I. Introduction
Services of General Interest (SGI) represent services that fulfil citizens’ daily needs contributing to their well-being. They include health, education, social care, elder care or culture, services with strong social nature, energy, post and communications services, water and sanitation, among others, representing the economic nature of it. These services foster economic competitiveness and are crucial to social and territorial cohesion, while also being a vector for sustainable development (Bjørnsen et al., 2015; Commission of the European Communities CEC, 2004). Although appearing in the European Union (EU) policy process, the term is still very unclear (Lenaerts, 2012; Szyszczak, 2018; van de Walle, 2008). This category of services is one of the last Keynesian orientations in the current neoliberal free-market economy context, being on the side of cohesion (Waterhout, 2007) and marked as a fundamental piece in the maintenance of the European model of society (CEC, 2003).
SGI provision is conducted by “specific public obligations”, which means the State is obliged to prosecute their universal access as a fundamental right to citizens. Hence, these must be provided regardless of the type of territories, metropolitan areas, cities, towns, and rural areas, even if that is unprofitable as usually occurs in rural or low-density areas. But, despite the public service obligation determination, there is no more EU directive for SGI. So, the challenge is to ensure a harmonious combination of market mechanisms and public service missions (CEC, 2004), with each Member State responsible for the policies to guarantee the SGI provision, despite each one having its organizational structure of provision, reflecting different social values, ideologies, and policies (Humer, 2014; Littke & Rauhut, 2013).
Though being fundamental for territorial cohesion (Rauhut et al., 2013), the SGI provision process represents a large effort for the states in their financing. In a post-financial crisis atmosphere, with an austerity mind set, the prosecuted quality, accessibility, and affordability could be impaired, as well as future provision and maintenance (Kolarič et al., 2019; Marques da Costa et al., 2015). But it is in economically difficult times that SGI are more preponderant, as the public service is an essential support for economically and socially vulnerable regions. Therefore, public service is vital to diminish disparities among regions, especially by supporting rural settlements and maintaining an urban-rural balance (Marques da Costa et al., 2015).
This study emerges within the SGI and regional disparities themes, specifically in the health services, which are one of the most impactful SGI and iconic representatives of the Welfare State. As the SGI and the European Social Model are so connected, the study takes the Welfare State Regimes into account for assessing and understanding the regional disparities in health in the European context. In addition, due to SGI major role in territorial cohesion, special attention is paid to the rural regions. Hence, this study has two distinct phases, each with its main purpose. The first part scrutinizes the NUTS 0 level through the Welfare State Regimes, assessing the total and health expenditures made by the national and local government, trying to understand if there is a typology of spending in each Regime, but also understanding their behaviour with expenditures through a pre-crisis, crisis, and post-crisis period. The second phase, developed at a NUTS 2 level, elaborates on the search for regional disparities in health services across European regions, with special attention to the territorial typologies and the Welfare Regimes context, understanding if the urbanicity or rurality have an impact on the regional health service provision, but also the population health status, hence impacting territorial cohesion.
II. Services of general interest, welfare regimes, and territorial cohesion
1. The role of services of general interest in territorial cohesion
The term SGI lacks precision in its definition, there are no succinct criteria capable of explaining precisely what an SGI is (Lenaerts, 2012; Szyszczak, 2018; van de Walle, 2008). This terminological question does not arise in vain, SGI emerges as a top-down term, that was not accompanied by a national policy context, but rather classified by the EU itself (Bjørnsen et al., 2013). These services are fundamental for the EU, reflecting the right of access to a set of goods and services, the promotion of economic, social, and territorial cohesion, and contributing to sustainable development (Bjørnsen et al., 2015; CEC, 2003; Copus et al., 2013).
The inexistence or insufficiency of SGI provokes disparities among territories (Malý, 2018; Rosik et al., 2020; Sá Marques et al., 2020; Wiśniewski et al., 2021) which makes it fundamental for cohesion. This is noted by the Cohesion Policy, as it has recently shifted from economic efficiency to a more social binding and focused access to SGI and opportunities distribution (Weckroth & Moisio, 2020). This contrasts with the macroeconomic view that had reigned, and where its weaknesses thrived, especially in rural territories, recommending a homogeneous development path instead of several heterogeneous development paths adapted to the European Regions singularities (Demeterova et al., 2020). In fact, the use of macroeconomic and production indicators as a basis for measuring cohesion took well-being out of the equation, damaging the concept of development and jeopardizing regional convergence, with consequences in the exacerbation of regional disparities (Atkinson & Pacchi, 2020; Avdikos & Chardas, 2016; Weckroth & Moisio, 2020). In this sense, every region has its own characteristics and conditions but the bottom line, there is no territorial cohesion without SGI (Gruber et al., 2019; Hamez & Ruffray, 2015).
According to the various EU guidelines and its institutions, the provision of SGI must be governed by a set of principles, ordered by their greatest preponderance: guaranteed availability, accessibility, affordability, quality and variety of choice (CEC, 2003, 2004, 2007, 2011a). In fact, these principles are shared in the analysis of the provision of health services (Gulzar, 1999; Marques da Costa et al., 2020; Pechansky & Thomas, 1981), with accessibility being further dissected in subcategories (Ferreira et al., 2021; Freitas & Marques da Costa, 2021; Geurs & van Wee, 2004; Joseph & Phillips, 1984).
