Introduction
According to the World Health Organization (WHO) 1, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) still represents the most critical ongoing global healthcare challenge. Since the beginning of the pandemic, the numbers of confirmed cases and deaths have increased exponentially worldwide (682,664,563 cases, 6,820,879 deaths as of March 21, 2023) 2.
Despite the WHO declaration about the end of COVID-19 as a public health emergency, this organization warns of the fact that the SARS-CoV-2 still kill and still change and the risk remains to new surges in cases and deaths 3. Older adults continue to be vulnerable to infection by SARS-CoV-2 with higher mortality rates compared to younger populations 4. Additionally, among older adults, the severity of SARS-CoV-2 is more prominent and associated with a higher risk of complications, such as greater rates of hospitalization and intensive care unit admissions 5-7, and this risk increases in adults over 85 years 5.
People infected by the SARS-CoV-2 have shown a wide range of symptoms that appear 2-14 days after exposure to this virus. The typical symptoms are fever or chills, cough, shortness of breath or difficulty breathing, muscle or body aches, headache, loss of taste or smell, sore throat, and congestion or runny nose. However, other possible symptoms could be present, especially among older adults, without fever or respiratory symptoms 8,9. In this population, the infection often manifests as subtle and unusual symptoms occurring outside the usual rubric of traditional signs and symptoms, called atypical presentations. These presentations include (a) a vague presentation of illness; (b) an altered presentation of illness; and (c) a non-presentation of illness 10. The knowledge of COVID-19 symptoms in older adults has increased during the pandemic, as has the recognition that this group is more likely to have an atypical presentation 11.
The atypical presentations of COVID-19 refer to patients where the constitutional or respiratory symptoms are absent or minimal, and other non-respiratory symptoms or signs are early or predominant features 12. With the growth of the pandemic, reports of atypical presentations are emerging globally 12. Comparatively, with younger patients, older adults with COVID-19 have more atypical presentations. Different studies have reported atypical presentations of COVID-19 13, but the results might vary according to the context (e.g., hospital, community, long-term care), methodological design and definitions of typical or atypical presentations. A community study reported that about 40% (n = 122) have had atypical presentation of COVID-19 (fall-36%, reduced mobility-36%, and delirium-22%). In hospital admission, many older adults had no respiratory syndromes (52%) 14, but they were more likely to present geriatric syndromes, such as delirium 8,14-16, functional decline 14, and falls 8,14. A retrospective study in three medical departments in Denmark with patients ≥80 years old reported that atypical COVID-19 symptoms related to geriatric frailty syndromes were frequent, namely, confusion (29%), walking difficulty (13%), and falls (8%) 8. These atypical symptoms were reported in other studies with hospitalized older adults, especially delirium/confusion and falls 17,18. Other symptoms have been reported, such as hiccups 19, Herpes Simplex Virus-1, Conjunctivitis 20, vasculopathy-related cutaneous lesions and intrahepatic cholestasis 21.
These clinical presentations could delay the diagnosis and treatment of SARS-CoV-2, which are of great importance to reducing acute respiratory distress syndrome and complications in this population. During hospitalizations, these atypical presentations of COVID-19, especially delirium, were associated with more adverse outcomes, such as malnutrition, anorexia and higher mortality 9. Despite the recognition of the atypical presentation of COVID-19 in older adults and the link with poor outcomes, there is no consensus in the literature on the categorization of those presentations and the full prevalence and impact in the older population. Given the need for health professionals to have evidence-based information about atypical presentations of COVID-19 among older adults, and its importance in providing timely diagnosis and treatment; this scoping review aimed to identify the atypical presentation of symptoms of COVID-19 in older adults and summarize and synthesize the evidence regarding the clinical outcomes of older adults with atypical presentations of COVID-19.
Method
This scoping review was guided by the framework proposed by the Joanna Briggs Institute 22. Our study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for a Scoping Review 23. The protocol is registered on the International Platform of Registered Systematic Reviews and Meta-analysis (Inplasy protocol 2021100103) 24.
