Introduction
Breastfeeding is the optimum feeding method for infants until two years, and this practice has been recommended until the sixth month for all newborns and supported for over two decades by the World Health Organization (HWO) and healthcare professionals in premature newborns (PN)(Lee & Huang, 2022; World Health Organization, 2018). Nevertheless, mothers' breastfeeding decisions are a complex and multifactorial process, thus many stop earlier than they intended before giving birth. WHO estimates that 15 million babies are born preterm (under 37 completed gestation weeks) every year across 184 countries, ranging from 5% to 18% (1 in 10). The evidence strongly supports that breastfeeding newborns receive the best nutrition and optimal nurturance due to close physical contact with their mothers. Breast milk is a complete, natural, alive and suitable food (with rare exceptions) for almost all newborns (Lee & Huang, 2022; Sánchez et al., 2021) with extensive benefits, especially in PN. Breast milk protects against infections and allergies in the first months of life (Sánchez et al., 2021), is crucial for a child´s neuro and psychomotor development and healthy growth, promotes the baby´s better adaptation to food (Han et al., 2019; Monteiro et al., 2020), and reduces neonatal morbidity and mortality (World Health Organization, 2018).
Breastfeeding advantages are multiple and well-known for mother and child, both in the short and the long term, and worldwide is consensual that the best way to feed a child until six months is exclusive breastfeeding (Sánchez et al., 2021). Nevertheless, almost half of mothers who initiate breastfeeding give up during the first month, earlier than they intended (Lima et al., 2019). Previous positive experiences positively influence the mother's decision to breastfeed (Giannì et al., 2016, 2018) as well as having a partner (Lima et al., 2019).
Prematurity is the most frequent cause of bringing to an end breastfeeding, and the barriers that inhibit breastfeeding are mostly linked to PN (low birth weight, comorbidity, ICU environment) and the mother´s conditions (stress and anxiety about PN clinical situation, pain and difficulty during milk extraction, lack of support from health professionals) (Matriano et al., 2022). Overall, prematurity disturbs the maternity project since introduces a gap between the imaginary baby(expected) and the real baby (Lee & Huang, 2022). Breastfeeding a PN in the ICU stressful and hostile environment is a significant challenge for mothers, mainly due to emotional stress and insecurity (Matriano et al., 2022). In ICU mothers face difficulties that can affect their breastfeeding process and decision, such as concerns about PN's clinical condition, early milk extraction, PN's difficulty in suction-swallow-breath coordination (physiological and neurological immaturity), lack of privacy for lactation, and distance from home (Bezerra et al., 2017).
However, literature is scarce focusing on women's feelings about their breastfeeding decisions. Studies focus mostly on the factors that influence women’s pre-birth decisions but fail to point out the reasons that influence mothers’ decisions to stop breastfeeding during the postnatal period, and about personal and contextual features from the mother-centred perspective (breastfeeding giving up too early) (Abugov et al., 2021). From a maternal perspective, knowing the factors that influence the breastfeeding of PN and outlining woman-centred recommendations is relevant to practice. Thus, mapping the needs and challenges experienced by mothers with their PN is the starting point for optimised breastfeeding. In this sense, this scoping review aims to map factors that influence the breastfeeding of PN from the maternal perspective.
1. Methods
The scoping review (SR) methodology follows the Joanna Briggs Institute (JBI) recommendations and adheres to the Preferred Reporting Items for Systematic Reviews (PRISMA-ScR)(The Joanna Briggs Institute, 2017). The SR protocol follows six consecutive stages: (1) formulation and identification of the research question and objective; (2) identification of potentially relevant studies, which will enable the extent and scope of the review's purposes; (3) selection of eligible studies, according to the criteria predefined (4) data extraction and coding, mapping; (5) compiling, summarizing and interpreting the results using a qualitative thematic analysis with the objective and question; (6) reporting the results, identifying the implications for practice or research (Arksey & O’Malley, 2005).