The supply of SGI is not regulated at the EU level; the organizational provision policies are Member States exclusive definition. Supply thresholds result from the interaction between providers and consumers and their ideologies and moral values, resulting from social policy and territorial planning and the current spatiotemporal contexts (Bjørnsen et al., 2015; Humer, 2014; Humer et al., 2013; Littke & Rauhut, 2013). Also, a great factor is the territorial occupation structure, where a concentrated typology is conducive to better access to services, creating a dichotomy between urban and peripheral or rural areas (Clifton et al., 2016; Copus et al., 2013; Gløersen et al., 2012; Humer & Palma, 2013; Milbert et al., 2013; Świątek et al., 2013). Moreover, rural and intermediate areas (generally) present inferior quality and levels of access to SGI than urban areas (Constantin et al., 2019; Rauhut, 2018; Stepniak & Rosik, 2013; Wiśniewski et al., 2021). And due to the EU directives on competition (Single Market Directive) and state subsidies (State Aid Directive), the difficulty in combating regional asymmetries is factual, being an obstacle to territorial cohesion (Milstein, 2015; Slot, 2013).
Another perspective to identify these territories comes from the lagging region’s classification provided by the EU (CEC, 2017). There are two types of lagging regions: regions with low-income and regions with low growth. Low-income regions owe their structural problems to the recent historical conjuncture and are mainly located in states that came out of the influence of the Soviet block at the time of its fall and recently joined the Union. These regions (and countries) have been showing important advances in convergence with the European average (CEC, 2017). The second group, the low-growth regions, includes regions further south or geographically more isolated from the European core, corresponding in a large sense to rural and peripheral regions. All of them are part of Eurozone countries, making adjustments to competitiveness more difficult and time-consuming to achieve than those in low-income regions (CEC, 2017). Unlike the latter, these have not seen improvements in their indicators, and are not converging with the national or EU average (CEC, 2017), despite being regions that had greater access to European funds, both in terms of time and amount of funding (Rodríguez-Pose & Ketterer, 2020). Nevertheless, many dimensions have been underrepresented in Cohesion Policy (CP) and its funding, and some of those are extremely important for these regions, as are the questions of aging and healthcare (Santana et al., 2020). Ultimately, and as Santana et al. (2020) demonstrate, based on an intersectoral and integrated approach, there is still room for improvement in CP to promote population health and health systems. However, the reality is that with or without CP, the responses to the crisis - an increase in the tax burden and a cut in public spending - turned the problems of low-growth regions denser, and they have effectively paid the costs of the crisis (CEC, 2017), with a particular incidence in rural and peripheral regions and large limitations in public investment efforts.
2. The relation of health services with Welfare State Regimes
Asymmetries in the health of populations, to an extent, are due to economic (Hill & Jorgenson, 2018), social (Clouston et al, 2021), cultural (Subica & Link, 2022) and behavioural (Franco & Marques da Costa, 2021) disparities - among other health determinants -, but also because of territorial inequity (different levels of service provision, accessibility problems, etc.). The State has a role in this with its policies for income redistribution and provision of goods and services - healthcare, education, conditions of existing work and leisure, housing conditions, among others -, managing regional disparities and the difficulty for populations to lead a healthy life (Marmot et al., 2008). Because health is dependent not only on the health sector but also on a conjunction of many health determinants (Carrapato et al., 2017; Gatrell & Elliott, 2015), policies and actions must be developed and conducted in a broad scope through holistic and integrated planning, in an intersectoral and multilevel way (Marmot et al., 2012) at regional and local scale applied not only to the health sector (Marques da Costa et al., 2020; Ferreira et al., 2021; Freitas & Marques da Costa, 2021) but also to other sectors, such as transport and mobility (da Costa et al., 2013; 2017 , 2021; Louro & Marques da Costa, 2019). These aspects are more evident in the more peripheral and rural territories, where service deserts are more likely to emerge (Rosik et al., 2020).
Thus, the actions of countries have a strong role in the health status of the population as they are responsible for the allocation and distribution of resources on health (or other sectors) and manage the interactions within health and between health and the other health determinants while trying to close regional health disparities (Bambra, 2011; Beckfield et al., 2015; Muntaner et al., 2011, 2017; Pförtner et al., 2019; Thomson et al., 2016). The different country policies have been aligned by several authors in Welfare Regimes typologies (e.g., Boeri, 2002; Esping-Andersen, 1989, 2013; Nadin & Stead, 2008; Sapir, 2006). A fusion of these perspectives results in five Welfare Regimes and a country classification can be observed in table I. These Regimes have dissimilar approaches to the economy and society, the Nordic has strong State intervention in the labour market and a wider fiscal policy; the Anglo-Saxon regime observes an important role of the State in benefit schemes and regular employment policies; the Continental regime shows the least labor market intrusive policies, but with a great power to the unions and their bargaining capacity; the Mediterranean has a very strict and protective legislation regarding employment, with pensions having a greater role in the dynamization of the economy (Sapir, 2006). From the point of view of public social spending, there are also relevant differences between Regimes; the Nordic registered the highest levels of social protection expenditures and universal welfare provision; the Continental has high investment rates with a large attention to pensions systems; the Mediterranean registered a low level of expenditures per capita, despite the national effort; the Liberal systems also present a lower level of public expenses; and the New Member States present low levels of expenses, despite having grown (Marques da Costa et al., 2015; Sapir, 2006). It must be stated that the New Member States Regime does not follow a clear path, it is very heterogeneous, with countries showing characteristics linked to multiple Regimes (Ferreira & Figueiredo, 2005).
