Introduction
Imaging examinations are fundamental in clinical practice, aiding physicians to obtain and rule out diagnosis, perform assisted procedures, and establish treatment plans.1 Consequently, their global usage has increased, rendering them indispensable in current clinical practice, and presenting both medical and legal value.1,2During their request, there are mandatory fields, the completion of which is the responsibility of the prescribing physician.3 These fields must necessarily contain relevant clinical information and a provisional diagnosis and/or diagnostic doubt that justifies the request,3,4providing the radiologist with an accurate context. It is known that the provided clinical information impacts the interpretation and consequently the accuracy of the produced radiological report.5,6,7
According to the best practice manual created by the Portuguese radiology specialty college, the request should include all pertinent information, a clinical summary, and the questions to be clarified.3 If the study's indication is not clear or appropriate and the examination is potentially harmful, the radiologist can point out the insufficiency found and suspend the examination.3
Considering the provided clinical information as an essential communication tool between the requesting clinicians and the radiologist,4,8,9we know, however, that its importance is sometimes undervalued.10,11The provision of adequate information allows the reduction of unnecessary examinations, improvement of the quality of service provided to the patient,2,10,12production of pertinent imaging reports,13 and a decrease in the number of incomplete reports.10
Although published clinical audits confirm the existence of deficits in filling out clinical information in imaging examination requests,10,14,15it is important to note that these results do not reflect malpractice, but that there is room for optimization.
Given the known relationship between the provided clinical information, its impact on the quality of the produced radiological report, and its importance in medico-legal context, the relevance of this study becomes evident, as a view to understanding the practices of filling out imaging examination requests by clinicians at our hospital.
Our aim is to assess the completeness of the mandatory fields in the request of imaging examinations [ultrasound (US), computed tomography (CT), and magnetic resonance imaging (MRI)], focusing on the clinical information and the suspicion/diagnostic doubt to be clarified, requested by the doctors of the Health Service of the Autonomous Region of Madeira (SESARAM), to the Radiology service of Dr. Nélio Mendonça Hospital (HNM) (level III), which provides care to a resident population of approximately 250,000 inhabitants, in addition to a variable floating population. We therefore aim to acquire a global perspective of the current practices of the requesting clinicians.
Material and methods
Study design and setting
This retrospective study was conducted at the Radiology department of HNM - SESARAM, Portugal. All requests for US, CT, and MRI requested on the ATRIUM® platform between May 1st and 31st 2022 were included. Data were collected retrospectively through the Radiology department database using RIS-Glintt software (version GCX2201.01). Approval was obtained from the health ethics committee and the SESARAM scientific and research committee.
Data collection and variables
All imaging examinations requested by the doctors of SESARAM on the ATRIUM® platform are stored in the radiological information system (RIS/PACS). This information is retrospectively accessible with RIS-Glintt software, allowing the selection of exams based on patient data, type of exam, location, and date of execution. After identification of the exams that meet the defined criteria, the completeness of the information provided in the mandatory fields was analyzed. No data were collected that allow the identification of the patients or the correspondence with other databases. The project's database does not contain information that allows identifying the patients, and the investigators do not have access to data from the examinees from other sources.
Data were manually collected and stored in an Excel® spreadsheet. We analyzed the variables: date of the request; patient’s gender and age; requested imaging examination; origin of the request; and clinical information filled out by the physician. The date of the request corresponds to the date in which the exam was requested, having included all requested tests on the ATRIUM platform from 05/01/2022 to 05/31/2022. The requested imaging examination refers to the modality of examination: US, CT, and MRI, considering for each exam the evaluated anatomical region. The origin of the request indicates the place where the exam was requested: emergency department, inpatient, outpatient consultation, and outpatient clinic. The provided clinical information was then classified as adequately filled out, incomplete, and missing. It was considered adequately filled out when both mandatory fields contained: (i) clinical context of the episode that motivated the request (with or without reference to relevant findings on physical examination AND/OR laboratory results) and (ii) diagnostic suspicion/questions to be answered with the study. It was considered missing when both points mentioned were not filled with comprehensible information (e.g., ".", "ditto", "abc", "..."). It was considered incomplete when only one of the mentioned fields (i) or (ii) were not filled out comprehensibly.