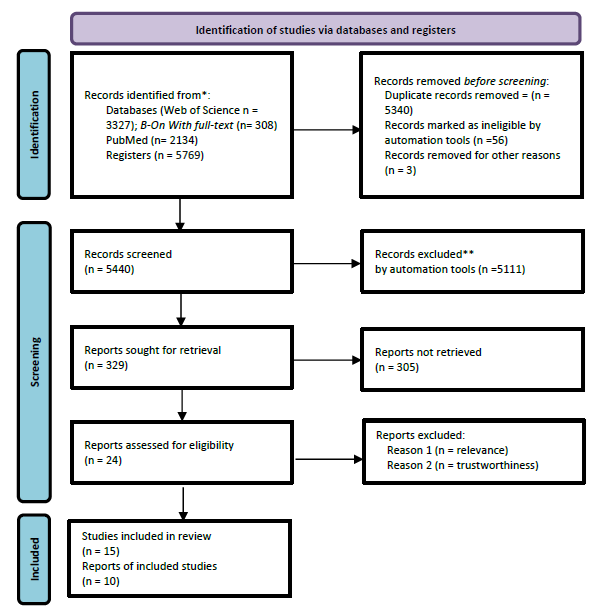
The research question is defined using the acronym PCC (Population-Concept-Context), and the respective results of interest. The SR started with the research question: What factors influence the breastfeeding of PN, according to the mother's perspective? followed by the search strategy protocol using the Boolean operator (AND) or (OR) in English. The database search strategy protocol combined central concepts using PCC acromion (P=Population: Mothers of Premature Newborns, C=Concept: Maternal breastfeeding, and C=Context: Influencing Factors). The search script terms match the Health Science Descriptors with the exact terms Breast Feeding (Mesh ID: D001942), Health Promotion (Mesh ID: D006293), Mothers (Mesh ID: D009035), Nursing (Mesh ID: D009729), Infant, Extremely Premature (Mesh ID: D0062071). Database search was conducted on the Web of Science, Core Collection via Web of Science, B-On with full-text, and PubMed, carried out between December 2019 and January 2021, available in full text in Spanish, Portuguese, and English. The final search protocol included #1: (“mothers*”)AND (“breast feeding*”) AND (“Nursing*”) (“Infant, Extremely Premature*); #2: (“mothers*”)AND (“breast feeding*”) AND (“Nursing*”) (“Infant, Extremely Premature*)AND (“Health Promotion”*); #3: (“mothers*”) AND (“breast feeding*”) AND (“Nursing*”) (“Infant, Extremely Premature*) OR (“Health Promotion”*); #4: (“mothers*”)AND (“breast feeding*”) AND (“Nursing*”) (“Infant Premature*) AND (“Health Promotion”*). The search was also carried out on grey literature using Google Scholar with the following terms: "mothers/mothers AND breastfeeding/breastfeeding AND premature newborn/premature infant". These sources were included to capture all existing research about mothers of PN with no time limit; studies that explore breastfeeding in PN and factors that influence breastfeeding. Figure 1 presents the PRISMA-ScR flowchart diagram to systematise the research process for data extraction.
To assess the relevance and trustworthiness, two authors independently appraised all included articles using the JBI. Studies were excluded if including nurses, health professionals or informal family caregivers as participants; case studies and theoretical reviews; and studies not in Spanish, Portuguese and English. The inspection process reached a consensus and generated fifteen records published, but only ten studies met the inclusion criteria for further analysis. Three researchers (SCMR, CAVS, and PMAP) screened the titles, abstracts, and then full texts of the remaining fifteen articles according to inclusion and exclusion criteria. The full-text papers were read thoroughly, several times to capture all relevant information and to ensure that nothing important was missed. Disagreements were resolved by consensualizing with the researchers (MJN and DT) when required, and finally, results were summarized and reported.
2. Results
Characterization of the Studies
Out of the 5769 articles identified ten met the inclusion criteria. Eight studies are qualitative (using interviews to collect data) and two surveys. Most of the studies (4) were published in 2015, two in 2016 and 2018, and one in 2017 and 2019; Brazilian (6), Italy (2) and China and the USA (1) respectively. In Portugal, no studies were identified. The sample includes only mothers of PN summarizing a total of 721, ranging from 6 to 478. Mothers highlight that breastfeeding is a weighty challenge linked with expected feelings (tiredness, insecurity, anxiety and fear) but intensified given the child's prematurity (Amando et al., 2016), and point some similarities between features that influence positively or negatively breastfeeding PN or term newborns (Yang et al., 2019). It was also evident that breastfeeding maintenance after hospital discharge remains a big challenge, for mothers and health professionals, particularly in the presence of barriers associated with the mother's poor production of breast milk, emotional suffering, unfavourable family environment, or sickness (Matriano et al., 2022). The sample´s studies are coded as A1 to A10 and charted by categories: title; authors, year of publication, country; scope of the study; design, duration, instrument; population/sample; main results and conclusions. Results are presented in Table 1.
