I. Introduction
The link between urban development and well-being, happiness, and quality of life, between physical space and health, between the city and public space and the advantages and disadvantages of their use, is an old discussion that has gained new momentum in the last three decades, by the exponential increase of urban problems and the need to with them. Urban planners and policymakers show haste to implement a myriad of actions for requalification and environmental valorisation, urban rehabilitation, revitalisation and regenerative public spaces, integrated strategies and processes for the reconciliation between people and places, increase places connectivity, promote compactness, fight sprawl, improve urban green areas and integrate nature in cities, upgrade waterfronts and soft transport modes (cycling and walking) to fight car use and private transport, among other initiatives.
While this urban development aimed to cope with urban problems and meet the needs of its citizens, leverage the quality of life, and promote health and well-being, there is “grey” literature highlighting the pros and cons of the urban environment and urban living style. Indeed, urban development outcomes have proven to be positive, fostering people’s general well-being and quality of life, but also harmful by affecting people’s health and well-being (European Commission [EC] et al., 2019), significantly burdening states’ finances and impacting the public economy. Then, to reduce uncertainty within urban development outcomes, there is an urgent need to build evidence on how and how much the urban environment people live in work, and spend time in, affects their health and well-being. Although the challenge has been stressed through the years, there is insufficient research to provide evidence-based knowledge.
Moreover, according to the United Nations (UN) population prospects, not only world population is increasing at an astonishing rate, but the urban population is projected to increase at an even higher rate. Indeed, the number of urban dwellers has been progressively increasing and, already in 2022, the UN reiterates that “six out of every ten people in the world are expected to reside in urban areas by 2030, rising to 83% by 2050.” (United Nations Human Settlements Programme [UN-Habitat], 2022, p. 9).
Therefore, it is impossible to dissociate the dynamics of world population growth from emerging phenomena and challenges such as climate change and climate action, the continued use and consumption of fossil fuels, the necessary decarbonisation of the planet, geopolitical issues and their impacts on human life, people’s health, and its socio-cultural dimension.
Taking mental health as a component of health that was (especially before the pandemic) often less considered, the existing knowledge is mainly empirical through a few studies correlating urban design with health issues and health benefits. However, there is still no evidence that mental health concerns are considered in the current urban planning processes/methodologies. One of the positive side effects of the pandemic is that it drew people’s attention to important issues, such as the mental health effects of the built environment, that until now were not correctly recognised. Another relevant issue raised through the pandemic was the importance of scientific knowledge for policymakers to support decisions. The ‘scientification’ of public policies during pandemic outbreaks was highly reported and impacted collective awareness of the importance of science with societal impact. In the scope of this scientific chain value, the need to have metrics for evaluation and benchmarking was stressed in different forums involving academics and politicians. In this realm, urban health determinants to measure, evaluate and classify the impact of urban space on the mental health of citizens were at the core of the discussion worldwide.
In this context, geography plays a key role, as many parameters mentioned in the literature are geographical-based, e.g. landscape (land use and land cover, topography, accessibility, connectivity, diversity, buildings, houses, etc.), the socio-economic structure of the population (age, gender, purchase power, education, etc.), the configuration of urban space, the cultural heritage, the climate and environmental factors (air quality, noise, temperature, relative humidity, wind, etc.), the health indicators (people diagnosed with a specific type of diseases; a daily dose of medication; access to health care facilities), and lifestyle indicators (drugs and alcohol consumption indicators, sports activity, etc.); the territory overall organisation (facilities, infrastructures, mobility, etc.), among others, that have a direct either-or indirect influence on people’s health and mental well-being.
The analysis of physical space and its relationship with health has a long history in architecture, interiors, work, and residence spaces (Higuera-Trujillo et al., 2021). However, research on the relationship between human health and the urban built environment is still at an early stage. In ‘Neurourbanism: towards a new discipline’ (Adli et al., 2017), the lack of close and effective interaction between urban planners and health professionals is evident, considering several studies that point to the increase in mental disorders such as anxiety, stress, depression, and other emotional disorders in urban environments (Peen et al., 2010). Thus, it is considered that neurourbanism is a new field that explores the neuroscience and the biological underpinnings of mental states and disorders to ensure a better quality of life in urban areas (Ancora et al., 2022; McCay et al., 2017; Pykett et al., 2020).