Given this study's objective and the subjectivity in the interpretation of the clinical information, all the provided information that complied with the referred criteria was considered valid, without any judgment as to whether it was relevant in the context of the requested examination. This approach thus prevented possible interpretation biases inherent to the subjectivity of the adequacy of the information.
Statistical Analysis
All analysis were conducted using the IBM SPSS Statistics software (version 25). Continuous variables were summarized with mean and standard deviation. Categorical variables were described by frequency and percentage in each group.
Statistical tests (Pearson's chi-squared) were used to evaluate statistically significant associations between variables - requested imaging exam, evaluated anatomical region, origin of the request - and the clinical information filled out by the requesting physician. The level of statistical significance was set at 5%. Statistical support was sought from the Dra. Maria Isabel Mendonça Research Center to assist in data analysis.
Results
Patient demographics
In a total of 2930 imaging examinations included in the study, the most requested was CT with 1995 requests (68.1%), followed by US with 684 requests (23.3%) and MRI with 251 requests (8.6%) - Figure 1. Patients’ mean age for whom imaging exams were requested was 58.3 ± 20.5 (mean ± standard deviation) and most patients were female (n=1534, 52%). Demographic data can be found in Supplementary Table 1 of Appendix 1.
Requested examinations
Considering the anatomical region, the most requested exam was Upper Abdomen CT scan with 613 (20.9%), followed by Pelvic CT scan with 591 (20.2%), and Thoracic CT scan with 551 (18.8%). Together, these accounted for 59.9% of the requests made during the study period - Supplementary Figure 1 of Appendix 1.
Requested examinations by origin
Regarding the origin of the requested exams, most originated from outpatient consultations totalling 1719 (58.7%), followed by inpatient 608 (20.8%), emergency department 567 (19.4%), and outpatient clinic 36 (1.2%) - Figure 2.
Completeness of clinical information filling in the requested examinations
2092 (71.4%) examinations had been requested with adequately filled clinical information, 800 (27.3%) incompletely filled, of which 170 (5.8%) lacked the clinical context of the episode that motivated the request and 630 (21.5%) lacked the diagnostic suspicion/question. Finally, in 38 (1.3%) requests the clinical information was incomprehensible - Table 1.
The Upper Abdomen CT, Pelvic CT, and Thorax CT obtained the highest number of requests with adequately filled clinical information, with 479 (16.3%), 445 (15.2%) and 443 (15.1%) respectively - Table 1. Interestingly, these were also the examinations that had a higher proportion of incomplete filling, lacking the diagnostic suspicion/questions to be answered with the study in 106 (3.6%), 112 (3.8%), and 83 (2.8%), respectively.
Association between requested imaging exams and the adequacy of the clinical information filling
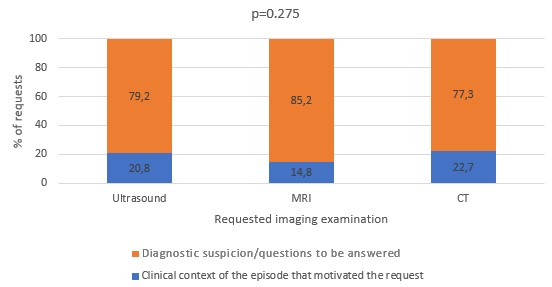
Of the 2092 imaging exams requested with adequately filled information, 1522 corresponded to CTs, 408 to ultrasounds, and 162 to MRIs. Conversely, of the 800 requested examinations with incomplete information, 459 were CTs, 260 ultrasounds, and 81 MRIs. Moreover, the diagnostic suspicion/questions to be answered were absent in 355 of those requests for CT, 206 for US and 69 for MRI. Also, out of the 38 requests with missing information, ultrasound was the exam with the highest number of requests, with 16, followed by CT with 14 and MRI with 8.
A significant association was observed between the requested imaging method and the degree of completion of the provided clinical information (χ2 = 84,137, p <0.05) - Figure 3. However, no relationship was identified between the missing clinical information parameter and the requested imaging method (p > 0.05) - Supplementary Figure 5 of Appendix 1.