Table 1 Summary of the included studies (A1 to A10) - Title, Author, Year/Country, Scope, Design, Sample, Main Results and Conclusions
| Title | Authors/ Year/ Country | Scope of the study | Design, Duration, and Instrument | Population/Sample | Main results and conclusions |
| A1. Breastfeeding in preterm infants after hospital discharge: follow-up during the first year of life. | Méio, et al. (2018) Brazil | Evaluate the prevalence of breastfeeding among preterm infants after hospital discharge | Cohort study Routine consultations, medical records Interviews (May 2005 and October 2010) | 478 PN less than or equal to 33 weeks of gestational, born in the Maternity of Fernandes Figueira Institute for Women, Children, Adolescent Health "Child-Friendly Hospital" and "Care Kanguru" admitted to the NICU and accompanied | This study showed that despite the difficulties in maintaining breastfeeding among mothers of children born preterm, with low gestational age and very low birth weight, it was possible to maintain non-exclusive breastfeeding for up to four months. Breastfeeding is essential in the preterm NB's neuropsychomotor development, healthy growth, and prevention of metabolic disease and obesity. However, breastfeeding after hospital discharge remains challenging for mothers and health professionals. |
| A2. The perception of mothers of hospitalized premature newborns about breastfeeding | Bezerra et al. (2017) Brasil | Understand how mothers perceive the breastfeeding process of their premature child hospitalized in the NICU | Qualitative, descriptive, and exploratory study. Semi-structured interviews. (August to September 2015) | 8 mothers of premature NBs admitted to a unit in the interior of the city of Ceará. | Perception of breastfeeding is essential for the child's growth, development, and hospital difficulties in the quantity and ejection of milk. Maintaining lactation is a complex process that needs to be learned by mothers. Mothers of hospitalized premature infants perceived breastfeeding as an accomplishment achieved by the joint efforts of the mother-child binomial. |
| A3. Mothers' perception about the breastfeeding process of premature newborns in the neonatal Unit | Amando et al (2016) Brasil | To analyze the perception of mothers regarding the breastfeeding process of preterm NB admitted to a Neonatal Intermediate and ICU | To analyze the perception of mothers regarding the breastfeeding process of preterm newborns admitted to a Neonatal Intermediate and ICU | 17 mothers of inpatient preterm newborns in neonatal units of a public maternal-infant hospital in Petrolina, called a child-friendly hospital (Pernambuco/Bahia) | Mothers recognized the vital role of breastfeeding for their premature children, but they found it difficult under hospitalization due to the routines and conditions of the inpatient sector. Breastfeeding hospitalized preterm NB requires special attention from mothers, especially health professionals, who are essential to facilitating mother-child contact during this period, favouring breastfeeding and the consequent reduction in early weaning. |
| A4. Maintenance of breastfeeding for very low birth weight preterm infants: mothers' experiences | Ciaciare, et al (2015) Brasil | Understand the breastfeeding process from the mothers' reports of premature babies and identify factors that facilitated and hindered this process. | A descriptive study with a qualitative approach Interviews May 2011. | 12 mothers of preterm infants at six months of age (Londrina-PR) | Four categories emerged: Previous breastfeeding experience, breastfeeding a premature baby process; emotional context versus breastfeeding process; and managing successes and failures of preterm breastfeeding. Results show that in prematurity, family and professional support, adequate management, and personalized service reception were recognized as primarily responsible for breastfeeding and may even override previous maternal desires. |
| A5. Maternal experiences with specificities of prematurity that make breastfeeding difficult | Pereira, et al (2015) Brasil | Unveil maternal experiences against the peculiarities of prematurity que dificultam a amamentação | Qualitative study interviews (September 2010 and June 2011) | 13 mothers of premature infants care from an outpatient clinic | The results show that when trying to breastfeed a premature baby the mother interacts with situations that she identified as obstacles to breastfeeding: the "torment" of hospitalization and the child's clinical instability, the fear of the baby's death, the breastfeeding struggle, the late-onset, the stress involved to maintain lactation. In addition, breastfeeding, and suckling the breast, can threaten the child's weight gain. |
