Introduction
Stroke remains an important source of morbidity and mortality around the world. The majority of strokes are ischaemic in nature and usually due to an intracranial artery occlusion. Until recently, the administration of intravenous thrombolytic therapy was the only standard treatment for acute ischaemic stroke. Today the mainstay of treatment is reperfusion therapy along with intravenous administration of pharmacologic thrombolytic agents. Aiming to get better recanalization rates and because thrombolytic agents are mainly useful in a period of 3 to 4.5 hours, endovascular thrombectomy (EVT) was launched. EVT comprises a wide array of endovascular tools to remove thrombus from the neurovasculature and rapidly restore the blood flow in the ischaemic area.1,2
Primarily, in the setting of an ischaemic stroke, medical centres should try to obtain a noncontrast head CT scan to rule out haemorrhage and to show the presence of a large vessel occlusion. Some of these patients, fulfilling certain additional clinical and imaging criteria, might be candidates for EVT.
EVT was proven to be an effective treatment for proximal occlusions of the major intracranial arteries in stroke patients,3,4 improving outcomes, and recently proved to be effective even after 6 hours.5
Vertebrobasilar strokes are known to be a life-threatening disease and fatal outcome rates of up to 90% have been reported.6 The main treatment of vertebrobasilar strokes has been thrombolytic therapy; however, due to the poor outcomes, EVT is frequently considered, especially in basilar artery occlusions.6
When performing EVT the traditional approach is the transfemoral access, but several risk factors can preclude this approach7 such as vascular anatomy, peripheral vascular disease or aortic dissection. In these situations, alternatives like the transradial, transbrachial or direct carotid puncture techniques are crucial to gain vascular and thrombus access, although they are poorly documented.8,9
We report a case of acute basilar occlusion where a transbrachial approach to revascularization was the preferred approach due to an aortic dissection that precluded the classical transfemoral route.
Clinical Case
A 47-year-old Caucasian male patient, with a clinical history of type A aortic dissection - with previous endovascular stent graft intervention in the ascending and hemiarch aortic segment, ascending aortic aneurysm, previous ischaemic stroke, active smoking and high blood pressure, recurred to the emergency department with left hemiplegia, inability to talk, anarthria, dysphagia, nistagmus and right ataxia, with a National Institute of Health Stroke Scale (NIHSS) of 24. The hemiplegia evolved later and rapidly to tetraparesis.
The initial non contrast CT scan (Fig.1) was negative for acute bleedings or acute ischemic signs - posterior circulation Alberta Stroke Program Early CT Score (PC- ASPECTS) was 10. There was a subtle spontaneous hyperdensity in the basilar artery, possibly corresponding to an acute thrombus. The CT angiography (Fig.1) confirmed a mid-basilar thrombus and additionally an arterial dissection involving the aortic arch and the left common carotid artery. The supra-aortic vessels were supplied by the true and false lumina. The right vertebral artery was hypoplastic, ending in an ipsilateral posterior inferior cerebellar artery. Thrombolysis with rtPA was then performed (165 minutes after the beginning of symptoms) and the cardiothoracic surgeon was contacted, who immediately contraindicated the EVT transfemoral approach, due to the risk of extending the dissection into the abdominal aorta and the false lumen.
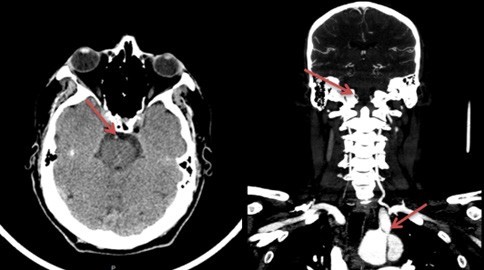
Figure 1: In the initial head CT scan (left) there were no major ischemic or hemorrhagic signs, the PC-ASPECTS score was 10. Hyperdense basilar artery was noted (arrow). In the CT angiography (right) a right vertebral artery ending in the ipsilateral posterior inferior cerebellar artery (upper arrow) and an arterial dissection extending between the aortic arch and the left common carotid artery are seen (lower arrow).
