Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.28 no.1 Lisboa mar. 2014
ORIGINAL ARTICLE
Alternative vascular access for haemodialysis – a single centre experience in transhepatic and intracardiac catheters
Acessos vasculares alternativos para hemodiálise – a experiência de um centro em cateteres trans-hepáticos e intracardíacos
Francisca Barros1, Berta Carvalho1, Raquel Vaz1, Patrícia Martins1, Ricardo Neto1, Manuel Pestana1
1 Department of Nephrology, Centro Hospitalar São João. Porto, Portugal.
ABSTRACT
Introduction: Vascular access for haemodialysis represents a major problem for patients undergoing this technique. The construction of fistulas or grafts is not always feasible, and a central venous catheter remains as the sole option. Exhaustion of the common sites for central venous catheters placement is common, which sometimes leads to new life-saving approaches. Methods: We retrospectively reviewed the charts of four patients who underwent intracardiac or transhepatic dialysis catheter placement in our clinic between January 2003 and November 2010. Two patients received an intracardiac catheter, one patient received a percutaneous transhepatic catheter and one patient had initially a transhepatic catheter followed by an intracardiac catheter when dysfunction of the former developed. Overall, five intracardiac and four transhepatic catheters were placed. Results: In our patients, when the first procedure was placement of intracardiac catheter the access average survival was 36 months (24–48 months), compared to the use of transhepatic catheters as first approach, with an access survival of 1.75 months (0.5–3 months) for the latter. The two patients who underwent intracardiac catheter replacement died in the post-operative period. Two transhepatic catheters needed replacement, and average catheter survival was 13 months (2 -24 months). Discussion: Our results provide evidence that these techniques can be considered as a last option for patients with exhaustion of vascular access and unsuitable for peritoneal dialysis or kidney transplantation.
Key-words: Haemodialysis; intracardiac catheter; transhepatic catheter; vascular access.
RESUMO
Introdução: A manutenção do acesso vascular para hemodiálise representa um problema importante para os doentes submetidos a esta técnica. A construção de fístulas ou enxertos nem sempre é possível e muitas vezes o doente permanece com cateter venoso central como acesso definitivo. A exaustão frequente dos locais comuns para colocação de cateteres venosos centrais condiciona a procura de abordagens venosas inovadoras para manter a continuidade da técnica. Métodos: Foram revistos retrospetivamente os processos de 4 doentes submetidos a colocação de cateteres de diálise trans-hepáticos e intracardíacos no Hospital de São João entre Janeiro de 2003 e Novembro de 2010. Dois doentes colocaram cateteres intracardíacos, um doente colocou um cateter trans-hepático e um doente colocou inicialmente um cateter trans-hepático seguido de colocação de cateter intracardíaco. Resultados: Foi obtida uma sobrevida média do acesso de 36 meses (24 – 48 meses) quando o primeiro procedimento foi a colocação de cateter intracardíaco, comparativamente com uma sobrevida média de 1.75 meses (0.5 – 3 meses) quando se optou pela colocação inicial de um cateter trans -hepático. Os doentes que efetuaram substituição de cateter intracardíaco acabaram por falecer no período pós -operatório. Foram efetuadas duas substituições de cateteres trans -hepáticos, sendo a sobrevida média do acesso 13 meses (2 – 24 meses). Foram colocados um total de cinco cateteres intracardíacos e quatro trans-hepáticos. Discussão: Os resultados obtidos evidenciam que o uso de cateteres intracardíacos e trans -hepáticos pode ser considerado como última alternativa em doentes com exaustão de acessos vasculares que não são candidatos a diálise peritoneal ou transplante renal.
Palavras-chave: Acesso vascular; cateter intracardíaco; cateter trans-hepático; hemodiálise.
INTRODUCTION
Although current guidelines advise against the use of central venous catheters (CVC)1, the construction of arterio-venous (AV) fistulas and grafts is not always possible and many patients must chronically remain with tunnelled CVC. These patients who undergo catheter -dependent haemodialysis (HD) may exhaust traditional sites of catheter placement, which becomes a major problem. Multiple alternative access sites were already reported (for HD and other treatments requiring tunnelled catheters) including tunneled catheters in collateral neck veins2,3, translumbar inferior vena cava (3,4), transhepatic3,5,6, renal veins7 and intracardiac8 -11.
