Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Psicologia, Saúde & Doenças
versão impressa ISSN 1645-0086
Psic., Saúde & Doenças vol.16 no.1 Lisboa mar. 2015
https://doi.org/10.15309/15psd160209
Weight management program based on self-determination theory: comparing parents-child data
Programa de gestão do peso baseado na teoria da auto-determinação: comparação de dados de pais-filhos
S.Veloso1, , M.G.Matos2,4,5, A.Palmeira1, S.Martins1, H.Fonseca3, & J.A.Diniz4
1 Faculdade de Educação Física e Desporto, da Universidade Lusófona de Humanidade e Tecnologias, Lisboa, Portugal;
2 ISAMB / Universidade de Lisboa, Portugal;
3 Departamento da Criança e da Família do Centro Hospitalar de Lisboa Norte, Portugal;
4 Faculdade de Motricidade Humana da Universidade de Lisboa, Portugal;
5 WJCR /ISPA, Lisboa, Portugal
Endereço para Correspondência
ABSTRACT
This study aimed to analyze the changes in self-regulation, basic psychological needs, staff and parents support after the first 4-months of a weight management program with adolescents. To improve our understanding about the clinical implications, we also analyze the participants' views (adolescents and their parents) about the program.
The 24 overweight adolescents (31 ± 4.9 kg/m2; 17 girls; 13,2 years), followed in a tertiary health unit, participated in a 4-month program with structured exercise, eight educational sessions on behavioral change and parental involvement. We measured the perception of staff and parental support, self-regulation for treatment, basic psychological needs at 0 and 4 months. At 2,5 months 20 adolescents and 16 parents participated in focus groups to analyze the impact of the program.
There were improvements in relatedness satisfaction, but not in weight. The adolescent’s opinion found the exercise as the main strength of the program, but for parents was the personalized and group format; for both parents and sons the main weakness of the program was the disillusionment with weight loss. The discussion suggests that the weight loss treatmentbased on exercise and self-determination theory principles could bring psychological benefits even without weight loss.
Keywords- adolescents; weight management; self-determination theory; exercise
RESUMO
A desafiante intervenção na obesidade pediátrica motivou um estudo quantitativo e qualitativo sobre os aspetos psicossociais num programa comportamental baseado no exercício físico com adolescentes e envolvendo os seus pais. Os 24 adolescentes (17 raparigas) com excesso de peso (31 ± 4,9 kg/m2), com 13,2 anos em média, seguidos na consulta dum hospital, participaram num programa de 4 meses que incluiu exercício físico estruturado, oito sessões educativas sobre mudança comportamental e envolvimento parental. Mediu-se a percepção do suporte da equipa técnica, a autoregulação para o tratamento, as necessidades psicológicas básicas e a percepção do suporte parental,aos 0 e 4 meses. Aos 2,5 meses 20 adolescentes e 16 pais participaram voluntariamente em grupos focais analisando o impacto do programa. Verificaram-se melhorias na satisfação da necessidade de relacionamento, mas não no peso. Na opinião dos filhos o exercício é a principal força do programa, mas para os pais é o formato personalizado e em grupo; sendo a desilusão com a escassa perda de peso uma fraqueza para ambos.A discussão compara os dados quantitativos com e as opiniões convergentes e divergentes de pais e filhos, reforçando a pertinência do exercício e da teoria da auto-determinação para a intervenção na obesidade, por trazer benefícios psicológicos mesmo sem perda de peso.
Palavras-chave: adolescentes; gestão de peso; teoria da auto-determinação; exercício
Obesity in children and adolescents has become a serious threat to public health. The environmental and lifestyle challenges led weight problem to epidemic proportions. Governments are concerned but research in young people has provided little evidence on what to base interventions (Flynn et al., 2006; Larson & Story, 2008; Sinha & Kling, 2009; Tsiros, Sinn, Coates, Howe, & Buckley, 2008).
The scientific evidence for what works best in the management of child and adolescent overweight and obesity shows that combined behavioral lifestyle interventions, compared to standard care or self-help, can produce a significant and clinically meaningful reduction in overweight (Finkelstein & Trogdon, 2008; Luttikhuis et al., 2009; Tsiros et al., 2008; Whitlock, O'Connor, Williams, Beil & Lutz, 2008; Wilfley et al., 2007). Although, patient non-attendance, drop-out and widespread failure to achieve weight maintenance, characterized treatment for pediatric obesity (Stewart, Chapple, Hughes, Poustie & Reilly, 2008b). Specific strategies should educate parents about healthy behavior patterns through modeling, avoiding strict dieting, using food as reward or punishment, setting limits of acceptable behavior; and promoting healthy intra family communication patterns which support adolescentsself-esteem (August et al., 2008).Qualitative methods may improve our understanding of patient perceptions thus improve treatment for childhood obesity (Styles, Meier, Sutherland & Campbell, 2007).