Association between the origin of the requested imaging examination and the completeness of clinical information filling
Regarding the origin of the requested examination, the outpatient consultation (1261), followed by inpatient (425) and emergency department (383), had the highest number of adequately filled out requests. On the other hand, the setting where examination requests were filled out incompletely more often, were the outpatient clinic (426), emergency department (181), and inpatient (180). Interestingly, in the outpatient clinic, no exam was requested without clinical information. A significant association was identified between the filling out of clinical information and the location in which the request was originated (χ2 = 23.508 and p<0.05) - Figure 4.
In examination requests accompanied by incomplete clinical information, it was observed that the most frequently omitted information was the "diagnostic suspicion / questions to be answered with the study" in 13 (100%) requests originating in the outpatient clinic, 353 (82.9%) in the outpatient consultation, 132 (73.3%) inpatient, and 132 (72.9%) in emergency. A significant association was identified between the location in which the request was originated and the missing clinical information (χ2 = 14.638 and p<0.05) - Figure 5.

Figure 4: Association between the origin of the imaging examination request and the completeness of clinical information
Discussion
This study aimed to understand the practices related to the filling of mandatory completion fields in the requests for imaging examinations at our hospital. This form represents a request for a specialist opinion from the radiologist,3 with medico-legal value.4 Beyond its importance for the preparation of the imaging report, the provided information aids in adhering to the principles of radiological safety - "As Low As Reasonably Achievable" (ALARA),4,16proposed by the International Commission on Radiological Protection (ICRP) in 1977, given the frequent use of ionizing radiation4 - through the evaluation of the appropriateness of the requested examination and the consideration of the risk-benefit ratio.1 Literature shows that there are documented difficulties in the adequate filling of the request for imaging exams, which create challenges in assessing their appropriateness.4
In total, 2930 imaging exams were requested, equivalent to about 95 requests per day. The most frequently requested examinations were CT scans of the upper abdomen, pelvic, and thorax, representing more than half of the requests during the period in which data were gathered. Generally, these exams are requested in conjunction for staging and evaluation of the response to treatment of neoplasms. Therefore, we consider these results to be expected. On the other hand, the least requested exams were Angio-MRI, Entero-MRI, and Entero-CT, used in the assessment of specific clinical questions, which is also expected.
Most imaging examination requests originated from outpatient consultations, which is anticipated since this is where patients with chronic conditions, such as neoplasms, are followed-up on an outpatient basis. The outpatient clinic had the fewest requested orders, as predictable, considering that its primary goal is the provision of ongoing care to patients, with examinations only being performed to clarify specific questions.
The analysis of the clinical information provided by the requesting physicians shows that although many requests were adequately filled out 2092 (71.4%), there is still a considerable number of imaging examinations 800 (27.3%) with incompletely filled out information, and in rare, but non- negligible, cases filled without any comprehensible information 38 (1.3%), thus creating additional challenges to radiology physicians. They are then faced with difficulties, having to consult the patient's clinical file and/or contact the clinician in-charge to better understand the clinical context and how they can add value to the care provided. The result is a disruption of their usual workflow, with a significant amount of time allocated to gathering information, culminating in a reduction in the number of examinations reported with a possible impact not only on patients (who depend on the execution and interpretation of the exams), but also on the institution, contributing to an increase in the number of exams on the waiting list. The non-negligible number of exams with insufficient clinical information could also be explained by the difficulties experienced by clinicians who sometimes find themselves confronted with uncooperative patients, incomplete clinical records, patient overload, and failures in computer systems, making the task of filling out clinical information challenging.