Emergent EVT was performed 5 hours after stroke onset, under general anaesthesia, using a 6F sheath left transbrachial approach. Left vertebral artery catheterization through the subclavian artery took place and the thrombus was removed after 1 retrieving attempt using the stent Trevo ® 6x25mm. Total revascularization of the occluded arterial territory was achieved in 15 minutes after puncture - thrombolysis in cerebral infarction (TICI) 3 score (Fig.2). There were no peri-procedure clinical or technical complications.

Figure 2: Digital subtraction angiography in AP view, before (arrow: basilar occlusion) (left) and after endovascular thrombectomy (right). Total revascularization of the occluded arterial territory was achieved - thrombolysis in cerebral infarction (TICI) 3 score.
There were no acute ischemic or bleeding signs in the 24h control CT scan and in the MRI there was only a small recent ischaemic area in the right anterior paramedian pons (Fig.3).
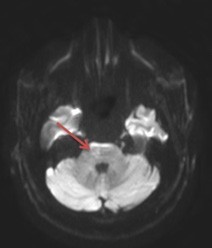
Figure 3 In the reevaluation MRI there was a small recent ischemic area in the right anterior paramedian pons (Axial Diffusion Weighted Imaging B1000; arrow). The neurological deficits were reversed - NIHSS =0.
The patient was transferred to the neurovascular unit ward with a normal and spontaneous ventilation, oriented, conscious and punctuating 1 in the NIHSS (slight dysarthria). Next day he was asymptomatic and without focal neurologic signs.
In the stroke unit the medical team underwent the clinical investigation: the blood tests had no major alterations, the vascular Doppler showed mild atherosclerosis in the right carotid artery and the dissection in the left carotid artery. Holter monitoring revealed bigeminy periods and T wave inversion and depression in V5.
The thorax/abdominal/pelvic CT angiography confirmed the intimal flap in the aortic arch and initial descendent segment, which was partially thrombosed, with communication between the true and the false lumen. The dissection progressed into the common left carotid artery and there were also small dissection segments in the initial brachiocephalic trunk and left subclavian artery. A marked aortic dilatation was seen in the ascending segment with a maximum diameter of 6.5 cm. There wasn’t any intracardiac thrombus. There were ischemic changes in the left kidney, pointing to an embolic origin.
The transesophageal echocardiography showed an atrial septal defect, ostium secundum, with right atrial enlargement, that possibly also supported an embolic origin.
The patient was discharged 15 days after stroke onset (NIHSS 0) and started anticoagulation therapy with warfarin (INR target: 2-3). In the following medical appointments (at 10 and 19 months) the patient remained asymptomatic, without neurologic sequelae or new strokes.
Discussion and Conclusion
EVT for large ischaemic stroke has been one of the most powerful treatments in any field of medicine, if the patient fits the most recent guidelines.10
In this modern era of endovascular treatment for large vessel occlusion in patients with an acute ischaemic stroke, a clear priority is to minimize time to revascularisation, because “time is brain”.
When performing EVT the transfemoral access has been the standard route and remains the most frequent approach, given its familiarity, easy accessibility,11 allowing unlimited repetition of puncturing, the use of larger sheaths and less radiation and contrast time.12 However, in some cases, when patients harbour challenging vascular anatomy, it can be technically difficult and time consuming, and this delay in catheter access and revascularization may be associated with worse prognosis.9 Other disadvantages are higher risk of bleeding and hematoma formation, especially in patients using anticoagulation (groin hematoma formation rate with transfemoral access reported to be as high as 10%),12 pseudoaneurysm, fistulae formation, vessel occlusion13 and the need to stop/readjust antiplatelet or anticoagulation treatment after angiography in patients at risk for atherosclerotic or cardioembolic disease.
Alternative routes such as the transradial, transbrachial or carotid artery direct puncture, should then be considered in order to gain vascular access and optimize delivery of thrombectomy devices.