A growing body of research supports self-determination theory (SDT) (Deci & Ryan, 2002; Ryan, Patrick, Deci & Williams, 2008) as a comprehensive model to understand mediators of behavior change and maintenance (Deci & Ryan, 2002; Ryan et al., 2008), also in the context of weight loss (Williams, Grow, Freedman, Ryan & Deci, 1996). SDT is an empirical theory of motivation, development and wellbeing which is concerned with social-contextual conditions which facilitate the natural processes of self-motivation and healthy psychological development (Ryan & Deci, 2000). Authors identified three innate psychological needs for growth and personal wellbeing (Deci & Ryan, 2002; Ryan et al., 2008): autonomy (feeling volitional, choice and responsibility), competence (feeling that one can accomplish and reach the goal) and relatedness (feeling understood, cared, valued by significant others). According to SDT there are two main types of motivation: the autonomous motivation is an expression of one's self and is undertaken with a full sense of choice, accompanied by an internal perceived locus of causality; the controlled motivation, although intentional, is experienced as pressure or coercion (internal and/or external), accompanied by an external perceived locus of causality (Deci & Ryan, 2002; Ryan & Deci, 2000). This distinction represents a continuum from a more controlled behavior regulation to a more autonomous, characterized in terms of degree to which regulation of behavior has been internalized so that it is engaged in with a true sense of volition and choice (intrinsic motivation). Finally, the need to promote adherence to non-intrinsically motivated behaviors (e.g. eating vegetables, exercise), led SDT researchers to findthree dimensions of social environment which facilitate behavior change. These require authority figures (e.g. parents, teachers, doctors, exercise instructors, nutritionists): listening with empathy, recognizing that change is demanding and challenging for participants, providing choices and rational for change without pressure (support for autonomy), providing accurate and realistic feedback about the outcome of behavior and contingencies (structure) and taking genuine commitment to support participants and their wellbeing (involvement). These strategies together are likely to promote autonomous motivation, satisfying psychological needs, discouraging controlled behavior (Wilson, Mack, & Grattan, 2008).
Factors of obese children’svulnerability to low self-esteem were reviewed (Lowry, Sallinen, & Janicke, 2007) and showed the importance of basic psychological needs and interpersonal context: beginning of adolescence, being a girl, identity with high slim standards, bullying, parental control of food, and self evaluations related with body weight. The factors which promote self-esteem were weight loss, parental involvement and group intervention (Stewart, Chapple, Hughes, Poustie, & Reilly, 2008a). Parents’ motivation to enter in a program were the perceptions of benefits on self-esteem, quality of life and children’s wellbeing (Stewart et al., 2008a).
Some qualitative studies expressed the importance of SDT principle by the point of view of participants. Adolescents express autonomous reasons to weight management as more efficient strategies: more physical activity; more consumptions of fruits, vegetables, water and less “fast food”; but didn't want to give up of soft drinks, TV and video games (Wilson, 2007). Interviews with 50 adolescents (13-16 years old) showed their awareness of unhealthy behaviors, a lower adherence to health diet, sufficient physical practice butlack of fitness (Lindelof, Nielsen, & Pedersen, 2010). They blamed themselves for obesity, but also blame their parents because they didn't support their physical practice and healthy diets. On the other hand, parents blamed his sons for their lack of motivation to adopt healthy behaviors, bringing a familiar climate of disagreement and negative feelings (Lindelof et al., 2010).
In the health care context, SDT considers that maintenance of behaviors over time requires that patients experience self-determination and internalize values and skills for change. It is by maximizing the person’s experience of autonomy, competence, and relatedness in health-care settings, that self-regulation of health behavior is more likely to be internalized, and behavior change will be better maintained (Williams et al., 1996).The model of self-determination health behavior (Ryan et al., 2008)states that the autonomy-supportive health care contexts, the personality differences in autonomy, and intrinsic vs. extrinsic nature of life aspirations can influence the individual’s experience of his basic needs, which impact on the health related outcomes and well being, such as greater intake of fruits and vegetables, or more physical activity.
This study tried to focus on SDT mediators in the context of adolescents’obesity. The goal was to analyze the changes in self-regulations, basic psychological needs and adolescents’ perceptions of their parents’ support, after the program. With focus groups we wanted to highlights their needs and find clinical implications for better weight management programs.
METHODS
Quantitative Study
Participants
Participants were overweight and obese adolescents (n=33),followed at an outpatient clinic (a tertiary unit of a public hospital) that accepted to participate in the study. Of these, ninewere subsequently excluded from all analysis becausethey failed educational sessions. Theninedropout adolescents had similar age (p=0.49), gender (p=0.27) and BMI (p=0.46) just as the 24 participants considered as the valid initial sample.Of these, sevenwere boys and 17 girlsbetween 10 and 17 years hold (13.6 ± 2.1 years) and were an initial BMI of 31.0 ± 4.9 Kg/m2. Retention rates were 75.8%.