MATERIALS AND METHODS
We retrospectively reviewed the charts of four patients with multiple venous access failure who had intracardiac or transhepatic dialysis catheter placement in our clinic, between January 2003 and November 2010, representing the experience of our department in alternative vascular access. In a total of 1621 long--term dialysis catheters that were placed in our unit in the mentioned period, five intracardiac and four transhepatic catheters were introduced. Due to the failure of common vascular accesses, two patients received an intracardiac catheter, one patient received a percutaneous transhepatic catheter and one patient had initially a transhepatic catheter followed by an intracardiac catheter when dysfunction of the former developed.
RESULTS
Patient 1
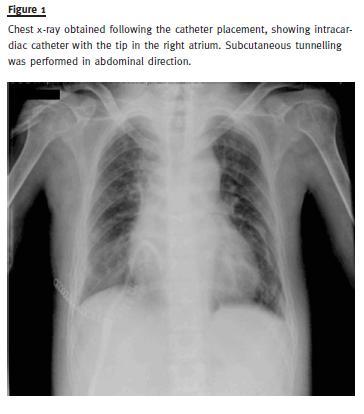
A forty-three year-old male patient with marked intellectual disability and obstructive chronic kidney disease (CKD) had been on HD treatment since the age of 27. The kidney transplantation and peritoneal dialysis teams refused him as a candidate to these treatment modalities. He had multiple vascular accesses including AV fistula, AV grafts and short and long term CVCs with multiple failures due to thrombosis and infection. As a consequence of this, he developed thrombosis of the superior and inferior cava vein, documented by angiography. In December 2006, fourteen years after the beginning of HD, a MedComp Ash Split Cath® catheter was introduced, through antero-lateral thoracotomy in the right atrium (Fig. 1). This catheter allowed good dialytic efficiency, with an eKt/V of 1.6. The patient had two CVC-related infections. No microorganism was isolated in either episode, and both were empirically treated with vancomycin and gentamicin, with no need for catheter removal. The patient died 24 months after insertion of the intra-atrial catheter in the context of major trauma (fall with hip fracture), with a functioning CVC.
A thirty - five year - old female patient, with CKD secondary to chronic pyelonephritis due to congenital sacral myelomeningocele had been on HD treatment since the age of 20.
During the first few years on HD, the patient had 5 AV fistulas and multiple CVC. When she was 26, a bilateral thrombosis of the subclavian-brachiocephalic venous arch was documented by angiography. One year later, the patient was considered to have no condition for further conventional vascular access construction, neither an AV fistula nor graft. She started PD aged 27, but shortly after developed ultrafiltration failure and diffuse peritoneal sclerosis.
She returned to HD through a femoral tunneled catheter. Renal transplant was tried at this point, missed by marked hypoplasia of the iliac vessels.
The most relevant causes of coagulopathy, including genetic disorders, were excluded. At the age of 28, catheter dysfunction was noticed and the CVC removed. Because angiography showed bilateral femoral vein thrombosis, an inferior cava vein catheter was placed under surgery. The catheter was used for ten months. In January 2003, due to the failure of this catheter with partial inferior cava vein thrombosis, she was purposed to an intracardiac CVC. She was submitted to right antero - lateral thoracotomy with insertion of a dual lumen MedComp Ash Split -Cath® catheter in the right atrium. With this access, a spKt/V of 1.9 was achieved. Multiple catheter associated infections occurred, mostly without agent isolation, and were treated empirically with vancomycin and gentamicin. Forty - eight months later, due to rupture with significant bleeding, this catheter was again replaced under thoracotomy. This catheter was persistently dysfunctional. The patients death occurred two weeks later due to procedure-related septic shock.
Patient 3
A fifty-five year-old female patient with Bardet-Biedl syndrome and diabetic nephropathy developed end -stage renal disease and begun HD at the age of 48, through an AV fistula.
Six years later, she presented exhaustion of common veins to insert catheters: she was proposed to peritoneal dialysis but was not accepted due to co -therapist absence. She was considered unsuitable for kidney transplantation.