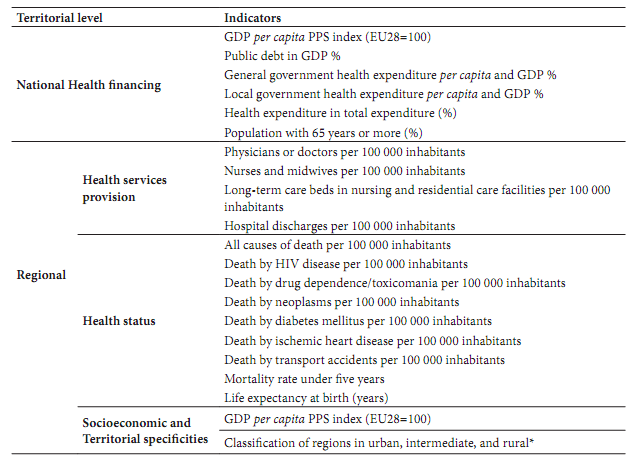
Table I Welfare Regimes and its composition.
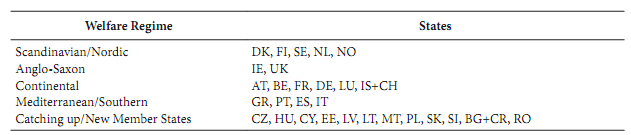
Source: adapted from Aiginger and Guger (2006); Boeri (2002); Marques da Costa et al. (2015); Nadin and Stead (2008) and Sapir (2006)
The Welfare State, through its policies, also impacts the effects that socioeconomic conditions produce on health, but not always in the same way, as different Welfare State Regimes show dissimilar ways to interact and influence how health determinants are translated to the population’s health status (Álvarez-Gálvez, 2016; Álvarez-Gálvez et al., 2014). There is an association between government spending and poverty, as higher expenditures are linked to lower poverty levels (Fritzell et al., 2013). Overall, expenditures are higher in the Welfare States with greater connections to poverty reduction, therefore, there is an association between poverty reduction and welfare policies, which in turn also affects health, since poverty is a fundamental health determinant (Marques da Costa, 2021).
The relationship between the Welfare State Regimes and one of its scopes of action can be assessed by its expenditures. By looking at health expenditures, one can evaluate their relationship with health. It is a fact that the universality of health services, brought by Welfare State policies, impacts the coverage of health services and the population’s health status (Kangas, 2010; Moreno-Serra & Smith, 2015). Likewise, the level of expenditure of public administrations on health has a positive impact on the population’s health status: higher health expenditures are correlated to superior health results (Bokhari et al., 2007; Farag et al., 2013; Vallejo-Torres et al., 2018).
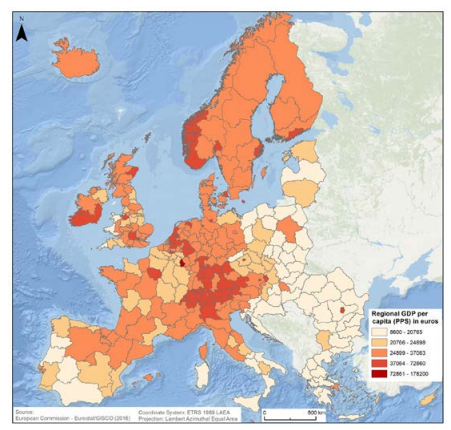
Another relevant aspect in the increase in expenses in EU regions is the aging population effect. This linkage is perhaps more relevant than the purely economic view (Lopreite & Mauro, 2017) as it induces larger demand for services in the territories with a larger share of aged people, as the rural and low-density ones, exactly where service provision is scarce.
In the last two decades, the Welfare State Regimes reformulation brought lower investments to the States where it was most needed. The crisis and the austerity that ensued, bolstered by the International Monetary Fund (IMF) gave way to the commodification of health systems (Greer & Mätzke, 2015), following a process of liberalizations, deregulations, and privatizations supported by the doing more with less paradigm (Hemerijck, 2015; Stubbs & Kentikelenis, 2017). Unfortunately, this was mostly felt in the countries most impacted by the crisis, which were the ones that already had several disparity problems and a great number of lagging regions. These States, like the Mediterranean countries, saw large expenditure cuts on social sectors, as happened with the health sector, resulting in a greater propensity to have weakened health care systems, lower health access, and higher regional disparities (Forster et al., 2020; Labonté & Stuckler, 2016; Ruckert & Labonté, 2017; Stuckler & Basu, 2009).