Even before the pandemic, several global institutions identified the need to study the urban context and the quality of life (also from the perspective of individual health), of which the UN and the European Union (EU) stand out. The UN-Habitat and the World Health Organization (WHO) have demonstrated that mental health has been at the heart of their policy research and work for several decades (WHO, 1998, 2001, 2010). Moreover, more recently, the EU, in its strategic investment fighting against imbalances and inequities, launched programmes and funding lines dedicated to promoting health in cities. As an example of such funding policies to foster research on the topic, we can highlight the eMOTIONAL project Cities, a research & innovation actions (RIA) project supported by the EU Horizon 2020 programme. Under this call, the European Commission (EC) supports five more projects worth 30 million euros total, which, together, constitute the Urban Health Cluster (UHC), the first European cluster to improve and safeguard the health and well-being of citizens, leaving none behind. Promoting and maintaining mental health and well-being and reducing mental illness risk factors are pivotal to achieving urban sustainability and building healthier, resilient, and human-centred cities and communities.
This article attempts to raise awareness of the importance of urban planning and urban design as a technical and political tool for preparedness for the emergent challenges cities and Humanity face and to guarantee people’s mental health and well-being. The article is organised in four parts. The first part discusses on public spaces realm of public health and summarises its conceptual evolution, drawing on the findings on the relations between the built environment and health, and more specifically, mental health; the second part of this article is dedicated to discussing the concept of urban health, mental health and urban stressors to shed light on the impact of an urbanite in people’s health and well-being; the third part is divided on the discussion of the determinants of urban health based on the extensive narrative on the topic, and ends with a summarised table of the built environments determinants and its adverse impacts on mental health; the fourth and last part it is dedicated to final remarks.
II. Public space as the collective living room
The history of a city is the history of its public space (Borja & Muxi, 2003) because it is where all social and political activities are printed and the place of all discussions and decisions that affect the collective. In this regard, public spaces demand thinking and design, e.g., the outline, the matter, the form, as well as the banal urban features citizens use daily for interaction with the environment, to enjoy, or to express themselves through social and artistic manifestations or simply the most careless use of crossing and permanence.
The understanding of the ‘public space’ concept varies. There are those who understand it as a set of voids, as a space that mediates volumes, as small ‘leftovers’ that must be filled up, and others who do not understand them and therefore do not place them at the forefront of planning and making cities. However, public space is the place that promotes socialisation and, as such, is a fundamental space to combat social isolation and the mental health problems that often result from it. Public spaces encompass publicly owned or designated for public use, where everyone can freely access and enjoy them without making a profit (UN-HABITAT, 2016).
In the scope of this article, public places are considered to be the most visible, collective, accessible and common spaces of the city. This vision of public space has gained increased importance in recent decades, and it is also the one that contributes to the satisfaction of different quality of life criteria, even when the “death” of public space, according to Remesar, has been announced. Despite this, municipalities persist in investing in public space as an area constantly expanding, resulting from changes in mobility and transportation infrastructures. The design and maintenance of streets have become a significant challenge for local authorities, who must find ways to harness the symbolic power of public spaces, as they have always done.
In the late 1960s of the 20th century, Jan Gehl “transformed” Copenhagen into a “laboratory city” for several studies on the interaction between public space and public life, intending to understand this interaction, testing different methods and analysing the resulting patterns. More recently, the Gehl Institute and the Robert Wood Johnson Foundation have developed an ‘Inclusive Healthy Places (IHP) Framework’ (Gardner et al., 2018) as a data-driven tool dedicated to people in the assumption of bridging health equity gaps in public space. Understanding Community Context; Support Inclusion in Process; Design and Program Public Space for Health Equity; and Foster Social Resilience are the four principles for creating healthy and inclusive places.