Eligibility Criteria
To be included in this scoping review, studies needed to clearly focus on atypical presentations of COVID-19; be published after December 31, 2019 (the day of confirmation of the first case of COVID-19); be written in English, French, Portuguese or Spanish; participants needed to be aged 60 years or older (older adults according to the United Nations); and performed in a diversity of care contexts, such as, hospitals, long-term care, primary care, community services, and home-based care. Quantitative, qualitative, and mixed methods studies were included, considering different approaches to identify atypical presentation. Quantitative designs involved any experimental studies (randomized or non-randomized controlled trials, quasi-experimental before and after studies and pre-experimental) and prospective and retrospective observational cohort studies; controlled before and after studies; case-controlled studies; cross-sectional studies; and series of cases.
Exploratory and descriptive qualitative studies were also included. Articles that did not fit the participants - concepts - context framework, such as non-atypical signs or symptoms of COVID-19 and age below 60 years, were excluded, as were study protocols, abstract narrative reviews, letters and correspondence reports and protocols.
Search Strategy
The search strategy was created, and the following electronic databases were searched between November 4, 2021, and January 12, 2022: MedLine (via EBSCO), Web of Science (via Web of Knowledge), Nursing and Allied Health: Comprehensive Edition (via EBSCO), MedicLatina (via EBSCO), Scopus, ScienceDirect, CINAHL Complete (via EBSCO), SciELO, World Health Organization International Clinical Trials Registry Platform (apps.who.int/trial search), World Health Organization Global Literature on Coronavirus Disease Database, and the PubCovid-19 platform (http://pubcovid19.pt/eng/).
The final search involved the words “older,” “signs or symptoms,” “atypical,” and “COVID-19.” Detailed search syntaxes can be found in supplementary Material 1 (for all online suppl. material, see https://doi.org/10.1159/000534250). The reference lists of articles included in the review were screened for additional papers. The grey literature search involved DART-Europe and OpenGrey. The final search results were exported into Mendeley (Mendeley Ltd., Elsevier, The Netherlands), and duplicates were removed.
Selection of Evidence Sources
Two independent reviewers (1st and 3rd authors) reviewed titles and abstracts according to the inclusion criteria and retrieved the full texts of articles of interest. If an article could not be obtained from the institutional collections, the corresponding author was contacted to retrieve it, and if there was no response, the article was excluded.
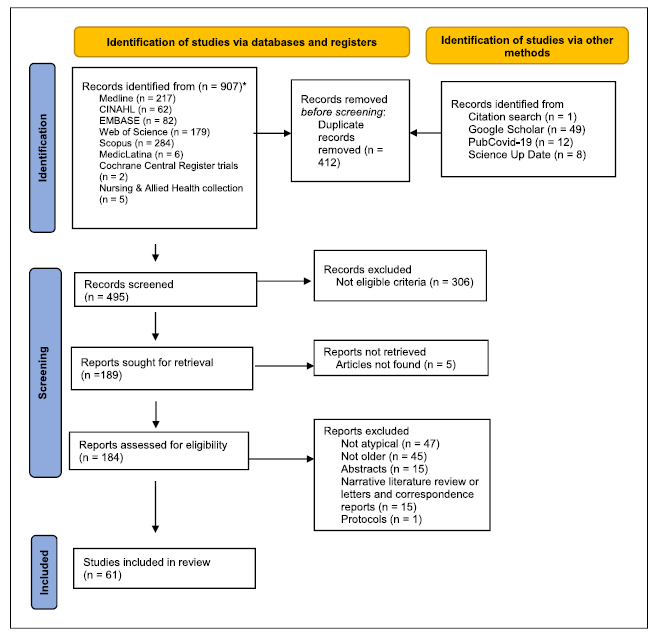
The full text of selected material was divided into three groups of two reviewers for reading and assessing eligibility. To increase consistency between reviewers, each group received the same number of articles to read independently. Inconsistencies were pointed out and resolved by the reviewers in regular meetings. Studies that did not meet the criteria were excluded during this process, and the reasons for exclusion were reported in the Prisma Flow diagram (shown in Fig. 1).