III. Data, methods, and area of study
The analysis of regional asymmetries in access to health services does not follow the general path of associating the Health Systems with access, as is the case of Ferreira et al. (2018). Instead, it is based on an appreciation of different Welfare State Regimes, linking the government expenditures made at the national and local level with the existence of health services in EU regions (NUTS 2). To this end, three distinct situations corresponding to the 2006-2016 period were analysed, one pertaining to a pre-crisis year (2006), another to a year of crisis (2012), and the last one to a post-crisis period (2016).
There are two scopes of analysis in this article:
analyse the investment, that is, the way the State deals with health and the level of the investment (national and local), observing the results aggregated by the Regimes behaviours in each of the three periods. That phase is developed at NUTS 0, assessing public expenditures by groups of countries corresponding to Welfare State Regimes. The groups of countries come from the 27 EU countries with the addition of Iceland, Norway, Switzerland, and the United Kingdom (indexes are created with the average of the 28 EU states because in the studied period the UK was still a Member State), focusing on:
the economic performance based on Gross Domestic Product (GDP) per capita and Public debt in percentage of GDP;
the correlation between total and health expenditures at the national and local level with the economic performance (public debt) and demographic characteristics (population with 65 years or more);
the level of effort of the countries in public investment at both levels (national governments and local governments) analysed by the total public expenditures and, in specific, the health expenditures spent at the national and local government levels;
the influence of demographic structure on the needs of investments (% of population with 65 years or more).
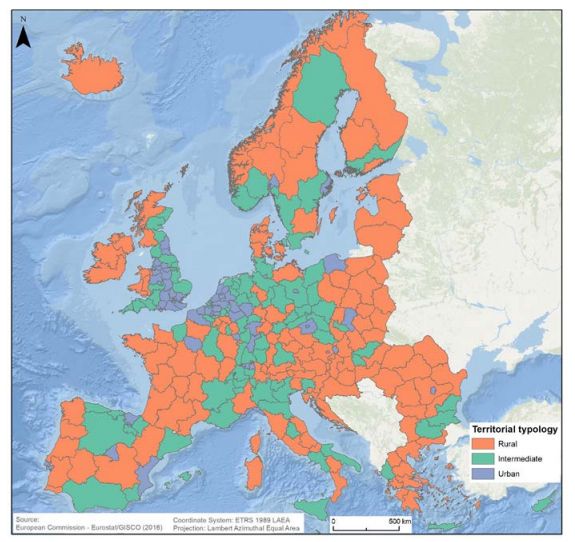
after establishing the previous typology of expenditures profile in the function of Welfare State Regimes, there is a transference to the regional scale (NUTS 2), where European regional disparities concerning the health services provision (four indicators) and the health status of populations (nine indicators) are analysed considering two important frameworks: the socioeconomic territorial characteristics of the regions and the Welfare State Regime context coming from part 1, represented by the GDP per capita and the urban classification of regions, of Eurostat (urban, intermediate and rural) (fig. 1).
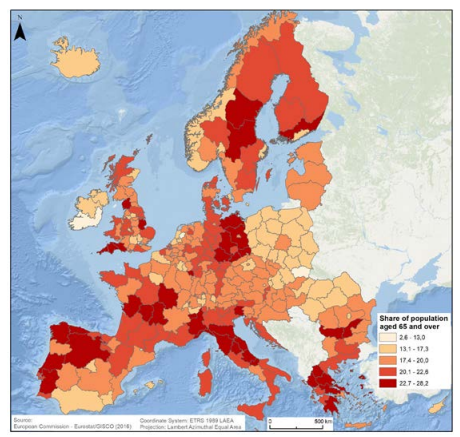
The selection of indicators was based on the WHO indicators list, considering three types of indicators (World Health Organization WHO, 2018):
for the national level, health financing indicators that represent input/efforts in the system;
for the regional level, health provision (service access as output indicators) and health status (considered impact indicators). Health provision and health status indicators are complemented with a third group of determinants: socio-economic and territorial specificities.
It is important to stress that the NUTS 2 level was chosen for the regional analysis due to being the last territorial level with information regarding the studied matters. This scale is not the preferable, but what is possible, as the NUTS 3 level would be the desirable one in this type of analysis. This does not compromise the results, only makes it difficult to go even deeper in the conclusions. Nevertheless, even at NUTS 2 level, some important indicators do not exist, and the available ones sometimes show great levels of missing data (years/regions), impairing analysis from a territorial and temporal viewpoint.
For the development of this study, only statistical indicators available to the public were used, enhancing its transparency, and allowing its replication for other years. As such, Eurostat was the main database used. The variables used are the best considering the availability and quality of the data, nonetheless, because in certain indicators data quantity and/or quality was poor, it was necessary to use the national statistical institutes for some countries. Table II shows the used indicators.