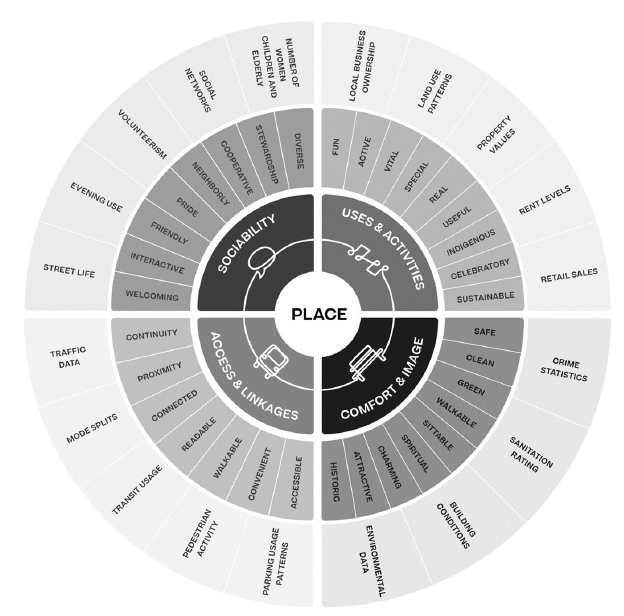
Another example that underlines the importance of the public space regarding its impact on general well-being is the American ‘Project for Public Spaces’, started in 1975, as one of the first attempts to systematise what makes a Great Place based on a set and sub-set of principles (fig. 1). The systematisation has a form of a wheel with three layers from the centre to the edge of the wheel, where in the centre there are four main principles-dimensions: 1) sociability, 2) uses and activities, 3) access and connections, and 4) comfort and image, each one of them sub-divided into attributes in a second layer, and finally the third layer with the identification of the parameters, which should guide an urban intervention that comes closer to citizens’ needs. The importance of current health promotion through public spaces and outreach relationships has guided the ‘Project for Public Spaces’ to achieve partnerships with companies and foundations that provide funding, technical assistance, and capacity building to local organisations. In this way, it is possible to ensure that more people have access to public spaces with community power as if they were collective living rooms.
Public civic space is not a residual space between streets and buildings. Nor is it an empty space considered public simply for legal reasons. Nor is it a “specialised” space, to which one has to go like someone who goes to a museum or a show. Rather, these spaces are potential public spaces, but something more is needed for them to be public civic spaces. (Borja & Muxi, 2003, p. 15)
Through public space, solutions were tailored to each era’s flavours of time, and some of those solutions still inspire many current interventions. Here are some of the cities labels or buzzwords of the epoch: ‘Garden’ (Howard, 1898), ‘Soft’ (Raban, 1974), ‘Sustainable’, from the diffusion of the term ‘sustainable development’ (Keeble, 1988), ‘Global’ (Sassen, 1991), ‘Smart’ (Deakin & Al Waer, 2011), ‘Innovative’, ‘Resilient’, ‘Equitable’, the ‘15 minute’ (Moreno et al., 2021) or the five, ten, or twenty-minute cities or ‘neighbourhoods’, depending on the scales and the means of mobility.
From ‘ecocities’ (Register, 1987) to ‘healthy cities’ or ‘healthy communities’, which, for the first time, puts health and urban design together in the perspective of understanding and mitigating the stress on human health. The WHO ‘Healthy Cities and Villages’ initiative in 1986 brought the importance of the topic to public health policies. They produced the first international agreement in this context, the Ottawa Charter for Health Promotion, more than 30 years ago, the cornerstone document for public health promotion.
Public spaces make up between two and 15% of land in city centres in Europe. Both their physical and social functions are essential and can relieve some of the pressures exerted on a city by a growing population. (...) In future cities, we will need to optimise the distribution and use of public space to ensure that it is safe, accessible, and inclusive for all. (EC et al., 2019, p. 92)
III. Health(s): the human, the urban and the mental
1. Health
It is in the preamble to the Constitution of the World Health Organization - “(…) adopted by the International Health Conference held in New York from 19 June to 22 July 1946, signed on 22 July 1946 by the representatives of 61 States (…), and entered into force on 7 April 1948” - that the notion of ‘Health’ is defined and comes to the present day, incorporating the revisions that follow.
The States Parties to this Constitution declare, in conformity with the Charter of the United Nations, that the following principles are basic to the happiness, harmonious relations and security of all peoples: Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. (WHO, 1946, p. 1)
This definition expresses “(...) that there is much more to health than simply a collection of negatives - a state of not suffering from any designated undesirable condition.” (Evans & Stoddart, 1990, p. 1347). Several circumstances influence human health: the personal characteristics of each and environmental factors, be they social, economic, or physical. These factors - health determinants - are defined by WHO as “the range of behavioural, biological, socio-economic, and environmental factors which influence the health status of individuals or populations” (WHO, 2021, p. 4).