Material
The Perceived autonomy supportof healthcare providers (Climate) was measured with The Health Care Climate Questionnaire, HCCQ (Williams et al., 1996), which analyzes the degree to which we perceive health care providers to be autonomy supportive. With 15-item, a 7-point scale and internal consistency of 0.93.The Treatment self-regulation was assessed with two versions of the Treatment Self-Regulation Questionnaire, TSRQ(Levesque et al., 2007; Williams, Freedman & Deci, 1998; Williams et al., 1996)that evaluates the reasons to initiate a weight-loss program and the reasons to stay in the program (autonomous vs. controlled). With 18 items and a 7-point scale, participants were asked to evaluate how well each statement represented their reasons to start the program (e.g. of autonomous self-regulation was “I decided to enter this weight-loss program because I really want to make some changes in my life.”). The other version (reasons to stay) had the same structure but consists of 13 items and assesses the person’s motivation for staying in the program (e.g. of controlled self-regulationwas “I have remained in treatment because I would have felt bad about myself if I didn't”). The internal consistency of twoversions for both subscaleswas respectively: autonomous (α=0.70 and α=0.90)and controlled (α=0.87 and α=0.77) self-regulation treatment.
The Psychological needs - competence, autonomy and relatedness - were measured with Basic Psychological Needs Scale, BPNS (Baard, Deci, & Ryan, 2004) that addresses need satisfaction in general in one’s life. The scale had 21 items, 6 items for competence (e.g. I have been able to learn interesting new skills recently), 8 items for relatedness (e.g. I really like the people I interact with), and 7 items for autonomy (e.g. I feel free to decide for myself how to live my life), to which participants responded on 5-point scale. The Cronbach’s alpha was respectively for baseline and after four mounts: competence 0.55 and 0.72, relatedness 0.68 and 0.88; autonomy 0.53 and 0.57 (excluding item 1 and 20). Adolescent’s perceptions of their parents support was measured with the college-student version of the Children's Perceptions of Parents Scale, POPS (Grolnick, Deci, & Ryan, 1997). This scale assesses adolescents’ perceptions of their parents’ autonomy support, involvement and warmth. With 42 items: 21 for mothers and 21 for fathersto which participants responded on 1-5 point Likert scale. From these items resultedsix subscale: Mother Autonomy Support, Mother Involvement, and Mother Warmth (baseline 0.67<α <0.81; after four month 0.65<α <0.75), as well as Father Autonomy Support, Father Involvement, and Father Warmth (baseline 0.68<α <0.86; after four month 0.62<α <0.81).
Exercise/physical activity: Minutes per week of leisure-time of moderate and vigorous physical activity were estimated with the 7-Day Physical Activity Recall interview (Blair et al., 1998). Regular activities with a metabolic equivalent task (MET) value above 3.0 and performed during the last seven days (or on a typical week of the past month) were quantified to produce four variables: Minutes per week of physical activities in leisure-time or transport (MinPA); Energy expenditure per week of that physical activity (EExpPA); Minutes per week of structured physical exercise (MinPE), and Energy expenditure per week of that structured physical exercise (EExpPE). Body mass index (BMI) was calculated by the formula kg/m2.
Weight was measured usingan electronic scale (SECA model 770, Hamburg, Germany).
Procedure
The study was quasi-experimental. In addition to intervention through hospital consultations (three consultations during four months) the intervention group and their caregivers participated in a four months program which comprised up to three sessions of exercise per week in addition to lifestyle physical activity recommendations; the adolescents and their parents participated in eight biweekly educational and interactive sessions (90 minutes) on motivation and behavior change, physical activity, nutrition and self-image (in five of the sessions adolescents were separated from caregivers). The focus groups with participants were conducted after 2.5 months. The program’s principles were based on SDT: the interactive sessions, the exercise training and the physical activity consultations (with staff training) followed these principles, particularly with motivational interview techniques as autonomy support. The study was approved by an ethics committee of hospital’s Children and Family Department and followed strictly the Helsinki Declaration of Human Rights. Informed consent was obtained for all subjects.
Subjects completed questionnaires prior to the first weekly program and again after the last session (four months later), following a standard protocol.
Qualitative study
Participants
Twenty of the 24 adolescents participated in focus groups (one of 11 adolescents, 7 girls; other of nine with 6 girls) with the same mean age and BMI of the quantitative sample. Sixteen parents participated in two focus groups: one with seven (one father), other with nine (two fathers).
Material
A focus group is a discussion-based interview which involves the simultaneous use of multiple respondents to gather data on a certain issue (focus) (Lambert, Hublet, Verduyckt, Maes, & Van den Broucke, 2002). This method allows to collect information on the views, beliefs, and values of a group's participants (Calderon, Baker, & Wolf, 2000).To know the parents and adolescent’s opinions about the program the main topics were: motives to adherence; perceptions about program components and itschanges inweight, physical activity, nutrition, body image and psychological wellbeing; difficulties; parents and peer support; proposes for a better program.