IV. Government expenditures by welfare regimes of the european countries
The socioeconomic context underwent major changes between 2006 and 2016, but the most extreme situation was the public debt crisis. In general, there was a decline in GDP per capita and an increase in the share of public debt in GDP from 2006 to 2012 and the reverse from 2012 to 2016. In terms of the Welfare Regimes, there was not one that clearly improved. However, the opposite is possible to demonstrate: from 2006 to 2016 the countries included in the Mediterranean Regime showed a strong negative trend, and it was here that the crisis left most metastases. Also, table III presents the data by Regimes types for the analysed years in terms of GDP and population with 65 years or more, demonstrating the perilous evolution of the Mediterranean Regime.
Table III GDP per capita (Index EU28=100) and share of the population with 65 or more years by Welfare State Regime (2006, 2012, 2016).
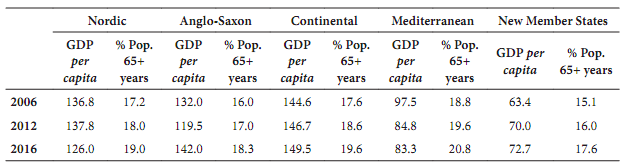
Source: Eurostat
The evolution between public debt and government expenditure shows that the increase in public debt, a consequence of battling the crisis, resulted in a change in SGI spending patterns, contributing to a deepening of regional disparities. It is also confirmed that the increase in spending, especially that related to health, as stated by Lopreite and Mauro (2017), is associated with an aging population.
Looking at table IV, there is a noticeable increase in the intensity of correlations and expenses as a percentage of GDP from year to year (regardless of scale or type), this occurs in evermore senior Europe. This correlation is particularly relevant in health expenditure by local governments, demonstrating its importance in this matter and in national government expenditure as a percentage of GDP, where a correlation coefficient with some expression is registered. This suggests that, not only in health expenditures but also in the total social state expenses, an aging population requires ever-increasing expenditures. The findings explain, for example, the Southern States national and regional reality, where an older population leads to the existence of a reduced GDP per capita - indeed, many regions are going through the brain drain phenomenon and its socioeconomic effects (CEC, 2017) -, but increases spending needs with the dire necessity to supply SGI, all while presenting worrying levels of national indebtedness. This service provision necessity must be seen along with the growing difficulties to justify public investments due to depopulation in most of these (lagging low growth) regions (Perucca et al., 2019).
For the first period of analysis (2006-2012), the first evidence is that all Welfare State Regimes presented an increment in the share of public expenditure in GDP at the national government level and a drop from the 2012 to 2016 period. This resulted is an increase in the total average, but it was accompanied by the standard deviation, showing that the dispersion followed the growth tendency, both on total and local expenditures. In fact, as table V shows, despite the decrease in the average values, in the second period of analysis the dispersion kept on rising. It is important to notice that with the exceptions of Anglo-Saxon and New Member States Regimes, all other Regimes sustained a share in GDP expenditure levels higher than the initial year (between 5,6% to 7,9% variation). The second evidence comes from the relation with the demographic structure. The Regimes whose countries have an older population structure show an increase in social public expenditure share in GDP, as suggested above. Further proving the change in relations, namely, the expenditure reduction related to public debt in favour of an augmentation induced by aging. Looking at per capita public investment values it becomes evident that the Mediterranean and the Anglo-Saxon Regimes are the only ones with a clear reduction tendency, retreating the crisis impacts on economies.
Table IV Correlation between public debt and percentage of population with 65 years or more with government expenditures (2006, 2012 e 2016).
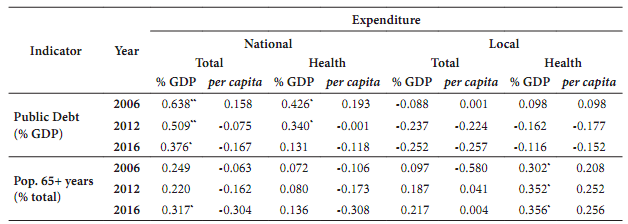
Note: *Significant correlation at 0.05 level (bilateral). **Significant correlation at 0.01 level (bilateral)
Table V Share of national and local public expenditures in GDP (%) and public expenditures per capita (index 100=EU28) for each Welfare Regime (2006, 2012, 2016).
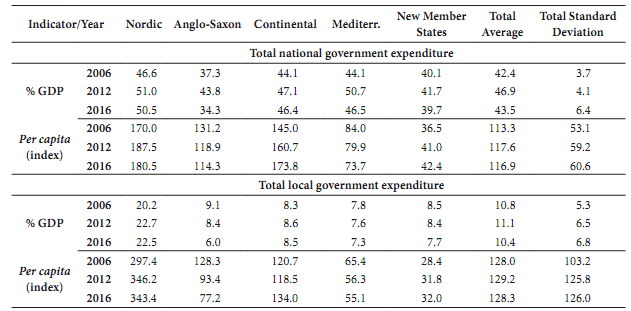
Source: Eurostat
Looking at the starting year, countries of the Nordic Regime show a significant prominence in general government health expenditure in terms of GDP percentage and its expenditure in euros per capita in the health sector. These marks follow the economic power rule observed in national expenses, richer countries spend more in the health sector than poorer countries, varying amongst themselves in terms of socioeconomic characteristics and leading political, economic, and market ideologies. In 2012, the Nordic Regime continues to enhance its differences regarding health expenditures, as now there are roughly two groups besides it, one constituted by the Anglo-Saxon and Continental Regimes, and the other with the Mediterranean and the New Member States Regimes. As for 2016, the ranking on general government health expenditure per capita keeps its standing, but with a strong approximation between the Mediterranean and New Member States Regimes. However, there seems to be an ever-increasing gap rising between the top three expenders and the bottom two (fig. 2), fueling more regional discrepancies in health services provision. This year also marks the end of the correlation between public debt and general government health expenditure (table IV), noting that the correlation coefficient had been decreasing since the beginning of the analysis.