Significant differences were found in the filling out of clinical information according to the imaging method requested, with clinicians more frequently filling out the clinical information in the mandatory fields adequately in CT requests, incompletely in US requests, and without comprehensible clinical information in MRI. These results are surprising, especially considering that MRI - given its long acquisition time and high economic cost - is typically performed as a last resort exam to clarify doubts stemming from previous studies, therefore requiring adequate clinical information for its correct interpretation. We admit as a possible explanation for these observations, in addition to those previously mentioned, that clinicians may not be aware of the importance that clinical information has in the request for imaging examinations to the quality of the produced report as well as the utilized protocol, particularly in MRI. Another hypothesis could be the difference in established priorities, with clinicians placing more emphasis on the speed of response to the question they have, rather than on the quality of the report produced, inadvertently providing incomplete information. A third hypothesis could be the unfamiliarity of what is considered relevant clinical information for the radiologist, originating discrepancies in the transmitted information. Regardless of these proposed hypotheses, one solution to this predicament could be the promotion and improvement of communication between radiologists and requesting clinicians,17,18,19through multidisciplinary meetings, for example.
Significant differences were observed between the origin of the examination request and completeness of the provided clinical information. Adequate completion was more frequent in outpatient consultations 1261 (73.4%), while a higher proportion of incomplete filled requests was seen in the outpatient clinic 13 (36.1%), with "diagnostic suspicion / questions to be answered with the study" consistently not properly filled out. The higher proportion of adequate filling of clinical information in outpatient consultation can be attributed to the more peaceful atmosphere of this environment, favouring a more careful analysis of clinical data by the clinician before requesting the examination. The recurring omission of "diagnostic suspicion / questions to be answered with the study" in examinations requested in the outpatient clinic may be related to the patient's follow-up by the attending physician, who may assume that the case is also already known by other professionals, assuming then that it is unnecessary to fill out this field adequately. Also, the complexity of these patients can play a role, with less complex cases tending to have incomplete information. Another factor could be the workload, which can condition non-negligible time constraints.
It is worth noting that there were no cases of absent clinical information in examinations requested at the outpatient clinic. We hypothesize that the absence of requests originating in the outpatient clinic setting missing clinical information can be attributed to the fact that this information is the reason why patients are closely monitored in this environment. As a result, this information is already known by the clinician, allowing him to fill it out quickly and easily in the appropriate mandatory fields.
Our study has some limitations, such as the fact that it was conducted in a single hospital. To our knowledge, there are no other similar studies that explore the relationship between the completeness of clinical information in imaging examination requests according to the imaging technique and the location of the request, in Portuguese hospitals. Due to the similarities in how the hospitals of the National Health Service (SNS) in Portugal operate, it is likely that the obtained results would be comparable with other centres. Other limitations include the retrospective nature of the study and associated pitfalls, the short data collection period (given the workflow varies throughout the year), the non-inclusion of all radiological examination requests in our institution, such as radiographies and neuroimaging studies (as they are not reported by radiologists from our department and the latter being an independent specialty in our country). The subjectivity in the adequacy of clinical information for the requested examination may also be considered a limitation, although partially mitigated by a) the discussion of doubtful cases with the other authors of the study and specialists in Radiology that work in our department, as well as, b) the criterion of considering all filled clinical information that fit into the methodology valid, without considerations regarding its relevance to the requested study. The complexity and diversity of clinical information, as well as the difficulty in interpreting information, sometimes hard to comprehend, are also noteworthy limitations.
We did not set out to assess other factors that may influence the results and therefore should be considered in future studies, such as the clinicians available time for filling out clinical information, nor their knowledge about the information radiologists consider important during the examination request.
Conclusion
This study demonstrates that a substantial proportion of imaging examination requests at our hospital contain clinical information that is either incomplete or entirely absent. This echoes previous studies’ findings that highlighted communication challenges between clinicians and radiologists, specifically in the form of clinical information. The significant number of these requests adds complexity in the radiologists’ interpretation of imaging examinations, which could potentially impact the quality of the produced radiological reports and lead to an underutilization of available resources.
Significant differences were identified in the completeness of the provided clinical information depending on the imaging method and the origin of the request. This information helps us understand current practices and identify areas for optimization through specific measures such as awareness and training programs for physicians on the importance of this topic, as well as the adoption of electronic information systems that facilitate this process. It is also important to highlight the need for radiologists to be open and available for the discussion and clarification of doubts.
We believe the conclusions of this study will have useful implications in improving the quality of health care provided at our hospital.