Procedures
The collective interviews were conducted with parents and adolescents who voluntarily agreed to participate after 2.5 months of the program. After the purpose of the study presented, it was noted that there was no wrong answers, the results would be anonymous, and informed consent was obtained. We performed an icebreaker activity for uninhibited participants and introduced the topics in an open style of moderation, allowing freedom of expression. Each interview (60-90 minutes) was recorded and later transcribed in full for subsequent data analysis. The Ethics Committee of the Lusófona University approved the study.
RESULTS
Quantitative results
The differences between the baseline and four months’ values were analyzed with non-parametric Wilcoxon Testand were presented in the Table 1. There were no significant differences between gendersat baseline and after four monthswith nonparametric Mann Whitney Test.
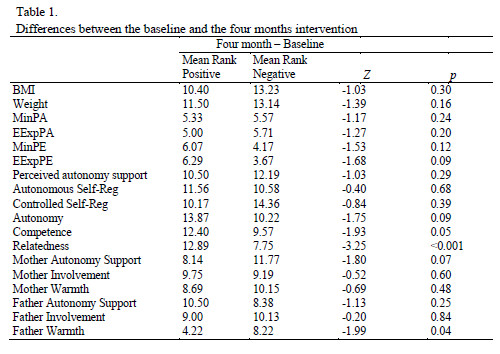
A linear regression analysis (with the adjusted residuals) with the variable EExpEF and both self-regulations was used to findsome BMI predictors. There was no significant result (p>0.05).To explore possible predictors of relatedness, the regression analysis showed two significant predictors in the first model, autonomous self-regulation (B =-0.65; p=0.02) and controlled self-regulations (B = 0.60; p=0.03); perceived autonomous supports (n.s). This model explained 38% of variance to relatedness (R2Aj=0.38; Error=0.84; F(3, 9)=3.45; p<0.06).The second model added the parents’ support variablesas relatedness predictor, but there was no significance.
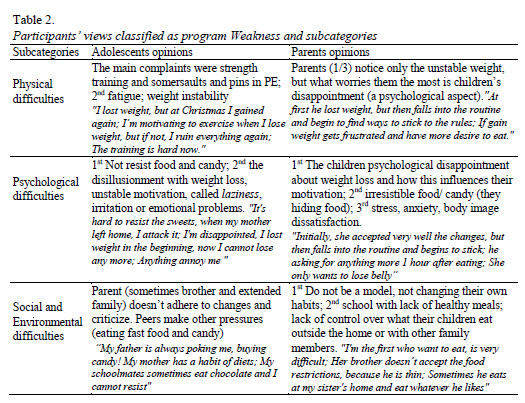
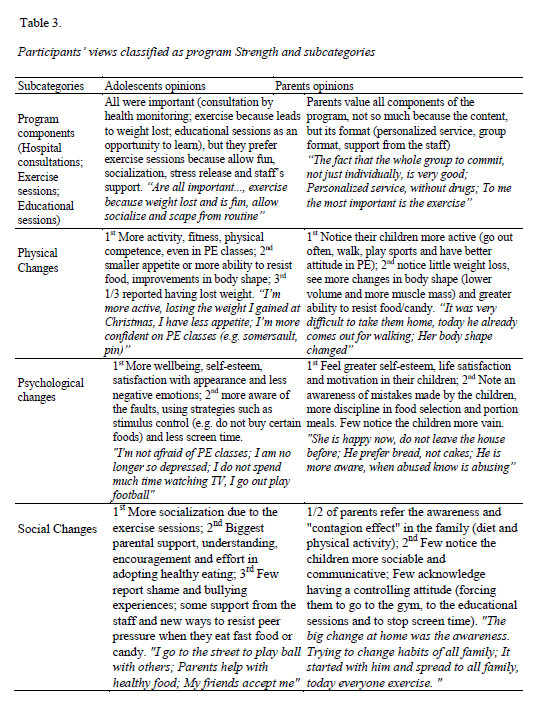
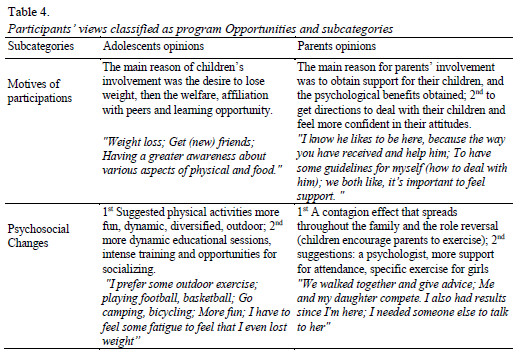
Qualitative results
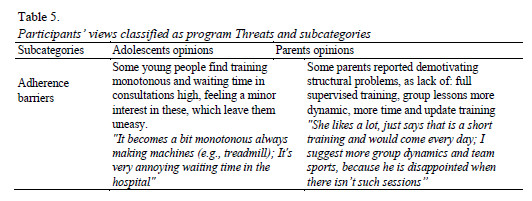
The data analysis of content was performed by a technique of thematic or categorical analyze (Bardin, 2004), but with the SWOT model to find the principles categories. The SWOT model is a structured planning method used to evaluate the Strengths, Weakness, Opportunities, and Threats involved in a program. Health managers have been applying this model to find self-regulating strategies for health care organizations and obtained gains in the efficiency of the services (Camden, Swaine, Tetreault, & Bergeron, 2009; van Wijngaarden, Scholten, & van Wijk, 2010).The data from the focus groupswasclassified into the four SWOT categories. From the report sent back by the three independent judges (researchers in pediatric obesity) it was possible to classify the results into 10 sub categories common to parents and adolescents. The data presented here reflects all the features brought up in the discussions, taking into account the most frequent responses and the criteria of Bardin (2004): completeness, uniqueness, objectivity and relevance to the study goal. The selection of the parents and adolescents’ opinions for each subcategory followed the same criteria. The results were presented in four tables here is possible to compare both participants’ opinions (see Table 2, 3, 4, 5).