From figure 2 is also possible to understand that heterogeneity exists amongst the Regimes, but also inside them. The dispersion is a factor, particularly in the Nordic and Continental Regimes in the post-crisis year. This shows that, although each regime displays a certain preponderance of behavior regarding national government health expenditure, some discrepancies and outliers still occur.
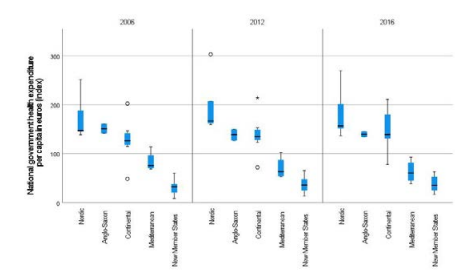
Fig. 2 National government health expenditure per capita by Welfare Regime, in euros (2006, 2012, 2016). Source: Eurostat
Complementarily to the national efforts, there are expenses related to the local government level, namely by municipal entities with different decentralized competencies. Considering the local government expenditure, there are two distinct groups: the Nordic Regime, and the others, with a huge difference between them (table V). This dichotomy reflects a greater responsibility for budget allocation in local governments in the Nordic Regime, as well as a larger dependence on these administrations for the provision of SGI (at least budget-wise), specifically, those greatly related to the local level. Another distinctive feature of local government expenditure is the values recorded for the crisis year, with expenditure not growing as a percentage of GDP. In addition, the others reduced spending and kept reducing it in the post-crisis period, disclosing a decrease in the importance of local government expenditure.
In particular, for local government health expenditure, there are two distinct typologies in terms of GDP percentage: the expenders, Nordic, Mediterranean, and New Member States; and the non-expenders, the Anglo-Saxon and Continental. Nevertheless, when analyzing the indicator of expenses per capita, the New Member States Regime turns almost into a non-expender. The tendencies for 2006, 2012, and 2016 are very similar, with some variability in each year but with no major changes. Also, in the local government health expenditure, the conjecture factor does not play a significant role, as in the crisis year there was no propensity for modification (to the contrary to what happened in the general expenditures). The Nordic Regime is the biggest spender, followed at a considerable distance by (some countries of) the Mediterranean, with this associated with the political and administrative structures.
Disparities between Welfare State Regimes bring to the top the variances in the organizational administration structures. This means that there is no clear system in terms of local government and health responsibilities, perhaps apart from the Nordic and Mediterranean States, groups where only one and two States (respectively) have a reduced expenditure on this matter (fig. 3). In some cases, health services and their actions and financing processes are executed by the local government, in compliance with bigger and broader national or regional programs, making it a more horizontal provision method. In other cases, the bulk of health responsibilities lies within a larger scale government, relating to a more top-down approach, revealing a limited local government expenditure (sometimes inexistent).

Fig. 3 Local government health expenditure per capita by Welfare Regime, in euros (2006, 2012, 2016). Source: Eurostat
There were multiple performances regarding the variation rate of general government expenditure on health. In the Nordic Regime, the annual rate was positive on every occasion and just one State (Finland) was a little beneath the mean value. Meanwhile, the biggest per capita spenders kept on rising. In the Anglo-Saxon, the United Kingdom had a positive rate and Ireland had a negative rate, in which the effects of the financial crisis can be a reason. For the Continental Regime, there was some dispersion, counting with values below average, but the only negative rate was related to Iceland (another country greatly affected by the crisis). The Mediterranean Regime had a disappointing performance with various very negative values, maintaining a poor overall path. The Mediterranean Regime seems to be the more profoundly affected by the crisis and rise of the national debt. The huge national debts allied with a declining economy and the external intervention through the IMF adjustment programs, ruled by an austerity paradigm - as already discussed - paved the road to decreased health expenditure (both in general and local government). Finally, the New Member States presented mixed behaviours, contrasting some of the best rates with roughly some of the worst.
Overall, there is one clear rule, higher GDP per capita and stronger economies lead to higher general government expenditures, either total or in health. Also, expenditures tend to be organized by Welfare State Regimes, that is, being part of a Regime is connoted with a certain behaviour expenditure-wise. Also, it was observed that the local government expenditure plays a big role mainly in the Nordic Regime.