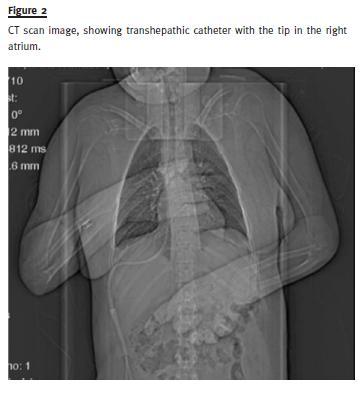
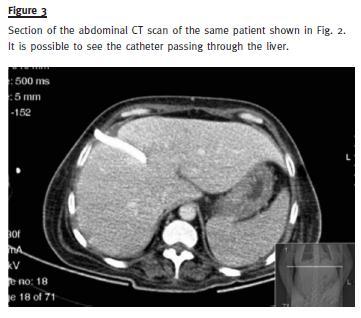
At this time, a transhepatic procedure was thought as rescue access. In July 2007, a Pourchez –Retro Spire Biomedical® haemodialysis catheter was placed, through percutaneous punction of the supra–hepatic vein under ultrasound control, with right atrium catheterization and insertion of HD catheter, with the extremities intra -auricular. Two weeks later, the patient developed migration of the catheter in the peritoneal space, with haemoperitoneum. The patient underwent transhepatic catheter replacement by a similar procedure (Figs.2 and 3).
During the twenty -four month period of the use of this catheter, good dialytic efficiency was achieved (eKt/V 1.9). Multiple infections (2–3/year) associated with CVC occurred, mainly due to Staphylococcus epidermidis and hominis, which were treated with vancomycin and gentamicin.
The patient died aged 57, two years after the insertion of the transhepatic catheter, due to fatal sepsis of unknown origin (infected venous ulcers Vs CVC).
Patient 4
A fifty-nine year-old male patient, with CKD due to autosomal dominant polycystic kidney disease, started HD at the age of fifty -five through a jugular venous catheter. In the following years, the patient had multiple AV fistulas, grafts and CVC with sustained failed attempts to find an access. Three years later, he was dialyzing through a femoral catheter, which developed chronic infection and finally thrombosis in spite of chronic hypocoagulation.
Due to exhaustion of common vascular access, in March 2007, a transhepatic route was considered, and a Pourchez -Retro Spire Biomedical® catheter was placed by percutaneous punction of the supra-hepatic vein. After three months, a chronic infection of the catheter tunnel due to Pseudomonas aeruginosalead to catheter replacement over a guided wire with construction of a new tunnel. Progressive dysfunction of the catheter in the two following months was identified.
Another transhepatic replacement was not considered at that point, and a transthoracic approach was decided as the best option. An antero-lateral thoracotomy for insertion of a Pourchez -Retro Spire Biomedical® catheter was performed. Following a short period of catheter malfunction with the need of fibrinolysis, a good dialytic efficiency was obtained, with average of eKT/V of 1.85. During the 36 months that followed, there were several catheter infections, predominantly associated with Pseudomonas aeruginosa (treated with oral ciprofloxacin).
Finally, he developed chronic infection with methicillin -resistant Staphylococcus aureus, which evolved to sepsis in spite of vancomycin and daptomycin treatment. In the end of 2010, it was decided to replace the catheter by thoracothomy.
The procedure was complicated by haemopericardium and cardiogenic shock and, two days later, an exploratory thoracotomy was done with a second CVC replacement, but it remained dysfunctional. Peritoneal dialysis was tried as rescue, but it proved useless because of displacement of the peritoneal catheter and infection. The patient died one month after admission due to uncontrolled septic shock with multi -organ dysfunction.
DISCUSSION
In patients who underwent multiple previous CVC placements, vascular access for haemodialysis can be challenging.
In cases of exhaustion of all traditional forms of vascular access, CVC placement using a transhepatic route has been used more frequently in the last few years and good outcomes have been described with this technique. As an example, Smith and Ryan5 report their series where sixteen patients submitted to a total of 21 transhepatic catheter placement, with a mean total access site service of 138 catheter days.
Younes and colleagues6, describe their experience with the use of 127 transhepatic catheters for dialysis, in 22 patients. Although technical success was admitted in all cases, there still were 105 replacements in 14 patients, with a mean of 7.5 exchanges. Both reports emphasized that transhepatic catheters are a functioning option, although associated with long-term maintenance problems. Prolonged use of intracardiac catheter for dialysis was described for the first time, in 1999, by Chavanon et al.8. The following years, this approach was described in a few case reports. Their advantage seems to be related to the ability to function despite thrombosis or stenosis of the central venous system. Agrawal and collegues reported, in 2009, two cases of intracardiac catheters10, one of which with the need of multiple replacements and a longest duration of primary patency of 4 years. A report of 27 patients with intracardiac catheter11 showed that 81.5% of the cases were successfully haemodialyzed via intracardiac permanent catheters during the mean follow-up time of 27.5 ± 14.8 months.