DISCUSSION
In the context of weak scientific evidence and limited clinical results in the treatment of pediatric obesity, recent reviews have recommended studies considering psychosocial variables to identify moderators and mediators of interventions that could produce sustainable change. The growing interest in qualitative research, to understand the needs of overweight children and their parents, to promote interventions efficacy, also motivated our work. This study analyze quantitative and qualitative data: the changes in some SDT psychosocial mediators, empirically supported (Williams et al., 1996), four months after a weight-management program based on exercise with obese adolescents outpatients; and the participants opinions about the program, collected from focus groups after 2,5 months, to explore quantitative data and clinical implications.
The lack of a significant change in weight and BMI after four months was a motive of deception by both parents and adolescents (notice soon after 2,5 months). The vast majority of studies with adolescents show the absence of significant weight loss or a small to moderate short-term improvements (Field, Haines, Rosner, & Willett, 2009; Whitlock et al., 2008). On the other hand, the subjects were adolescents referred by a tertiary health unit, who failed previous weight loss attempts, a negative moderator of the effects of treatment on women (Teixeira, Going, Sardinha, & Lohman, 2005), which can explain the lack of effects that we found on weight loss. Both participants recognized the importance of all program components (consultations, exercise and educational sessions), and this seemed positive to the adherence of the combined behavioral lifestyle interventions who showed scientific evidence (Finkelstein & Trogdon, 2008; Luttikhuis et al., 2009; Tsiros et al., 2008; Whitlock et al., 2008; Wilfley et al., 2007).
The improving of relatedness was the most significant result obtained. The relatedness need satisfaction, as the feeling of a meaning connection with others may have been fostered by the gradual positive interaction with staff, family members and peers. Both participants testified it, because they preferred the exercise sessions by fun and socialized opportunity, wellbeing, stress relieve and staff support. The psychosocial benefits from exercise are very supported from literature (Biddle & Mutrie, 2008). On the other hand, this result could support the staff commitment to the SDT principles that facilitate the satisfaction of psychological needs (Ryan et al., 2008). Additionally, the positive climate and fun in exercise sessions could promote intrinsic motivation and probably the autonomous regulation; the socialization between peer and the staff could promote the relatedness (Deci & Ryan, 2002; Ryan & Deci, 2000).
It seems there was not enough time in the program to foster autonomous self-regulation and to decrease the controlled self-regulation as expected. SDT states that controlled motives have been associated to the initial change, as initial adoption of physical activity (Ingledew, Markland, & Medley, 1998), whereas autonomous motives have been associated to stage progression and maintenance of health behavior over time as weight loss (Williams et al., 1996) and lifestyle change (Ryan et al., 2008). Studies with adolescents supported the same results(Smits, Soenens, Vansteenkiste, Luyckx, & Goossens, 2009). One study with young studentsprovided compelling evidence supporting the use of autonomous supportive interpersonal styles (as opposed to controlling styles) when teaching novel exercises, which was linked to greater expended effort, more self-determined regulation, greater persistence behavior across the four months, and future involvement in exercise-related clubs (Vansteenkiste, Simons, Soenens, & Lens, 2004). The qualitative data could explain the results of self-regulation, because adolescents disagreed with parents believe that pressure (a program strengths for parents) was necessary to control their children’s adherence to changes. Participants felt pressure and criticism from family members as a program weakness. This situation were explained by the parents desire to help their children, who resulted in a greater control and intrusion (Hills, King, & Byrne, 2007). In fact, parental authoritarian style or the incongruent styles (e.g. authoritarian vs. negligent) or parental practices (e.g. negative role model vs. motivate to the health behavior) between father and mother were associated to higher BMI of the adolescents (Berge, Wall, Bauer, & Neumark-Sztainer, 2010). The strategies of parental control reduced self-esteem (Lowry et al., 2007) and undermined the SDT principles and controlled motivation were not transformed in autonomous motivations (Chirkov, Ryan, Kim, & Kaplan, 2003).