Data-Charting Process
A data-charting form was developed by the first author according to the review questions to determine the variables to be extracted. The data charting included authors and year of publication, country, and study design. The clinical outcomes included the characterization of the population (e.g., sex, age, place of admission), comorbidities, frailty assessment, testing for COVID-19, atypical signs and symptoms, time to present typical syndromes, and prevalence. The adverse outcomes comprised length of stay, mortality, and admission to an intensive care unit. Two reviewers (1st and 3rd authors) independently charted the data, discussed the results, and updated the extraction chart. Eligibility disagreements that could not be resolved were reviewed by a third reviewer (2nd author), who made the final decision.
Synthesis of Results
The studies are organized in tabular form to demonstrate the full scope of the articles about the review questions. Based on the extracted data, a narrative format with a basic numerical analysis (absolute frequency, percentage, median, and standard deviation) was provided in accordance with the aims of this scoping review (atypical symptoms, patient characterization, prevalence, and outcomes).
Results
Study Selection
The literature search identified 907 articles. After removing duplicates (n = 412), 495 titles and abstracts were analysed, 189 were selected for full-text review and 306 were excluded for not meeting the eligibility criteria. Of the 189 works selected, five were not retrieved due to the unavailability of the full text, even after contacting the authors, and 123 were excluded (the main reasons were not atypical presentation - 47 and not older adults - 45), as shown in the PRISMA flowchart (show in Fig. 1). Thus, 61 studies were included, of which 36 (59%) were published in 2020 and 25 (41%) in 2021.
Study Characteristics
All were written in English and conducted in 25 countries, particularly in the USA (8, 13.1%), Italy (8, 13.1%), the United Kingdom (7, 11.5%), France (4, 6.6%), Spain (4, 6.6%) China (3, 4.9%), Denmark (3, 4.9%), Ireland (2, 3.3%), Turkey (2, 3.3%), and Mexico (2, 3.3%). Regarding the study design, 36 (59%) were case reports, with three multiple case reports 24-26, ranging from 2 to 14 patients. A multiple case report included 5 patients, but only 1 patient was aged 60 years older 27 and just this participant was included in this SR. Among the retrospective studies, 18 (29%) were cohort studies, two were longitudinal studies 28,29 and one was a multicentre study 30. The prospective design was found in two studies - one longitudinal and multinational study 31 and one cohort study 32. One was reported as an observational study 33 (online suppl. material 2).
Participant Characteristics
The number of patients (considering only those 60 years or older) ranged from 1 to 40,298 with the median (Q1; Q3): 1 (1;113.75). The case reports included 49 older adults (32 males) with a mean age of 77.88 ± 8.51 years. Twenty-four cases reported the provenience of the patients, with 22 from home, one from a nursing home 24 and 1 including patients from home and nursing homes 25. In the case studies, the most prevalent comorbidities were hypertension (n = 17), diabetes (n = 9), heart attack (n = 6), dementia (n = 6), cancer (n = 3), and hyperlipidaemia (n = 2). In the cohort studies, female participants constituted 56.81 ± 15.68% (ranging from 21.42 to 83%), with ages ranging from 60 to 94 years (mean = 71.88 ± 8.5 years). Six studies reported the median age, which was between 67 and 89 years (Q1; Q3): 75.65 (69.25; 86.75) years. Comorbidities were reported in 19 studies, representing 6,670 patients (with and without atypical presentations).
The most representative comorbidities reported by older adults (n = 19 studies) were dementia/cognitive disability (25.94%); cardiovascular disease (22.73%); neurological problems, such as stroke (9.36%); hypertension (10.06%); pulmonary disease (7.87%); diabetes (6.62%); kidney disease (6.7%); mental disorder (3.4%); congestive heart failure (1.66%); Parkinson’s disease (1.78%); and cancer (0.79%). Two studies presented the comorbidities of patients with an atypical presentation, with hypertension being the most prevalent in both (57% and 72%, respectively), followed by diabetes (35% and 44%, respectively) 34,35, dementia (33%) 34, and heart disease (49%) 35.