There is evidence in the interventional cardiology field demonstrating safety and advantages of the transradial approach.14 This route has fewer major access site complications and similar procedural and clinical outcomes, compared to the other two modalities.15 The advantages of this method are easier compression/hemostasis and thus quick Hospital discharge, reduced costs, fewer bleeding and vascular complications (e.g. pseudoaneurism formation) and reduced injury risks because no major nerves or veins are located near the radial artery. Despite its large number of benefits it is not always feasible, it requires a longer learning curve for the operator, increased X-ray exposure time, increased pain during the procedure, possibility of radial artery spasm or occlusion, branch vessels can be difficult to catheterize, continued access in the same arm is limited, devices having dimensions and specifications for radial access are lacking,14 sheath kinking can occur16 and, in patients with anomalous palmar arch, there may be insufficient blood supply at hand in cases of thrombotic, spastic or traumatic occlusion of the radial artery.12
It has been demonstrated that the brachial approach17 may have more complications compared to the transradial or femoral approaches, with reported overall access site complication rate for noncoronary procedures of 11%.12,15 Some of the disadvantages are increased risk because major nerves/veins are located near the brachial artery, repetition of puncturing is limited and it is more difficult to compress, consequently leading to vascular/bleeding consequences and longer Hospital stay.
In this particular case the brachial route was chosen instead of the radial one because the brachial artery caliber looked more favorable (anticipating the need to introduce a larger- bore catheter12 (8F) to aspirate, if stent retriever failed), due to the interventionist personal experience and preference and also because Allen’s test was inconclusive. Additionally, because the distance from the brachial artery to the subclavian artery is smaller and straighter, this technique can offer a more stable support for the guiding catheter.12 Concerning direct carotid artery access, in this setting of stroke management, the main advantage is the ability to bypass the anatomically unfavourable areas, shortening the time to reperfusion. In our clinical case, being a basilar artery territory, the carotid route was not considered.
Although not well documented in the neuroendovascular field, neuroradiologists have been slowly adopting these brachial and radial approaches, learning mainly from Cardiology. These routes have been reported as safe and feasible, reducing retroperitoneal haemorrhage since intravenous thrombolysis is often administered concurrently and allowing patient recovery sooner.9,16,18,19 Also, there are recent reports14 showing no difference in single-pass recanalization rate, number of passages, mean access to reperfusion time, successful revascularization rates and functional outcomes between transradial and transfemoral approaches, particularly in patients whose aortic arch anatomy would present a challenge. Joshi KC et al.14 have showed that the transradial access has a high rate of procedural success (95.23%) with low complication rates (2.90%) when used for various neuroendovascular interventional procedures. Lee et al.12 also showed that the transradial or brachial access modalities are good alternative access routes for various neurointerventional procedures. Actually they accomplished almost all kinds of interventional procedures with a high success rate except for cases of carotid stent insertion.
In this case, the patient presented an important contraindication - type A aortic dissection - and also a right vertebral artery ending in the ipsilateral posterior inferior cerebellar artery. There was no other option but to use the transbrachial or radial approach on the left side. Time was crucial to give the patient the proper treatment. Having a previous supra-aortic vessels CT angiography, EVT was rapidly planned and successfully executed and the patient, who was tetraparetic, started walking the very same day after arterial revascularization was obtained. At the end of the procedure, he punctuated 1 in NIHSS (slight dysarthria) and, at discharge, he had a NIHSS of 0, without neurological deficits.
In a time when alternative techniques are undergoing growing adhesion and familiarity in the neuroendovascular field, we recognize that future studies should focus on early and effective triage of patients most likely to require alternative EVT approaches to reduce their morbi-mortality rates, particularly when posterior circulation strokes occur. Interventional neuroradiologists should become familiar with alternative access routes like radial and brachial artery access in order to provide comprehensive endovascular care to their patients.















