Introduction
Multiple pregnancies (MP) account for about 3% of the live births and increase the risk of maternal, fetal and neonatal morbimortality1. Their incidence has risen in developed countries, mainly due to the spread of assisted reproduction techniques (ART). Up to 26% of successful in vitro fertilization (IVF) procedures result in MP1,2.
MP increase the risk of miscarriage or stillbirth, preterm delivery, fetal growth restriction or complications related to chorionicity1,2, which is even higher in triplets comparing to twins. As an example, triplet and higher-order pregnancies more than double the stillbirth rate comparing to twins1. Therefore, efforts have been made to decrease its incidence, namely by reducing the number of embryos transferred with each IVF2.
In triplet pregnancy the mean gestational age at delivery is 32-33 weeks and around 75% of neonates require admission to the neonatal intensive care unit (NICU)1 3. The risk of spontaneous preterm delivery (SPD) <32 weeks may be predicted by sonographic screening of cervical length4-6. Once cervical shortening is diagnosed, the main challenge is to decide the best clinical approach since no intervention has been shown to improve the outcomes in this population.
The authors describe a case of a triplet gestation with pronounced mid-trimester cervical shortening. The pregnant underwent an ultrasound-indicated cervical cerclage and delivered three newborns at the 28th gestational week. The selected approach and the controversies around it will be briefly discussed.
Informed consent was obtained from the patient.
Case report
A 39-year-old patient, primigravida, with tubal factor infertility and a triplet gestation by IVF (2 embryos transferred 5 days after IVF) was referred to our obstetric department for pregnancy surveillance. She had no other relevant medical history. The first trimester ultrasound revealed a dichorionic triamniotic gestation, with anatomically normal fetus. Since it was a gestation by ART, vaginal progesterone was prescribed during the first trimester.
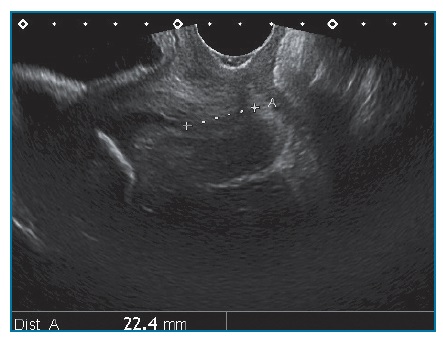
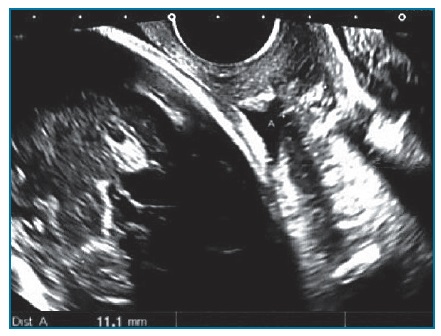
The cervical length was screened by transvaginal ultrasound, measuring 3cm in the first evaluation (15th gestational week). A week later, cervical shortening was detected, measuring 2,2cm (Figure 1). The pregnant was advised to restart vaginal progesterone (200mg at night) and reduce physical activity, including dispense of her professional activity. Blood analysis with inflammatory parameters, urine culture and cervicovaginal swab were performed with no abnormal findings. There was a progressive and significant asymptomatic cervical shortening, with U-shaped funnel, reaching 0.5cm at the 20th week (Figure 2 A, B). After discussing the poor prognosis and the controversial obstetric interventions, the parents asked for cervical cerclage. A McDonald cerclage was performed (20+2/7 weeks) with no intercurrences, promoting a partial restoration of cervical length (1cm) with no funneling above suture. Serial obstetric ultrasound ensured normal fetal growth, morphology and well-being.