We are reporting on a group of patients who started haemodialysis in the 1990s. At that time, fluoroscopy was not available in our unit as a resource to help an early diagnosis of subclinical vascular stenosis, in the context of central venous catheter placement. Furthermore, the lack of policies for a maximum saving of vascular territory available at that time, probably resulted in a vessel wastage that could be presently spared with premature use of angiography in CVC dysfunction.
This can explain our patients loss of vascular territory and our need to find alternative vascular access in this young group.
In our group of patients, we achieved a better catheter and patient outcome with intracardiac versus transhepatic catheters (Table I).
When the first procedure was placement of intracardiac catheter, access average survival was better, of 36 months (24–48 months), compared to the use of transhepatic catheters as first approach, with access survival of 1.75 months (0.5–3 months) for the latter.
In our centre the two patients that underwent intracardiac catheter replacement died in the post-operative period. Our experience with replacement of transhepatic catheters was more successful, in line with the description in the literature, and proved that it is possible to maintain a second transhepatic catheter for as long as 24 months with an average catheter survival of 13 months (2–24 months).
Our results, together with other reported rare cases6,7, provide evidence that these techniques can be considered as a last option for patients with exhaustion of vascular access and unsuitable for peritoneal dialysis or kidney transplantation.
References
1. III. NKF -K/DOQI. Clinical Practice Guidelines for Vascular Access: update 2000. Am J Kidney Dis 2001;37(Suppl 1):S137 -S181. [ Links ]
2. Funaki B, Zaleski GX, Leef JA, Lorenz JN, Van Ha T, Rosenblum JD. Radiologic placement of tunneled hemodialysis cateter in occluded neck, chest, or small thyrocervical collateral veins in central venous occlusion. Radiology 2001;21:472 -476. [ Links ]
3. Weeks SM. Unconventional venous access. Tech Vasc Interv Radiol 2002;5(2):114-120 [ Links ]
4. Lund GB, Trerotola SO, Scheel PJ Jr. Percutaneous translumbar inferior vena cava cannulation for hemodialysis. Am J Kidney Dis 1995;25(5):732 -737. [ Links ]
5. Smith TP, Ryan JM, Reddan DN. Transhepatic catheter access for hemodyalisis. Radiology 2004;232(1):246-251. [ Links ]
6. Younes HK, Pettigrew CD, Anaya-Ayala JE, et al. Transhepatic hemodialysis catheters: functional outcome and comparison between early and late failure. J Vasc Interv Radiol 2011;22(2):183-191 [ Links ]
7. Murthy R, Arbabzadeh M, Lund G, Richard H 3rd, Levitin A, Stainken B. Percutaneous transrenal hemodialysis insertion. J Vasc Interv Radiol 2002;13(10):1043-1046. [ Links ]
8. Chavanon O, Maurizi -Balzan J, Chavanis N, Morel B, Blin D. Successful prolonged use of an intracardiac catheter for dialysis. Nephrol Dial Transplant 1999;14(8):2015 -2016. [ Links ]
9. Santos-Araújo C, Casanova J, Carvalho B, Pestana M. Prolonged used of an intracardiac catheter for dialysis in a patient with multiple venous access failure. Neprol Dial Transplant 2006;21(9):2670-2671. [ Links ]
10. Agrawal S, Alaly JR, Misra M. Intracardiac access for hemodialysis: A case series. Hemodial Int 2009;13(Suppl 1):S18–S23 [ Links ]
11. Oguz E, Ozturk P, Erkul S, Calkavur T. Right intra-atrial catheter placement for hemodialysis in patients with multiple venous failure. Hemodial Int 2012;16(2):306–309 [ Links ]
Drª Francisca Barros
Department of Nephrology, Centro Hospitalar São João
Alameda Prof. Hernâni Monteiro
4200 – 319 Porto
Portugal
E-mail: mfranciscabarros@gmail.com
Conflict of interest statement: None declared.
Received for publication: 31/10/2013
Accepted in revised form: 04/02/2014