Two studies categorized comorbidities according to the Charlson Comorbidity Index, being higher in 49 out of 111 patients 36 and having a median of 2 37. One study used the Cumulative Geriatric-Illness Rating Scale, with a mean of 12.3 and a severity index of 2.36 38. Frailty was assessed in six studies, one with the Frail Non-disabled Survey 38 and five with the Clinical Frailty Scale 9,29,36,39-41. The Frail Non-disabled Survey showed a higher number of older adults with dependency (72, 76.6%) 38. The results of the Clinical Frailty Scale showed that most of the evaluated patients had a cut-off point ≥5 and were thus considered frail.
COVID-19 Test
Regarding the performance of the COVID-19 test, most studies 38 reported administration of the test upon hospital admission or at the onset of the first signs or symptoms. Twelve studies, 10 of which were case reports, did not perform the test upon admission or at the onset of signs/symptoms, mainly because they were atypical. In these studies, the average number of days taken to perform the test was 6.27 ± 4.45 days (1-14 days). One study reported 7-10 days to complete the test 33.
Atypical Presentations of COVID-19
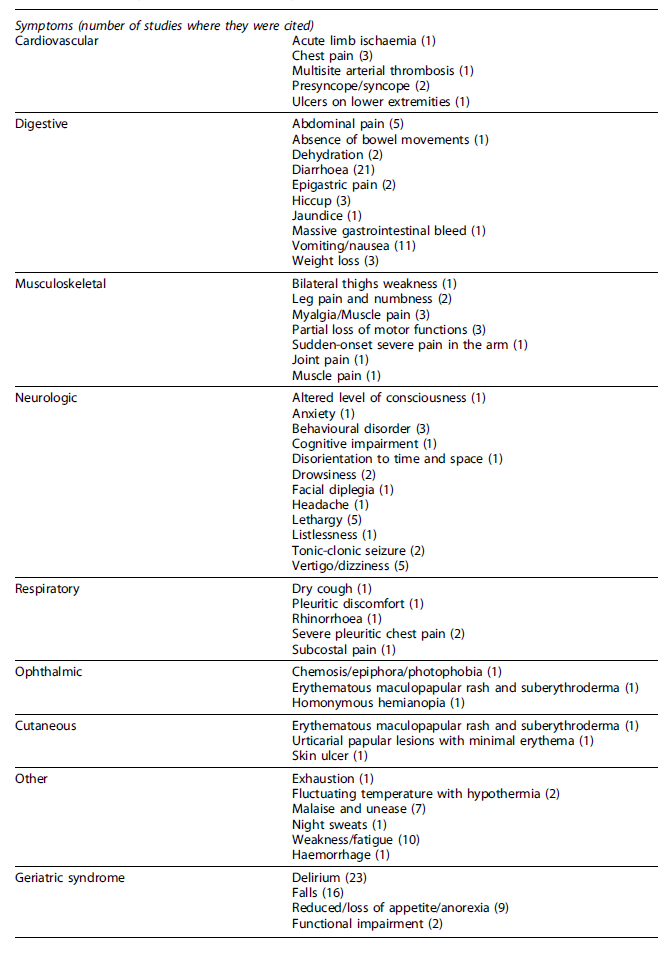
Several symptoms were considered atypical by the authors. Fifty-eight distinct symptoms were identified in the reviewed studies and were classified according to human systems and geriatric syndrome, as shown in Table 1. Most symptoms were digestive (21.41%), neurological (20.67%), musculoskeletal (12.67%), respiratory (10.34%), cardiovascular (8.62%), and geriatric syndromes (6.9%). The ophthalmic and integumentary systems presented three symptoms each one (5.17%).
Delirium was the most frequent geriatric syndrome presented in case studies and cohort studies (n = 23 studies) (Table 2). Among the cohort studies (n = 17), 16 reported the percentage of delirium with a prevalence of 37.1 ± 18.16%, ranging from 9.1 to 67.1% 8,9,16,31,32,34,37-40,42-47. Anorexia (noted in 2 case studies and 7 cohort studies) had a prevalence of 27.25 ± 22.63%, ranging from 2.1 to 61.3% 8,9,28,30,36,42,48. Falls were referred to in 16 studies, of which 12 had a cohort design. In these cohort studies, the prevalence was 16.78 ± 9.45, ranging from 3.8 to 36% 8,9,28,33,34,36-40,42,47.