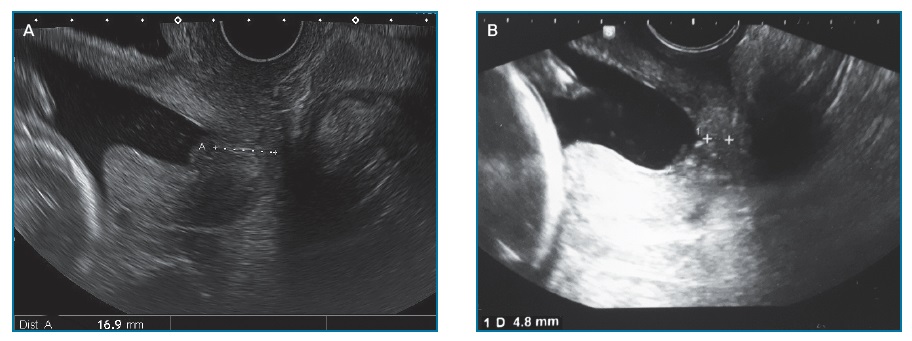
Figure 2 Cervix evaluation at 18th gestational week, measuring 1.7cm (A), and at 20th gestational week, measuring 0.5cm (B)
At the 25th week, the pregnant was admitted for inpatient surveillance due to maternal anxiety, with no obstetrical indication for hospitalization. Although asymptomatic, she felt more secure with this approach. Vaginal exam was avoided and daily tocography revealed no asymptomatic uterus contractions.
Three weeks later, the cervix remained unchanged (Figure 3). An obstetric ultrasound on prenatal diagnosis department was scheduled to 28+5/7weeks and antenatal corticosteroids would be performed after that.
At 28+4/7weeks, the pregnant started regular and painful contractions, with no fever, fetal tachycardia or rupture of membranes. Tocolylisis, betamethasone and magnesium sulfate for neuroprotection were immediately given. Two hours later, she remained symptomatic and the cervix was 4cm dilated, compromising the cerclage which was removed. An urgent cesarean section was performed, delivering two male and one female newborns weighing 1300, 1088 and 1065 grams, with Apgar scores of 6/8/9, 6/8/8 and 6/8/8, respectively. All of them required ventilator support immediately and during the first days of life. Placental histopathology revealed signs of acute chorioamnionitis in both placentae.
The newborns’ clinical response was appropriate for their prematurity and very low birth weight, namely with sustained hemodynamical stability, no severe complications, no evidence of infection or cerebral injury. They were discharged on the 50th postpartum day.
Discussion
An ultrasound-indicated cerclage in triplet pregnancy is a rare and controversial approach. The authors discuss the management of this exceptional case and resume the current literature.
The risk of SPD <32 weeks gestation is one of the biggest concerns in triplet gestation. It may be predicted by serial sonographic cervical length evaluation, but there is limited data on the optimal timing and frequency of surveillance in triplets4-6.
In asymptomatic women with twin pregnancy, cervical length measurement at 20-24 weeks of gestation is considered a good predictor of SPD5. Some authors tried to stablish that association for triplets. In those cases, a cervical length of ≤2.5cm by transvaginal ultrasound seems to predict SPD <32 weeks, although different gestational ages for screening were suggested6,7. Some proposed a cervical length of ≤2.5cm at 21-24 weeks as a good predictor for SPD, with an 86% sensitivity for delivery at <28 weeks7. Others reported a predictive value when the screening was performed at 16-20 weeks, with an increasing odds of SPD <32 weeks by 43% for each 1cm decreased in cervical length6. Cervical shortening also seems to predict an increased risk of lower birth weight and lower Apgar scores4,8.
Once mid-trimester cervical shortening is diagnosed, the main issue is to decide the clinical approach. Although vaginal progesterone or cervical cerclage can be offer to singleton pregnancies9, there is no evidence to support their indication in MP2,5. There is insufficient and conflicting data due to the small number of trials, with small cohorts and heterogeneous inclusion criteria. Other controversial alternative could be the use of Arabin pessary. It has been studied in twin pregnancies with short cervix and some trials report reduction in SPD5. However, the available evidence still conflicting5 and to our knowledge there are no studies in triplets. In the present case, that option was also discussed with the parents, although the Obstetric team admitted lack of experience with pessary use.