| A6. Experiences and perspectives on breastfeeding in Chinese mothers separated from their hospitalized premature babies | Yang, Y et al (2019) Pequim | Develop an understanding of mothers' experiences breastfeeding a hospitalized premature NB and the support needed to establish a milk supply during separation from the babies. | A descriptive, qualitative study Semi-structured interviews (2017) | 11 mothers of premature babies hospitalized in three-level III NICUs | Mothers reported mentally and physically challenging breastfeeding experiences during separation from their babies. Although some found breast milk depletion expressive, mothers saw milk extraction as an integral part of their maternal role. With little professional support available, mothers depended on non-professionals to establish breastfeeding. The study identified the difficulties faced by the mothers in establishing a milk supply separate from premature babies and the importance of accessing support from health professionals. |
| A7. Maternal views on facilitators and barriers to premature breastfeeding | Giannì, et al (2018) Itália | Investigate the facilitators and barriers to breastfeeding during a hospital stay, according to the experiences of mothers who gave birth to premature babies | Cross-sectional study Questionnaires (January to June 2016) | 64 Mothers of PN less than or equal to 33s of gestational age | Facilitators of breastfeeding were: health professionals' support, knowledge/ information during hospitalization; proximity to the baby and the implementation of skin-to-skin contact; availability of a pump for milk extraction; The barriers that inhibit breastfeeding: having a premature baby and either low birth weight or being affected by comorbidity; stress and anxiety about the baby's clinical situation; the pain and difficulty during milk extraction and the lack of support from health professionals. The results allow a more thoughtful knowledge of maternal experience about the facilitators and barriers to human milk supply during hospitalization in PN. Mothers indicate that health professionals should modify hospital policies to support breastfeeding and discourse barriers to breastfeeding in preterm infants. |
| A8. Facilitators and barriers to breastfeeding late preterm infants according to mothers' experiences | Giannì, et al (2016) Itália | Identify the facilitators, and barriers to breastfeeding during hospitalization, giving the mother experience who intended to breastfeed and give birth PN. | Cross-sectional study Questionnaires (July to October 2015) | 92 mothers of preterm infants from 34s to 37s of gestational age | Mothers emphasized the importance of receiving specialized lactation support, including the education of health professionals. The most frequently reported inhibitors of breastfeeding are related to prematurity comorbidities (baby drowsiness, medical devices, having twins, and the mother's perception of inadequacy and stress). However, most mothers felt adequately supported by the breastfeeding consultant and health care providers. |
| A9. Support and Barriers to Human Milk Supply by Mothers of African American Premature Babies | LoVerde et al (2018) USA | Qualitatively describe the supports and barriers experienced by mothers when providing their breast milk to their premature babies | A qualitative and descriptive study Semi-structured interviews and medical records | 16 African American mothers | Themes perceived to support breastmilk provision included (1) Being a Mother, (2) NICU environment, (3) community support, and (4) valuable resources. The themes that emerged as barriers to the provision of their breast milk were: (1) maternal illness; (2) milk expression; (3) challenging home environment (4) emotional distress |
| A10. Breastfeeding in premature: knowledge, feelings, and experiences of mothers | Cruz, M.R & Sebastião L.T (2015) Brasil | Analyze the knowledge, feelings, and experiences of mothers of premature babies concerning breastfeeding | Qualitative cross-sectional study semi-structured interviews (March to October 2013) | 20 mothers of premature babies | Regarding mothers' knowledge about breastfeeding, the reports expressed the benefits of this practice, which, for the most part, were limited only to the benefits involving the infant's health. The "positive" feelings occurred more frequently regarding the mothers' feelings. Concerning breastfeeding experiences, the results showed positive expectations regarding the fulfilment of motherhood, although some reports indicated feelings of anguish, fear, and difficulties. The reports also indicated that breastfeeding at home occurred with greater tranquillity. However, there was great concern about weight gain. |
Many psychological, social, cultural and environmental features contribute to the ambivalent attitude toward PN mothers’ breastfeeding.
Mother breastfeeding inhibitors. All mothers reported pain (during breastfeeding, milk extraction, and breast engorgement); low milk production, difficulties in positioning the newborn, lack of sleep quality, and exhaustion/tiredness (Ciaciare et al., 2015). The majority also report fear, anxiety, insecurity, stress, discomfort, the environment of NICU, prematurity and the separation of the infant, difficulty in breastfeeding and breast milk extraction, and scarce support from health professionals (Ciaciare et al., 2015). Mothers report a lack of guidance and support from health professionals and complain about the excess amount of information in a short period, suggesting that information should be fragmented and validated several times (Yang et al., 2019).