Table 2 Atypical symptoms, prevalence, and outcomes of COVID-19 in older adults (n = 61)
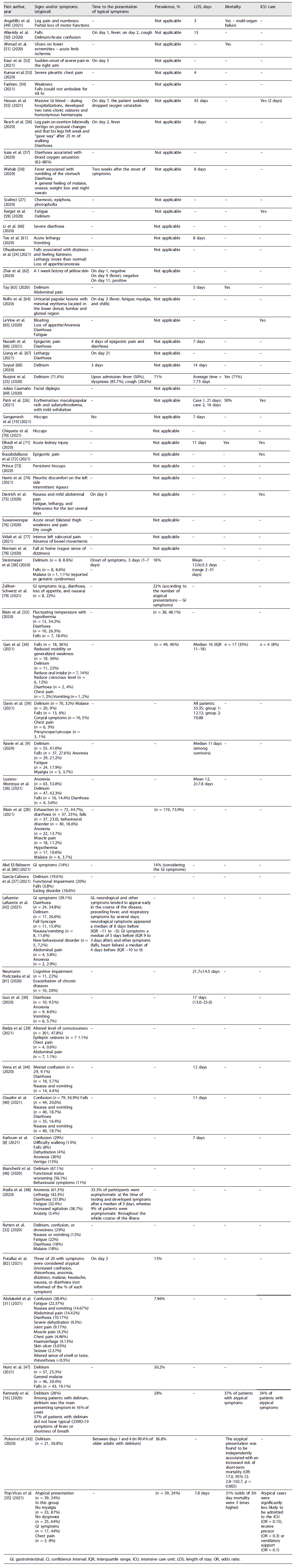
GI, gastrointestinal; CI, confidence interval; IQR, interquartile range; ICU, intensive care unit; LOS, length of stay; OR, odds ratio.
Relating to the gastrointestinal system, diarrhoea (mentioned in 21 studies) and vomiting/nausea (mentioned in 11 studies) were the most mentioned symptoms. Two cohort studies mentioned only gastrointestinal symptoms, with prevalence ranging from 14 to 22% 79,80. Among the gastrointestinal symptoms, the most reported was diarrhoea (n = 11), with a prevalence of 17.21 ± 12.05%, ranging from 3.6 to 37.8% 28,30-34,36,40,42,44,48. The percentage of vomiting/nausea was reported in seven studies, with a prevalence of 9.87 ± 6.02%, ranging from 2 to 18.7% 30-32,34,40,42,44. Other atypical signs and symptoms, such as fatigue, myalgia, or malaise, were also reported but more rarely and sparsely. The time taken for the manifestation of typical symptoms in patients with atypical presentation was rarely presented or unclear in most studies. Those that reported this identified a time ranging from 24 h to 14 days.
Prevalence of Atypical Presentations
Twelve studies reported the prevalence of older adults with atypical presentations, which was 29 ± 18.45%, ranging from 7.96 to 73.9% (Table 2) 16,28,31,33-35,38,43,47,79,80,82.
Adverse Outcomes
Regarding the outcomes, mortality was reported in six case reports (Table 2). Among the reports with more than 1 patient, mortality ranged from 50 26 to 71% 25. Four cohort studies reported mortality as the outcome; of those, three presented mortality rates, with a mean of 34.33 ± 3.06 (31-37%) 16,34,35. Poloni et al. 43 observed that atypical presentation was independently associated with the increased risk of short-term mortality (OR: 17.0, 95% CI: 2.8-102.7, p = 0.002).
Admission to an intensive care unit was reported in seven case reports. In the cohort studies, Kennedy et al. 16 reported 34% of admissions to the intensive care unit. Another study showed that patients with atypical presentation were significantly less likely to be admitted to the intensive care unit (OR = 0.15) or receive a pressor (OR = 0.3) or ventilatory support (OR = 0.1) 35.