Considering some functional aspects of the program referred by participants asthreats may help us to explain better the observed unchanged variables mentioned above and others as unchanged levels of physical exercise and activity. The monotony of some exercise sessions, the required large waiting time of the consultations (also inhibitory) were the principal threats for adolescents. For parents the threats were, absence of: all exercise sessions supervised, more intense and actualized training and dynamic exercise group classes. According to SDT model, the contextual strategies to promote psychological needs were not sustained by these threats. There were failures in the structure (e.g. unsupervised exercise sessions impede contingent feedback), in the autonomous support (e.g. the monotonous training could impede choice and fun), and in the involvement (desire of group sessions and more support)(Wilson et al., 2008).
The worst perceptions of father warmth after intervention can be explained by their lower involvement in the program, because it was mainly the mothers who accompanied their children to the sessions. The focus groups sample was mainly mothers, who enhanced the relevant role reversal when daughters incentive them to adopt healthier habits, and the transference of the same habits for all family members. But this attitude was not sufficient expressed in quantitative results (perceptions of mothers support is not higher after four months), probably due to their control attitude referred above.
With the exception of relatedness, the results of the quantitative data suggest that the intervention was not long enough (and perhaps even without an autonomous support climate) to promote the other SDT variables, the physical activity level and also to decrease the BMI. A minor impact might have occurred in the parents, because the adolescents’ perception of parents’ support had no positive changes. Nevertheless, qualitative data showed that parents and adolescents agreed with the relevance of multidisciplinary interventions for weight management, although considering the physical exercise as the most important to promote social and psychological benefits. The interpersonal climate between peer, with staff and parents could influence motivation and basic psychological needs. Self-regulated strategies were essentials to promote self-efficacy, nurturing basic psychological needs and promote autonomous motivations. These strategies could be developed by staff, who should received supervised training in structure, support autonomous and involvement, teaching also to the parents to diminish the usually control attitude for children.
The major limitations of this study were the absence of a control group. The small sample and the short-term intervention was another limitation to explore long-term influence. Peers influence could be an important mediator to explore in the future. Greater involvement of parents in the intervention, through specific education on autonomous support strategies, could be an important mediator to promote the children’s autonomous regulation and the satisfaction of their basic needs, and thus allowed the adoption of long-term healthy lifestyles.
REFERENCES
August, G. P., Caprio, S., Fennoy, I., Freemark, M., Kaufman, F. R., Lustig, R. H.,... Endocrine Society. (2008). Prevention and treatment of pediatric obesity: an endocrine society clinical practice guideline based on expert opinion. Journal of Clinical Endocrinology and Metabolism, 93, 4576-4599. doi: 10.1210/jc.2007-2458 [ Links ]
Baard, P. P., Deci, E. L., & Ryan, R. M. (2004). Intrinsic need satisfaction: A motivational basis of performance and well-being in two work settings. Journal of Applied Social Psychology, 34, 2045-2068. doi:10.1111/j.1559-1816.2004.tb02690.x [ Links ]
Bardin, L. (2007). A análise de conteúdo. Lisboa,PT: Edições 70. [ Links ]
Berge, J. M., Wall, M., Bauer, K. W., & Neumark-Sztainer, D. (2010). Parenting characteristics in the home environment and adolescent overweight: a latent class analysis. Obesity (Silver Spring), 18, 818-825. doi: 10.1038/oby.2009.324 [ Links ]
Biddle, S. J., & Mutrie, N. (2008). Psychology of physical activity: determinats, well-being and interventions. New York,NY: Routledge. doi: 10.1007/978-1-4471-1793-3
Blair, S. N., Applegate, W. B., Dunn, A. L., Ettinger, W. H., Haskell, W. L., King, A. C., ... Simons-Morton, D.G. (1998). Activity Counseling Trial (ACT): rationale, design, and methods. Activity Counseling Trial Research Group. Medicine Science in Sports & Exercise, 30, 1097-1106. doi: 10.1097/00005768-199807000-00012 [ Links ]
Calderon, J. L., Baker, R. S., & Wolf, K. E. (2000). Focus groups: A qualitative method complementing quantitative research for studying culturally diverse groups. Education for Health, 13, 91-95. doi: 10.1080/135762800110628 [ Links ]
Camden, C., Swaine, B., Tetreault, S., & Bergeron, S. (2009). SWOT analysis of a pediatric rehabilitation programme: a participatory evaluation fostering quality improvement. Disability and Rehabilitation, 31, 1373-1381. doi: 10.1080/09638280802532696 [ Links ]
Chirkov, V., Ryan, R. M., Kim, Y., & Kaplan, U. (2003). Differentiating autonomy from individualism and independence: a self-determination theory perspective on internalization of cultural orientations and well-being. Journal of Personality and Social Psychology, 84, 97-110. doi: 10.1037/0022-3514.84.1.97 [ Links ]
Deci, E. L., & Ryan, R. M. (2002). Handbook of self-determination research. Rochester,NY: The University of Rochester Press.