Mother breastfeeding facilitators. Mothers point out the family members as an essential support factor, followed by health professionals' support, previous positive experiences of breastfeeding, relevant information, and resources for milk extraction (including successes and failures) (Cruz & Sebastião, 2015; Méio et al., 2018). Personalized care is reported as mainly responsible for the positive influence on breastfeeding, changing mothers' prior decisions/desire not to breastfeed vs breastfeeding success (Ciaciare et al., 2015). Table 2 presents the inhibiting and facilitating breastfeeding factors.
Table 2 Summary of breastfeeding inhibitors and facilitator factors
| Inhibiting Factors | Study code |
|---|---|
| Mother-child separation makes it difficult to bond and establish breastfeeding | A5, A6, A8 |
| Prematurity (premature and low birth weight newborns, sick newborns); immaturity | A1, A4, A7, A8 |
| Hospital environment, ICU admission | A3, A5, A6, A8 |
| Instability, clinical complications of PN | A1, A5, A8 |
| Pain, discomfort, and difficulty in extracting milk | A7, A6 |
| Difficulty breastfeeding (ineffective holding, ineffective sucking, insufficient milk, delayed lactogenesis) | A1, A2, A4 |
| Fears (loss, physical contact), anxiety, insecurity, stress | A1, A3, A4, A5, A6, A7, A8, A9, A10 |
| Lack of support from health professionals | A6, A7, A9 |
| Facilitating Factors | |
| Breastfeeding and milk extraction cultural importance | A4, A8, |
| Mothers suggest prenatal group classes and videos would be helpful as an official booklet. | A6 |
| Kangaroo Method - skin-to-skin contact | A1, A7, A8 |
| Support from health professionals | A4, A7, A8, A10 |
| Support from family members | A4, A9 |
| Positive previous experience or knowing someone who had a positive experience | A7, A8 |
| Decision to breastfeed | A7, A8 |
ICU: Intensive Care Unit | Study Code A1 to A10: The same code used in Table 1 for the articles retained in the analysis
3. Discussion
The current findings reflect that breastfeeding mothers' main difficulties are the anguish of PN´s clinical instability, PN´s separation, and the stress involved in maintaining breastfeeding (Amando et al., 2016; LoVerde et al., 2018; Méio et al., 2018). Parents of PN experience guilt, anxiety, impotence, uncertainty, fear for the baby's future, and suffering associated with routine changes and personal and professional life (Almeida et al., 2020). PN requires specialized ICU for a long time, undermining mothers' expectations and ideals about motherhood during pregnancy meddling in the breastfeeding process (Matriano et al., 2022). Among the difficulties, mothers indicate the NICU environment, surrounded by technologies, as a barrier to natural contact between mother and children and breastfeeding (Amando et al., 2016; Giannì et al., 2016, 2018). Overall, mothers recognize that breastfeeding is essential for the PN hospital recovery, growth and healthy development (Bezerra et al., 2017). Nevertheless, maintaining lactation this a complex process that faces several obstacles that mothers must learn to go through (Méio et al., 2018), like the torment of PN hospitalisation caused by the PN´s clinical instability, low birth weight, comorbidities, and immaturity (ineffective holding and sucking) (Lee & Huang, 2022). But also, due to the mother's insufficient milk and/or delayed lactation, breast pain, discomfort, difficulty in extracting milk, and lack of support from health professionals (Yang et al., 2019), worry, and a sense of abandonment (López-Maestro et al., 2017). The adjusting process to the new reality of motherhood, taken by surprise after childbirth, mothers of PN demonstrate greater ambivalence about their feelings, and several emotions arise, like alienation, despair, and grief, often due to the expectations created during pregnancy (Lee & Huang, 2022). Mothers described themselves as ambivalent, like swaying between hope and hopelessness and fear of the affective bond with the baby in the first weeks (López-Maestro et al., 2017). The combination of adverse factors such as the risk of morbidity and mortality of the child; the crisis atmosphere associated with the NICU; the inevitable separation from the RN; time and cost of hospitalization, produce severe impacts on parents (Matriano et al., 2022). In these circumstances, mothers are more likely to develop blues and/or postnatal depression (Lee & Huang, 2022), and authors argue that a woman’s decision to breastfeed results from the balance between her intrinsic and extrinsic factors, where she tries to find a balance (Matriano et al., 2022). Despite multiple barriers, mothers of hospitalised PN perceived breastfeeding as an accomplishment achieved largely through the joint efforts of the mother-child binomial (Bezerra et al., 2017). However, after the shock and surprise phase, the parents start the second stage - the bonding process, starting to build a relationship with the new and real baby, not the idealised one (López-Maestro et al., 2017). This process between the mother and the PN must begin as early as possible, for instance, through the kangaroo technique with skin-to-skin contact and frequent breastfeeding (Bruce et al., 2022; Pereira et al., 2015). The Kangaroo technique increases the mother's self-esteem, sense of competence and confidence in caring for the baby, and promotes bonding and trust ensuring a greater success rate in breastfeeding (Bruce et al., 2022; Sweeney et al., 2017). Also, reduces mothers' anxiety and stress, eases breastfeeding (Bezerra et al., 2017; Méio et al., 2018a) is associated with a decrease in the NICU length stay, the risk of post-traumatic stress and post-partum depression (Abugov et al., 2021).