The crisis had an impact on all States and regions, there is no discussion on that, but some felt it more than others. The Mediterranean Regime and its States clearly had the bitter end and could not resurface to the pre-crisis expenditure levels.
V. Regional health disparities in europe
From the previous analysis, differences between countries emerged linked to the political and administrative social model organization and expenditures profiles. Subsequently, how are national Welfare Social Regimes patterns translated into health provision of services? Are there any differences in health status on a regional scale? The analysis of the indicators of provision of services and health status at a regional scale in the EU context gives contributions to this analysis. This article relates the national data about expenses and socioeconomic support of the countries and the regional performances in terms of health services provision and status. The analysis considers three types of EU regions, representing three types of territorial characteristics: urban, rural, and intermediate regions.
As initially postulated, SGI gaps characterize rural areas. These territories are sparsely populated which impacts the organizational minimal standards necessary for the existence of provision structures. Also, these areas tend to have a more vulnerable population, as the degree of aging is far greater than in urban areas. But not only, it is preponderant to relate SGI provision with GDP, as richer regions have a greater capacity to provide them than poorer regions. Furthermore, predominantly urban regions tend to have a superior GDP per capita.
Indicators of healthcare services provision (physicians or doctors, nurses, or long-term care beds per 100 000 inhabitants) tend to accompany the regional socioeconomic and territorial characteristics. So, higher GDP capita regions correspond to urban areas with more health services. Besides, it seems that regions integrating Welfare State Regimes with stronger public service and higher expenditure levels, although presenting worse socioeconomic conditions or greater rurality (figs. 4 and 5), show more positive health services than other more developed regions that integrate weaker public provider Regimes. Not only do more urban regions in weaker Regimes have good results - and better ones than the regions that encircle them - as in the example of Prague -, but also, sparsely populated regions in stronger Welfare Regimes, mostly in the Nordic Regime (for instance the Upper Norrland region) have good results in these indicators. This situation is particularly evident in long-term care beds in nursing and residential care facilities. Also, in the studied period, we found some countries, mainly from the Mediterranean Regime, that registered a decrease in health expenditures and synchronously in the observed indicators, deepening regional disparities, especially as most of those regions are low-growth regions and were already lagging behind.
Although having some of the lowest investment levels, the Mediterranean Regime presents a favorable performance in the provision of services, shown by the larger number of doctors or physicians per 100 000 inhabitants in all territory types - which in part is due to its general health model approach, that is “intensive” in doctors and “extensive” in nurses -, while the New Member States Regime counts with a great number of it in urban areas but not in other areas (table VI). Nevertheless, these regimes have a low per capita number of nurses and midwives and long-term care beds. When analysing hospital discharges, the biggest values are in the New Member States and the lowest in the Mediterranean Regime. Showing that, although having a smaller offer, the latter also has a potentially minor necessity, on the contrary, the New Member States present a diminished offer with a theoretically greater necessity.
Looking at the territorial aspect, in general, there is a tendency to have a better offer in the urban areas than in the rural ones (table VI), which confirms the urban and rural disparities in Europe. Nonetheless, in the Nordic and Anglo-Saxon Regimes - but mainly in the first - there are situations in which the reverse occurs, that is, the rural areas present a larger offer, mainly, in the care services. This is in line with the necessity of such services, as the rural areas have a more vulnerable population due to their greater proportion of senior individuals. Hence, it is alarming that the Mediterranean Regime does not follow this trend, as it comprises the bulk of low-growth regions and its low-density, economic stress, and (major problem) aged population.
Table VI Health services per 100 000 inhabitants by Welfare Regime and territorial typology (2016).
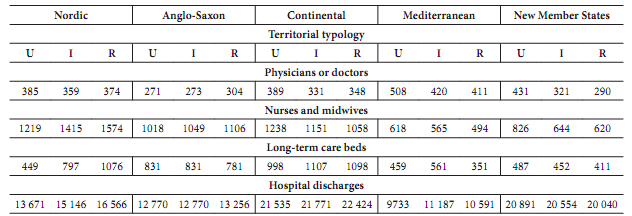
U=Urban; I=Intermediate; R=Rural
Thus, less financing capabilities will keep on widening the disparities that plague European regions, and due to the States that constitute the Mediterranean and the New Member States Regimes, is fair to assume that the gap will widen further.
The analysis of the standardized death rate by causes gives the possibility to assess on one side the primary health care and on the other the hospital care. Primary health care is observed via the standardized death rates due to HIV, diabetes, and drugs. These variables, excluding drugs, have been decreasing their impact on deaths, but still, there are some particularities per Welfare Regime. So, at the local level, only three Welfare Regimes made some positive evolution in the studied period: Nordic (notably this one), Anglo-Saxon, and Continental; the other Regimes have increased their rates. This result shows an interesting duality, both Nordic and Mediterranean Regimes have an important local government expenditure on health, however only one has witnessed benefits. The same applies to the remaining Regimes, although no extensive expenditure, some achieve better results than others. This may have a connection with implemented policies and practical outcomes derived, besides ideological, political and governance frameworks have perceptible traits of dissimilarity, for instance, the relation between market forces and the Third Sector. Also, it is important to note that in some cases, the local government has the right and duty to operate and control parts of the health service system, however, the means for it are not there due to governance problems and administrative complications.