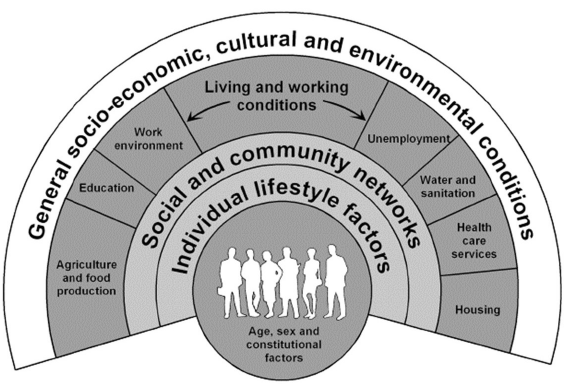
Whitehead and Dahlgren’s ‘rainbow model of the determinants of health’ has become an iconic illustration of the significant groups of determinants, adopted by WHO and adapted by several authors, referring, from the inside out: 1) age, sex, and hereditary factors; 2) individual lifestyle factors; 3) social and community networks; 4) living and working conditions; and 5) general socio-economic, cultural and environmental conditions (Dahlgren & Whitehead, 1991). The weight represented by each of these determinants is variable and has been the subject of study in recent decades. The Health Mission states that biological and genetic factors and health behaviours affect health up to 25%. In contrast, factors of the social and physical environment and the health service account for 75% (Health Mission, 2017).
In an article that takes as reference the ‘County Health Rankings Framework’ (Stiefel et al., 2020), what is inherent to human conditions is confined to the personal socio-economic context (which represents the importance of 40%) and behaviour (where genetic and acquired issues can be included) which represent 30%; what depends on externalities includes access to healthcare (20%) and the built environment which represents, for this proposal, the shortest slice of this influence (10%).
The concepts of health exist along a continuum without distinct boundaries; however, this does not preclude us from acknowledging their distinctions. Various concepts are neither correct nor incorrect; they serve different purposes and have different areas of applicability. Regardless of the level of health definition employed, it is crucial to differentiate it from the issue of determining the factors that contribute to that definition of health (Marmor, 1989).
2. Urban Health
The urban health concept, accordingly, to one of the definitions of WHO’s development, includes ‘urban governance’, ‘population characteristics’, ‘the natural and built environment’, ‘the social and economic environment’, ‘food quality’ and ‘emergency health services and management’ as factors contributing positively or negatively to urban health, but also about individual health within the urban context.
For example, in developing countries, the best urban governance can help produce 75 years or more of life expectancy. With poor urban governance, life expectancy can be as low as 35 years. (…) While most of these root causes lie beyond the direct control of the health sector, local leaders have direct influence over a wide range of urban health determinants, from housing and transport policies to social services, to smoking regulations and the policies that govern food marketing and sales. (WHO, 2010, p. 5)
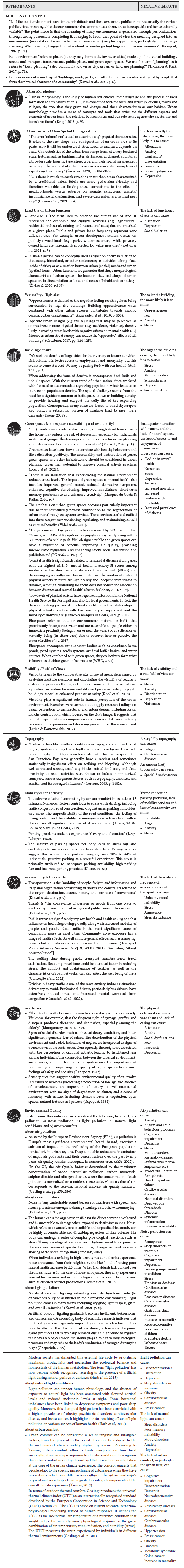
Therefore, it is critical to identify and reorganise, upfront, the determinants that go beyond human health or the “health of cities” and are not restricted to social ones (social health determinants), on which there has been focusing most of the research on the topic in recent decades. Moreover, it is essential to mention that the proposal of determinants presented here (fig. 3) correlates the built environment with both physical and mental health, as they are inseparable. Indeed, urban health reflects the impact of the physical and social environment on the quality of life and well-being of individuals and communities living in urban areas. The physical and built environment, including urban structures, infrastructure, and spaces, can significantly affect health, mainly when issues such as water quality or air pollution arise. On the other hand, the urban environment can also contribute positively to health through the presence of open, green, and recreational spaces (Michalos, 2014).