In the case reports, the mean length of stay was 9.93 ± 5.03 days, ranging from 3 to 21 days. In the cohort studies, the length of stay was reported in 10 studies with a mean of 14.36 ± 8.63 days, ranging from 7 8 to 35.35 days 39, or a median ranging from 11 9 to 16 days 34.
Discussion
To the best of our knowledge, this is the first scoping review to investigate the atypical presentation of COVID-19 in older adults. This is particularly relevant as atypical symptoms in this population are not yet well established.
The main results showed that studies on atypical presentation have been performed in different contexts (hospitals, emergency rooms, other wards, and long-term care facilities) worldwide (25 countries). However, most of the studies have been conducted in the USA, Italy, the United Kingdom, France, and Spain - that is, countries with the largest older populations (especially in Europe) and the highest rates of COVID-19. In this scoping review, most of the studies were case reports, and most had a single case design. Despite the limited evidence provided by these types of studies, they were very important at the beginning of the outbreak in shedding some light for the medical community on the atypical symptoms in the older population. Nevertheless, cohort studies (prospective and retrospective, n = 25) were also found in this scoping review, representing a higher level of evidence regarding the case studies.
Atypical Presentations of COVID-19
Fifty-eight symptoms were considered atypical. Most of them were classified by organ systems (digestive, neurological, musculoskeletal, respiratory, and cardiovascular) and geriatric syndromes. The atypical presentation of COVID-19 in the organ systems, especially neurological, cardiovascular, ophthalmic, and cutaneous, showed various symptoms that could be infrequent or rare. These results highlight the importance of clinicians being aware of and considering those symptoms to test older adults for COVID-19 11. This is particularly relevant considering the delay in testing for COVID-19 or diagnosing COVID-19 when the first presentation is atypical symptoms, as our SR shows, since they preceded the manifestation of typical symptoms, particularly fever and respiratory signs, by several days (mean 6 days).
The geriatric syndromes considered atypical presentations of COVID-19 constituted a major finding of this scoping review. Among them, delirium (37.1%), anorexia (27.25%), and falls (16.78%) were most prevalent. A multicentric cohort study with a sample of 1,786 patients reported anorexia (33.5%), weakness (29.1%), and delirium (25.1%) as the most common atypical presentations 83. Other systematic reviews reported delirium 84 and falls 85 as the most reported presentations in older adults with COVID-19. The emergence of delirium as a relevant atypical presentation of COVID-19 in the older population reinforces the association of this syndrome with infection in older adults and the importance of considering delirium as a vital sign in older adults. Few studies investigated anorexia, but our results highlight the relevance of this geriatric syndrome, despite the lack of consensus on the conditions commonly considered geriatric syndromes and which ones are most important to detect 86.
Weakness was reported in 10 studies, but it was usually associated with fatigue; it was prevalent only in the results of one study (36%) 34. Regarding geriatric syndromes, a significant number of older adults included in this scoping review had a diagnosis of advanced age, multimorbidity, and cognitive impairment, which are risk factors for atypical presentation of illness in older adults. According to Wong et al. 83, geriatric syndromes may not have a single direct pathophysiological link to COVID-19; rather, it is the combination of an infectious process in a susceptible older population that presents multimorbidity and more frailty.
Moreover, our results showed that the majority of patients assessed for frailty were, in fact, frail and more likely to present with atypical symptoms (e.g., delirium) 40. Wong et al. 83 reported that frailty had a large impact on atypical symptoms compared with robust individuals (61.1% and 38.9%, respectively) and that frailty made a relatively greater contribution to atypical presentation than age. Generally, recognizing and managing geriatric syndromes on their own represent a challenge for health professionals caring for older adults; however, their association with COVID-19 infection has posed an even greater challenge because those professionals have needed to increase their levels of suspicion of COVID-19 infection in older adults.