Deci, E. L., & Ryan, R. M. (2002). The Paradox of Achievement: The Harder You Push, the Worse it Gets. In J. Aronson (Ed). Improving academic achievement: Impact of psychological factors on education (pp. 61-87). San Diego, CA: Academic Press,. doi:org/10.1016/B978-012064455-1/50007-5
Field, A. E., Haines, J., Rosner, B., & Willett, W. C. (2009). Weight-control behaviors and subsequent weight change among adolescents and young adult females. Am Journal of Clinical Nutrition, 91, 147-153. doi: 10.3945/ajcn.2009.28321 [ Links ]
Finkelstein, E. P., & Trogdon, J. P. (2008). Public Health Interventions for Addressing Childhood Overweight: Analysis of the Business Case. American Journal of Public Health, 98, 411-415. doi: 10.2105/ajph.2007.114991 [ Links ]
Flynn, M., McNeil, D., Maloff, B., Mutasingwa, D., Wu, M., Ford, C., & Tough, S. (2006). Reducing obesity and related chronic disease risk in children and young: a synthesis of evidence with 'best practice' recommend. Obesity Review, 7, 7-66. doi: 10.1111/j.1467-789x.2006.00242.x [ Links ]
Grolnick, W. S., Deci, E. L., & Ryan, R. M. (1997). Internalization within the family: the self-determination theory perspective. In J. E. Grusec & L. Kuczynski (Eds.), Parentins strategies and child outcomes: a handbook of contemporary theory (pp. 135-161). New York, NY: John Wiley & Sons, Inc.
Hills, A. P., King, N. A., & Byrne, N. M. (2007). Children, obesity and exercise: prevention, treatment and management of childhood and adolescent obesity (1st ed.). London and New York: Routledge. [ Links ]
Ingledew, D. K., Markland, D., & Medley, A. R. (1998). Exercise motives and stages of change. Journal of Health Psychology, 3, 477-489. doi: 10.1177/135910539800300403 [ Links ]
Lambert, M., Hublet, A., Verduyckt, P., Maes, L., & Van den Broucke, S. (2002). Report on the project: Gender differences in smoking in young people. Brussels, BE: Flemish Institute for Health Promotion. [ Links ]
Larson, N., & Story, M. (2008). The adolescent obesity epidemic: why, how long, and what to do about it. Adolescent medicine: state of the art reviews, 19, 357-379. [ Links ]
Levesque, C. S., Williams, G. C., D., E., Pickering, M. A., Bodenhamer, B., & Finley, P. J. (2007). Validating the theoretical structure of the treatment self-regulation questionnaire (TSRQ) across three different health behaviors. Health Education Research, 21, 691-702. doi: 10.1093/her/cyl148 [ Links ]
Lindelof, A., Nielsen, C. V., & Pedersen, B. D. (2010). Obesity treatment-more than food and exercise: a qualitative study exploring obese adolescents' and their parents' views on the former's obesity. International journal of qualitative studies on health and well-being, 5, 5073-5084. doi: 10.3402/qhw.v5i2.5073 [ Links ]
Lowry, K. W., Sallinen, B. J., & Janicke, D. M. (2007). The effects of weight management programs on self-esteem in pediatric overweight populations. Journal of Pediatric Psychology, 32, 1179-1195. doi: 10.1093/jpepsy/jsm048 [ Links ]
Luttikhuis, O., Baur, L., Jansen, H., Shrewsbury, V., O'Malley, C., Stolk, R., & Summerbell, C. (2009). Interventions for treating obesity in children: Cochrane Database of Systematic Reviews. doi: 10.1002/14651858.cd001872.pub2 [ Links ]
Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55, 68-78. doi: 10.1037//0003-066x.55.1.68 [ Links ]
Ryan, R. M., Patrick, H., Deci, E. L., & Williams, G. C. (2008). Facilitating health behaviour change and its maintenance: Interventions based on Self-Determination Theory. The European Health Psychologist, 10, 2-5. [ Links ]
Sinha, A., & Kling, S. (2009). A review of adolescent obesity: prevalence, etiology, and treatment. Obesity Sureryg, 19, 113-120. doi: 10.1007/s11695-008-9650-4 [ Links ]
Smits, I., Soenens, B., Vansteenkiste, M., Luyckx, K., & Goossens, L. (2009). Why do Adolescents Gather Information or Stick to Parental Norms? Examining Autonomous and Controlled Motives Behind Adolescents' Identity Style. Journal of Youth Adolescents, 39, 1343-1356. doi: 10.1007/s10964-009-9469-x [ Links ]