3. Mental Health
The built environment can influence physical and mental health in both favourable and unfavourable ways, emphasising the significance of purposeful planning and policy initiatives incorporating a health perspective. Mental health is a complex matter with no single cause but is shaped by numerous factors that can affect an individual’s mental well-being (Van Winckle et al., 2022). According to the WHO, “Mental health is a state of well-being in which an individual realises his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community” (WHO, 2019, p. 1). In this regard, emphasising the community value, David Sim highlights the role of everyday places and proximity where urban interventions can flesh out social relationships and communities. In David Sim’s words, “Neighbourhood is not a place. Neighbourhood is a state of mind.” (Hamilton, T. & Tucker, N., 2022, 00’20’’).
Moreover, to underline the high importance of promoting mental health and global well-being, the report ‘The Future of Cities’ (EC et al., 2019) cites Hayes et al. (2015) to assert that severe mental disorders are a primary contributor to global disability, leading to an average lifespan that is 10-20 years shorter than that of the general population. According to the report above, the United Nations has calculated that a significant proportion of individuals with mental illness in low-income countries, up to 75%, do not have access to proper care. In high-income countries, this percentage still varies between 35% and 50%. The Organisation for Economic Co-operation and Development (OECD/EU) refers that mental health issues affect approximately 84 million individuals throughout the European Union, and the associated costs, both direct and indirect, are considerable (OECD/EU, 2018). In response, many European countries are adopting comprehensive policies that promote mental health and raise awareness.
4. Urban stress cuts across physical and mental health
Stress is a transversal problem that aggregates various organic and psychological disorders caused by diversified stimuli such as physical, emotional, and living conditions, among others. Stress, therefore, affects physical health and mental health. Belonging to the social domain, according to Koene, the study of stress has great scientific relevance to the extent that it is researched from social, psychological, or medical perspectives (Koene, 2018a). According to the same author, “Urban stress is stress in humans, caused by the urban environment” (Koene, 2018b, p. 3).
Although stress and mental disorders occur mainly in urban environments, the physical and spatial causes have not yet been adequately associated (Lederbogen et al., 2011; Malta & Marques da Costa, 2021)), at least at the time of reference. However, due to the increasing number of articles that have been published on the topic most recently, there are reasons to believe that will change and soon, more than build evidence on associations between the urbanite and stress and mental disorders, causality is on the way. From this interdisciplinary research endeavour, guidelines to integrate urban planning and public health policies will foster mental health and prevent or reduce mental illness.
Regarding this article’s proposal of urban health determinants, it is essential to note that it was considered that these determinants are the ones that, if not considered and taken into account in urban planning, then it may be classified as “urban stressors”. On the other hand, if they are part of the urban planning and urban design process, they can be considered beneficial elements that increase well-being, happiness, and quality of life, or as “urban conciliators or restorers” in the positive perspective of these determinants.
IV. Identifying the determinants of urban health
1. ‘Urban’ as a determinant
The knowledge that the built environment impacts health has ancient foundations. Until Hippocrates, health and disease were divine attributions of gift or punishment. In his treatise “Of Airs, Waters and Places”, he argued that human nature did not depend on the gods and justified the natural influence of the environment and its geographical factors, as well as the influence of physical characteristics of inhabitants of different regions, on health and disease.
The physical dimension of the places and their inhabitants acquired characteristics that demonstrate differences labelled as urban and rural despite being complementary in their functions in the face of growth and development. However, in a broader view, the ‘urban’ itself - perceived as a spatial condition and as a way of life - is understood as a determinant of health because it provides unique insights into defining characteristics of cities such as size, density, diversity, and complexity (Vlahov et al., 2007; Marques da Costa et al., 2013, 2020).