Prevalence of Atypical Presentations
The prevalence of atypical presentation was 29% but only in cohort studies that presented prevalence results. This value may underestimate the prevalence of atypical presentations by neglecting case studies in which these symptoms were present. Wong et al. 83 reported a prevalence of 66.5% of atypical symptoms (defined as geriatric syndromes) but only when the prevalence of atypical presentation was low (6.2%) because atypical and typical presentations can occur at the same time. In addition, there was a dispersion of results between studies (e.g., 7.96-73.9%), which may be due to the design of the studies, the criteria used to classify typical versus atypical and the sampling procedure. Most of the studies included in this scoping review were case studies, and among those with a cohort design, few reported the prevalence of atypical presentation. However, with the increased number of studies with prospective and retrospective cohorts and case-control and cross-sectional designs, a prevalence review will allow a more accurate determination of the prevalence of atypical presentation of COVID-19 in older adults. Future research focused on atypical presentation should analyse the duration of those symptoms and the impact of COVID-19 reinfection on the manifestation of atypical presentation.
Our findings also evidenced that patients with atypical presentations were older (mean age 78 years), frail and with comorbidities. These conditions could have had three effects: (a) be an underlying cause for of atypical presentations, (b) have potentiated the emergence of atypical presentations, and (c) make recognizing COVID-19 a challenge, often resulting in its delayed diagnosis. Among the chronic conditions presented, hypertension, diabetes mellitus, heart and kidney diseases, and dementia were most preventable, positioning this population at a higher risk of COVID-19 infection. These chronic conditions (particularly hypertension, diabetes, and cardiac disease) may be associated with the emergence of atypical presentation of COVID-19 in older adults and were the most prevalent in patients with COVID-19 13, 87. Furthermore, these chronic diseases were prevalent among older adults in developed countries, such as the USA and European countries, where most of the reviewed studies were performed. For these reasons, further studies using a clear definition and a robust checklist of atypical presentations, precise clinical information (e.g., multimorbidity, prevalence of chronic disease) and study designs with a higher quality of evidence will be relevant to investigate the association between these chronic conditions and the patterns in atypical presentation.
Adverse Outcomes
Few studies reported outcomes - namely, mortality and admission to an intensive care unit. The mortality rate in older adults with atypical presentation was 34.33% - significantly higher than the 11% reported in a systematic review of clinical features and outcomes of COVID-19 in older adults 13. In two studies, mortality was higher than in the control groups 16,35, and that mortality rate was related to atypical presentation 8,48. Other studies found no significant difference in the hospital mortality rate between typical versus atypical presentations 34,87. Wong et al. 83 showed a mortality rate in hospitals of 24.85% among older adults with atypical symptoms. The association between atypical presentations and mortality show conflicting results 87,88. The older population with atypical presentation of COVID-19 had more comorbidities and was frailer. These factors could have a direct and/or indirect effect on the higher mortality reported, not the atypical presentation itself. Future studies should correct for confounders, such as comorbidity, frailty, age, sex, and other typical symptoms developed later in the disease trajectory (e.g., fever, dyspnoea).
Mortality was higher in more common syndromes, such as anorexia (32.8%), weakness (30.6%), delirium (36.6%), and falls (16%), in line with our results indicating that geriatric syndrome was the most prevalent presentation of COVID-19 infection that impacted the mortality rate. In our review, delirium was the most frequent presentation, which could have contributed to the mortality rate found since this geriatric syndrome has been independently associated with mortality in hospitalized older adults with COVID-19 84. Unrecognized atypical presentation, especially in the geriatric syndromes common in older adults, could sustain a low threshold of suspicion of COVID-19, resulting in delayed diagnosis and further contributing to increased mortality.