Parenthood adjusting to PN is an urgent issue, thus NUIC professionals must find supportive environmental mechanisms to help families overcome this complex transitional crisis, especially mothers (Abugov et al., 2021). The opportunity to stay with the PN during hospitalisation promotes the mother-infant bond and strengthens, mothers´ calmness and happiness, which in turn, increases milk production (Lee & Huang, 2022). Mothers must be empowered by healthcare staff to increase self-efficacy and reduce negative feelings and emotions. The NICU´s multidisciplinary team is crucial in this adaptation process and must adopt the family-centred care model, which focuses on strengthening affective bonds in the family by providing continuum support from the PN's admission to the home, after discharge (Lee & Huang, 2022) since mothers of PN need to be supported by partners, family, and friends (LoVerde et al., 2018). Particularly, NICU nurses are key elements in building flexible care plans to prepare parents for autonomous parenting based on their needs, and respect for their culture and beliefs (Abugov et al., 2021; Bruce et al., 2022). The nursing strategies to provide parents with emotional and practical support include educational and nutritional programs, developing coping skills, support groups, NP-adapted developmental care, telenursing, and spiritual care (Lee & Huang, 2022). Furthermore, nurses are actively facilitating agents helping mothers gain confidence and security, defeat fears, clarify doubts and help support the difficulties that arise in the breastfeeding process of PN (LoVerde et al., 2018). Supporting mothers towards breastfeeding practices must begin by focusing on the features tailored for a woman's comfort so she can feel safe about breastfeeding decisions.
The study has some limitations. Several papers were excluded due to the Chinese language, and the time interval of the article´s search protocol may have excluded relevant articles. These results encourage an active change in healthcare practices like woman-centred care, family education about breastfeeding and mother-child bonding. Further research must be conducted to provide evidence for mother-child bonding practices and a supportive breastfeeding environment. Also, future investigations must study the weight of the difficulties most reported by mothers in dropout breastfeeding PN. Finally, a systematic review will assess the effectiveness of nurse strategies and interventions to assist and support optimal breastfeeding practices.
Conclusion
From the mothers' perspective, the factors that positively and negatively influence the breastfeeding process of PN are complex and multifactorial. The inhibitors most reported were fear, anxiety, insecurity, stress, prematurity, pain and discomfort, the NICU environment, mother and child separation, and difficulty in breastfeeding and extracting milk. As positive factors, mothers mention active support and guidance from health professionals to establish and sustain good breastfeeding practices, and to feel safe and comfortable. The review reinforces the nurses' role as active players in promoting, protecting, and educating families about women's breastfeeding needs and mother-child bonding. Approaches to promote and support breastfeeding must be mother-centred and consider the mother's social network, where she can feel safe and comfortable about breastfeeding.
How might this information affect nursing practice?
The review reinforces the nurses' role as active players in promoting, protecting, and educating families about women's needs for breastfeeding. Adds knowledge to empower mothers, healthcare professionals, teachers, and nurse students about caring (woman-centred care) for post-partum and breastfeeding in all care contexts. Results encourage active behavioural changes to provide supportive environmental care about breastfeeding and mother-child bonding.
Author contributions
Conceptualization, M.J.N., S.R., C.S., P.P. and D.T.; data curation, M.J.N., S.R., C.S. and P.P.; formal analysis, M.J.N., S.R., C.S., P.P. and D.T.; investigation, M.J.N., S.R., C.S., P.P. and D.T.; methodology, M.J.N., S.R., C.S., P.P. and D.T.; project administration, M.J.N.; resources, M.J.N., S.R., C.S., P.P. and D.T.; supervision, M.J.N. and D.T.; visualization, M.J.N., S.R., C.S., P.P. and D.T.; writing-original draft, M.J.N., S.R., C.S., P.P. and D.T.; writing-review and editing, M.J.N. and D.T.