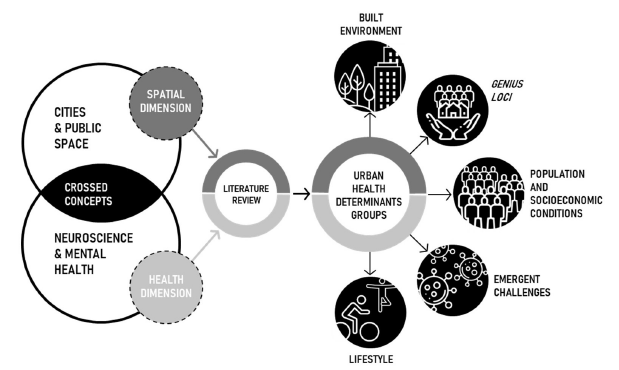
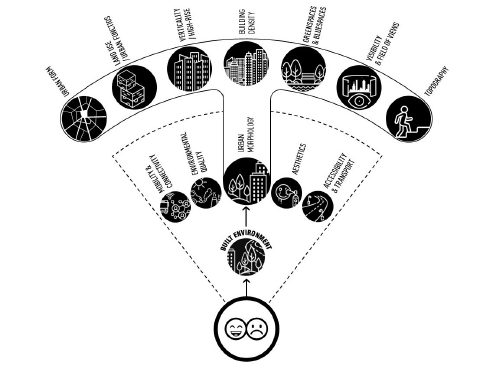
The proposed collection of urban health determinants derives from a comprehensive literature review. Here, some initial musings, and key concepts, through the lens of urban planning and urban design, are found, and, as a result, five groups of urban determinants that have a direct or indirect impact on health emerged. Figure 2 illustrates the methodological approach.
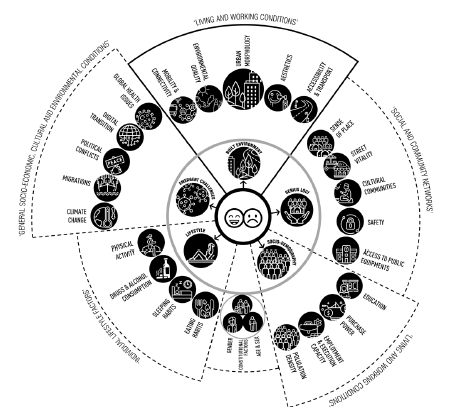
Also considering Dahlgren and Whitehead’s ‘rainbow model of the determinants of health’ and the distribution of the levels of the determinants (fig. 3), this article proposes a representation of a ‘determinant collection wheel’ (fig. 4), which intends to illustrate that any of the determinants can have a negative or positive impact on human health (depending on the conditions in which each one is found). Thus, they can assume the role of ‘urban stressors’ or ‘urban reconcilers or restorers’. Figure 5 shows the seven ‘sub-determinants’ related to ‘urban morphology’.
To explain each identified determinant, a table that systematises and summarises the findings across the comprehensive literature review on the relationship between the built environment and physical and mental health was built (table I).
Currently, the scientific work that has made it possible to ascertain the factors that condition mental and physical health in an urban context (table I) has mainly come from the fields of environmental psychology in dialogue with architecture and, more recently, with urbanism and urban planning.
The advances made in the technological field allow accessing neural signals in real-time as people interact with the built environment, avoiding the limitations and subjectivity of the studies from environmental psychology. Mobile EEG, health wristbands, wearable eye tracking and other wearable biological devices allow to cross biological data with contextual-geographical data and explore associations (Neale et al., 2019; Pykett et al., 2020).
V. Final remarks
Although urbanisation and city living offer many socioeconomic advantages, they can also be stressful. Today, there is a growing recognition that health, specifically mental health, must be addressed considering the social and environmental context. Therefore, health inputs are critical to urban planning, as mental health/illness is highly correlated with the urban environment and lifestyle. However, we argue that insufficient work has been done to integrate neuroscience content into urban planning and design.
To create healthier and sustainable cities and promote general well-being, urban planning must adopt neurourbanism principles. This means capturing brain signals triggered by the built environment stimulus and objectively uncovering how these impact people’s perception, cognition/emotions, and behaviour.
A healthy city and community contribute to citizens’ empowerment which in turn raise awareness on politicians and professionals to take action and address risk factors, e.g. noise, pollution, traffic jam, high density, accessibility, lack of green spaces and shadows, etc., that impact negatively on peoples mental health and well-being.
Similarly, urban planning and design can positively contribute to mental health. Having scientific evidence on what type of built and natural environment triggers positive emotions, promotes physical activity, and reduces stress and anxiety levels will inform urban planners and designers and empower them to (re)design healthier and more people-friendly cities.