In twin pregnancies, most studies suggest no usefulness of ultrasound-indicated cerclage (cervical length ≤2.5cm before 24 weeks gestation) and a possible adverse effect on neonatal outcomes2,5. However, recent retrospective cohort studies evaluating the impact of cervical cerclage in twin pregnancies with asymptomatic short cervix have shown promising results, such as possible reduction of SPD <32 weeks10-13.
Studies in triplets are more limited and smaller. Some authors tried to assess the efficacy of prophylactic cerclage but failed to prove any benefit, namely in gestational age at delivery, birth weight, rate of live birth or admission to NICU3,14. There is also no proven benefit of emergency or ultrasound-indicated cerclage4,14.
In this report, a cervical shortening was identified from the 16th gestational week, with U-shaped funnel and fast progression. The parents were informed about the poor clinical prognosis, with high probability of late miscarriage or extreme prematurity, and the absence of evidence supporting the performance of cervical cerclage in triplets. However, considering the parents’ determination to perform it, the obstetric team chose to uphold their decision. The final outcomes seem to approach the published results of ultrasound--indicated cerclage. A retrospective study evaluating 24 triplets with short cervix, which were managed expectantly or with cervical cerclage, reported a mean gestational age at delivery of 29+3-5/7weeks and more than 60% of very low birth weight newborns in both groups, with no differences in other outcomes8. The authors did not specify cervical characteristics, but a previous analysis of the same cohort (only 13 cases) reported a mean cervical length of 1.6cm and a mean gestational age of 20+2/7weeks at the time of cerclage placement4.
Vaginal progesterone was provided as an effort to extend the latency period. In unselected women with MP, it does not reduce the incidence of SPD2. Nevertheless, given its role in maintenance of uterine quiescence, progesterone is biologically plausible in selected cases. A meta-analysis reports possible benefits in twin pregnancies with short cervix15.
The corticosteroids’ treatment for fetal maturation is other concern in triplets. In singleton pregnancies at risk of imminent labor <34 weeks gestation, antenatal corticosteroids are strongly associated with decreased neonatal morbimortality, namely for respiratory distress syndrome9,16,17. These benefits seem to be transient, with greater effect at 1-7 days after the initial dose16,17. Therefore, it is recommended to offer a single course of corticosteroids for pregnancies between 24+0/7 and 33+6/7weeks at risk of preterm birth within 7 days9,16,17.
In MP several studies fail to prove significant benefits of antenatal corticosteroids in neonatal outcomes17,18. Further research is needed to clarify if corticosteroids bioavailability is reduced in MP or if the lack of stablished efficacy is mostly due to the small and low quality data17-19. On the other hand, prophylactic corticosteroids frequently implies multiple doses, which may increase its potential adverse effects, with no proven beneficial effects comparing to the rescue approach18,20,21. Therefore, the current recommendations for antenatal corticosteroids in MP are the same made for singletons. Prophylactic or repeat courses are not recommended, with the exception of a single second course in specific clinical scenarios1,2,17.
In this case, weighing the clinical stability and the high-risk of preterm delivery, corticosteroids administration was planned to 29th gestational week. These timing seemed reasonable to achieve the optimal therapeutic window or to repeat only a rescue course until delivery. Unfortunately, due to the rapid cervical progression, there was no time to promote the corticosteroids therapeutic effect.
In conclusion, early preterm delivery is one of the biggest concerns in triplet pregnancies. Obstetricians can predict it by screening for short cervix but obstetrical interventions to improve neonatal outcomes are still missing. The authors believe that cervical cerclage had a good performance in this case, given the fast and pronounced mid-trimester cervical shortening. Considering the current limited evidence, a case-by-case evaluation based on cervical shortening progression and a conscious parents’ decision seems to be a reasonable approach. A clear explanation about the procedure’s risks and unproven benefits in triplet gestations is essential.