when healthcare professionals are at their best can they allow their patients to reach the best possible outcomes. It is our hope that, this thesis makes a positive and meaningful contribution to the ongoing efforts of creating a future where KT is the first line of treatment for ESKD, and where patients achieve higher survival rates and quality of life.
