In the hospital care theme, there is a clear trend of reduction in occurrences (table VII), all Welfare State Regimes were prolific in decreasing death rates. Although all are very close, the most effective in this reduction is the New Member States Regime, followed by the Mediterranean Regime. Here, those who spend less show benefits as those who spend considerably more. However, this is in part explained due to a worse starting point and, thus, a bigger impact from improvements.
Table VII Health status indicators per 100 000 inhabitants by Welfare Regime and territorial typology (2016).

U=Urban; I=Intermediate; R=Rural
Nevertheless, despite the values in hospital care for the Mediterranean and the New Member States Regimes, the Nordic, Anglo-Saxon, and Continental Regimes are the ones that have been improving the most in healthcare, making it difficult to converge. Therefore, territorial cohesion is not a reality, it is a fact that these underdeveloped regions are doing better in general, but so are the more developed ones. Thus, regional disparities perdure as always.
Combining these results with the previous analysis (profiles of expenditures made by the national and local administrations) comes one possible evidence; the regimes where national government expenditure on health is a major investment can achieve more solid results. However, the local government expenditure on health is not a clear-cut winner, being more intricate and problematic than it would seem at first sight: the local investment in health improves the primary care support, and that could be relevant for rural territories.
Territorially wise, the urban-rural distinction is real. The results in health status showed by the Life expectancy at birth and general mortality rates are usually better in urban areas, fall in the intermediate and finally reach the bottom in the rural areas. In fact, some rural regions in the Regimes with the best results, present better results than richer and more developed regions in the Mediterranean and the New Member States Regimes, showing that Welfare Regime and its characteristics can circumvent the rurality trait and its healthcare impacts.
VI. Conclusion
The results showed relevant differences in terms of policy efforts and population results in health status, between Welfare Regimes. Nordic, Anglo-Saxon, and Continental Regimes are the biggest national government health spenders, and this accompanies the general expenditure; more spending in the latter means bigger expenses in the first. This leads to a growing gap between the economically sturdy Regimes and the less sturdy ones.
In complementarity to the national government expenditures, the local government plays a major role in Nordic and, to an extent, in the Mediterranean Regimes, although it barely exists in the remaining regimes. However, the results show that service provision and health status results simply do not accompany the investments in the Southern States, being possibly related to socioeconomic fragilities and the low-income of the population, demonstrating the importance of national and local public investment to cohesion and regional development. It was also concluded that, contrary to what was established with primary healthcare, on the hospital care level, all Regimes demonstrate capabilities to achieve results.
A second conclusion is the confirmation of cleavage between health services in urban, intermediate, and rural territories, a hindrance to territorial cohesion. Also, territorial characteristics constitute a robust health determinant. Nevertheless, it was concluded that Welfare State Regime practices are linked to the countries socioeconomic profiles and its characteristics seem to have the power to minimize the territorial impacts on health. As pointed out, some of the rural less developed regions within some Welfare Regimes, have better results than urban prosperous/developed ones located in the Mediterranean or the New Member States Regimes (mainly the last).
So, disparities in healthcare between European regions have two major obstacles, GDP per capita and territoriality (rurality). Higher GDP per capita and higher urbanization result in better services. This follows the logic that greater density allows reaching demand thresholds more easily and, therefore, there is a greater number of services in urban areas, while in other territorial typologies, the viability of the service implies an extension of its coverage area, making the service more distant and, thus, less accessible (Palma et al., 2017). But service availability is not the only factor that defines the health status, socioeconomic factors, and the model of access to health services (near or far, free or paid) play an important role. So, the biggest barrier to equity in health is wealth (consumer) and scale economies (producer).
Across the studied period, the asymmetries in health among Welfare Regimes increased. Convergence was observed at the top and bottom, but the pit between widened. The Mediterranean Regime emerges as the most concerning situation, suffering with the public debt crisis and showing a downgrading in investment and yet still encompassing most of the low-growth regions. Hence, the gap, between these territories and more developed ones, keeps widening, either national or international. Ultimately putting territorial cohesion at stake and the healthcare structure in a challenging situation as the socioeconomic development condition of the countries organized in different Welfare Regimes accounts for intra and inter-regional disparities at the EU level.
This article returns to the theme of regional Europe and services, but much more is needed. Future research should consider these findings and explore the associations found in this work. Further investigations need to look for the quantification of said relationships, the development of models to verify and test even deeper regional disparities are a need for regional science and European territorial cohesion. Also, future studies should follow two different scopes, focusing each time on the NUTS 0 or on the NUTS 2 level, this will expand the range of possible methodologies and potentially enhance the quality of obtained results.
Author contributions
Pedro Franco: Conceptualization; Methodology; Software; Validation; Formal analysis; Investigation; Resources; Data curation; Writing - original draft preparation; Writing - review and editing; Visualization. Eduarda Marques da Costa: Conceptualization; Methodology; Validation; Investigation; Writing - original draft preparation; Writing - review and editing; Supervision.