The consolidation process of this new discipline, whose empirical evidence has claims to be fundamental for the future of cities and citizens, involves finding scientifically sound answers to a set of still open questions, such as:
When and where will neuroubanism be practised?
Who will be the agents disseminating and practising the discipline?
Will the Academy only educate this new discipline, bringing together neuroscience and urbanism?
Hou urban design of public spaces can be re-designed?
How to integrate co-creation and place-making within neurourbanism?
How to involve local communities and stakeholders in the process?
Will health centres be the first vehicle for the practice of neurourbanism, where, for example, family doctors (with complementary training in the new discipline) may prescribe the directed fruition of urban spaces, greenspaces or waterfronts instead of anxiolytics and antidepressants?
Which spatial planning toolkit integrates guiding measures coming from neurourbanism?
How to have citizens as reliable sources of information?
What methods and techniques should be adopted to produce, capture and analyse data?
Who is responsible for producing and disseminating such data at the neighbourhood/street scale level?
The relevance of this issue was pre-pandemic; however, it was covid-19 pandemic that brought people’s attention to the importance of mental health and its relationship with the built environment. The European Union created a ‘European Urban Health Cluster’ before the pandemic under the theme ‘Innovative actions to improve urban health and well-being’, addressing environmental, climatic, and socio-economic factors to optimise synergies and promote urban health in the European Urban Agenda.
There is a long-term search to identify urban variables and indicators related (directly or indirectly) to mental health, at different scales, with different natures and typologies; being very difficult to set universal parameters given the territorial and cultural differences of the multiple territorial settings analysed. For this reason, the diversity of social contexts, case studies and scales of analysis and the non-inclusion of factors of cultural contexts are pointed out as limitations in most articles. The lack of use of technology to obtain quantifiable biosensory data are also some of the limitations detected. Therefore, scientific papers often restrict their analysis to “empirical evidence” surveys and policy documents. The evidence results mainly from experiences in urban spaces, by structural or ephemeral interventions or by the absence of either, whose conclusions result from continuous observation, are not always standardised and constitute empirical knowledge in continuous development.
In the relationship between what is scientific and what is empirical, science must continuously add new knowledge to what has already been acquired, respond to new challenges, and draw inspiration from reality. Public policies should seek robustness in this new scientific knowledge. Based on evidence from current projects (such as the ones forming the Urban Health Cluster) and future ones, by 2050 (when an estimated two-thirds of the world’s population live in cities), neurourbanism must be a full-fledged discipline.
This article stands as a contribution towards that end. However, future research is currently under development to dive more in-depth into the topic, namely to 1) find indicators that can make the determinants measurable; and, consequently, 2) to define actions that can be translated into public policies on urban planning and health. Moreover, with the general recognition that science supports the better decision and help policymakers to meet people’s needs, it is anticipated that will be opportunities for more pilot studies on human-scale, which in turn will push authorities to provide more meaningful and trustworthy data with suitable scale granularity and that can be systematically produced and collected, and integrated into urban planning, and from there to the street’s realm.
Acknowledgements
This article was developed following the presentation made at the International Congress
GEOSAÚDE 2022 - “Inequalities in health, inequalities in the territory: challenges for Portuguese-speaking countries in a post-pandemic context” (thematic axis 4 - Healthy urban planning: an approach to health in all policies) and the respective article published in the book with the same title by the editors Eduarda Marques da Costa and Ana Louro from the Centre for Geographical Studies.
This article is part of the research developed within the eMOTIONAL CITIES Project, which received funding from the Horizon 2020 research and innovation programme of the European Union under grant agreement no. 945307. More information at https://emotionalcities-h2020.eu/
Author’s contributions
Ana Bonifácio: Conceptualisation; Methodology; Formal analysis; Research; Collection of scientific literature and policy documents; Infographics; Writing - preparation of original draft; Writing - revision and editing. Paulo Morgado: Conceptualisation; Methodology; Formal analysis; Research; Writing - revision and editing; Visualisation; Supervision. Angeliki Peponi: Methodology. Leonardo Ancora: Research. Diego Andrés-Blanco Mora: Research. Marta Conceição: Research. Bruno Miranda: Visualization; Research.