Stewart, L., Chapple, J., Hughes, A. R., Poustie, V., & Reilly, J. J. (2008a). Parents' journey through treatment for their child's obesity: a qualitative study. Archives of Disease in Childhood, 93, 35-39. doi: 10.1136/adc.2007.125146 [ Links ]
Stewart, L., Chapple, J., Hughes, A. R., Poustie, V., & Reilly, J. J. (2008b). The use of behavioural change techniques in the treatment of paediatric obesity: qualitative evaluation of parental perspectives on treatment. Journal of Human Nutrition and Dietetics, 21, 464-473. doi: 10.1111/j.1365-277x.2008.00888.x [ Links ]
Styles, J. L., Meier, A., Sutherland, L. A., & Campbell, M. K. (2007). Parents' and caregivers' concerns about obesity in young children: a qualitative study. Family and Community Health, 30, 279-295. doi: 10.1097/01.fch.0000290541.02834.e0 [ Links ]
Teixeira, P., Going, S. B., Sardinha, L. B., & Lohman, T. G. (2005). A review of psychosocial pre-treatment predictors of weight control. Obesity Reviews, 6, 43–65. doi: 10.1111/j.1467-789x.2005.00166.x
Tsiros, M. D., Sinn, N., Coates, A. M., Howe, P. R., & Buckley, J. D. (2008). Treatment of adolescent overweight and obesity. European Journal of Pediatrics, 167, 9-16. doi: 10.1007/s00431-007-0575-z [ Links ]
van Wijngaarden, J. D., Scholten, G. R., & van Wijk, K. P. (2010). Strategic analysis for health care organizations: the suitability of the SWOT-analysis. International Journal of Health Planning and Management 27, 43-49. doi: 10.1002/hpm.1032 [ Links ]
Vansteenkiste, M., Simons, J., Soenens, B., & Lens, W. (2004). How to become a persevering exerciser? Providing a clear, future intrinsic goal in an autonomy supportive way. Journal of Sport & Exercise Psychology, 26, 232-249. [ Links ]
Whitlock, E. A., O'Connor, E. P., Williams, S. B., Beil, T. L., & Lutz, K. W. (2008). Effectiveness of weight management programs in children and adolescents. Evidence Report Technology Assessment, Full Report, 1-308. doi: 10.1542/peds.2009-1955 [ Links ]
Wilfley, D. E., Tibbs, T. L., Van Buren, D. J., Reach, K. P., Walker, M. S., & Epstein, L. H. (2007). Lifestyle interventions in the treatment of childhood overweight: a meta-analytic review of randomized controlled trials. Health Psychology, 26, 521-532. doi: 10.1037/0278-6133.26.5.521 [ Links ]
Williams, G. C., Freedman, Z. R., & Deci, E. L. (1998). Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care, 21, 1644-1651. doi: 10.2337/diacare.21.10.1644 [ Links ]
Williams, G. C., Grow, V. M., Freedman, Z. R., Ryan, R. M., & Deci, E. L. (1996). Motivational predictors of weight loss and weight-loss maintenance. Journal of Personality and Social Psychology, 70, 115-126. doi: 0.1037//0022-3514.70.1.115 [ Links ]
Wilson, L. F. (2007). Adolescents’ Attitudes About Obesity and What They Want in Obesity Prevention Programs. The Journal of School Nursing, 23, 229-238. doi: 10.1177/10598405070230040801
Wilson, P., Mack, D., & Grattan, K. (2008). Understanding Motivation for Exercise: A Self-Determination Theory Perspective. Canadian Psychology, 49, 250-256. doi: 10.1037/a0012762 [ Links ]
Acknowledgments
This research wassupportedby Centro de Malária e Outras Doenças Tropicais (CMDT), Instituto de Higiene e Medicina Tropical, Universidade Nova de Lisboa, Portugal. The Portuguese Foundation for Science and Technology (FCT) financed a doctoral grant to the first author during this research. Appreciation is expressed to HBSC Portuguese team, to the Departamento da Criança e da Família of Hospital Centre of North Lisbon, and to the Faculdade de EducaçãoFísica e Desporto of Lusófona University for assisting with data collection.
Endereço para Correspondência
Faculdade de Educação Física e Desporto, da Universidade Lusófona de Humanidade e Tecnologias; e-mail: veloso.susana@gmail.com
Recebido em 15 de Junho de 2013/ Aceite em17 de Março de 2014