There is some evidence that older adults with atypical presentation were less likely to be admitted to an intensive care unit. Our results are in line with those of Marziliano et al. 87 showing that older adults with typical presentation were 1.39 times more likely than those with atypical presentation to receive care in an intensive care unit. However, few studies compared the intensive care unit admissions of patients with typical versus atypical presentation 87. It is important to highlight that frailty assessment was lower in the studies included in this scoping review, possibly because of the recommendation of a frailty assessment to help healthcare professionals better stratify the admissions of older adults with COVID-19 to the intensive care unit 88 emerged during the evolution of the pandemic, which could have impacted our findings, which reflected research on the outbreak of pandemic. The length of stay showed diverse results according to the study design and presentation of results (mean or median). Nonetheless, the older adults with atypical presentation had a significantly higher mean length of stay (10 days in case studies and 14 days in cohort studies) compared with other studies involving older adults (8.11 ± 13.97 days) 89. One study that analysed the length of stay of older adults with COVID-19 reported a mean of 9.4 days for those with atypical presentation versus 10.6 days for patients with typical presentation but with no statistically significant difference 87. A prolonged length of stay increased in-patient complications 90, especially in vulnerable populations, such as the population with atypical presentations (e.g., cognitive impairment, delirium, poor nutritional status, and higher comorbidity burden). Therefore, the impact of length of stay on the population must be considered in future studies. Additionally, further research should be performed to gain a better understanding of atypical presentations of COVID-19 in older adults and the clinical outcomes (e.g., mortality, length of stay, intensive care unit admission), and they should analyse other outcomes (e.g., hospital readmission, falls, nutritional status).
Limitation/Future Directions
Our scoping review has some limitations. Firstly, the search was conducted between November 2021 and February 2022, with the included studies having been performed in the first and second waves of the COVID-19 pandemic, most of them case reports. Since then, there have been an increasing number of studies published regarding COVID-19 that must be considered in future research. Consequently, future research must include studies performed during subsequent waves of COVID-19 and analyse the impact of new variants of COVID-19 on the manifestation of atypical symptoms as those variants could present with different symptoms. Additionally, most of the studies reported (59%) were performed before the first COVID-19 administered vaccine (December 8, 2020). Further studies with a fully vaccinated population will be relevant to analyse the association between the impact of vaccines in the atypical presentation of COVID-19 and adverse outcomes.
Secondly, there was significant heterogeneity among the studies in terms of design, setting, patient population, and sample size. This significant heterogeneity might have limited the prevalence results.
Thirdly, the definitions of typical and atypical symptoms of COVID-19 were unclear in some studies and there was also inconsistency in the definitions of atypical symptoms in the literature. This factor contributed to variation among the studies in clinical characterizations of symptoms of COVID-19, making it difficult to decipher what the authors considered typical and atypical. In this scoping review, the atypical symptoms were categorized according to signs and symptoms considered atypical at the time when a study was performed. However, there was enormous heterogeneity of criteria and an overlap between typical and atypical symptoms among the studies, which made it difficult to obtain a clear list of atypical symptoms.
Fourth, several studies did not present data nor clear information about the outcomes of older adults with an atypical presentation, which limited the ability to draw conclusions on this topic. To fill these gaps, more high-quality evidence is needed to understand the link between the outcomes and atypical symptoms of COVID-19 in older adults. Finally, some studies published in other languages besides English, French, Spanish, or Portuguese may have been omitted in this scoping review.
Conclusions
In this scoping review, we found 61 studies that reported 58 atypical presentations of COVID-19 in older adults, highlighting the spectrum of atypical presentations in this population. The geriatric syndromes were the most common atypical presentation in the older population. Delirium, anorexia, and falls were the geriatric syndromes more frequent. The prevalence of atypical presentation was 29%, ranging from 7.96 to 73.9%. Our results showed that older adults with atypical presentation had a mortality rate of 34.33% and were less likely to be admitted to an intensive care unit. This review provides evidence that can support the creation of guidelines for the categorization of atypical presentation in older adults with COVID-19 and highlights the importance of screening this population not only for typical symptoms but also for atypical symptoms. Early recognition of those symptoms remains essential to prevent misdiagnoses, reduce delays in testing for COVID-19, develop interventions to prevent the spread of infection, and initiate treatment and support that could avoid the occurrence of adverse outcomes.
Author Contributions
João Tavares, Daniela Figueiredo, and Larissa Pedreira were involved in the conception and design, analysis, and interpretation of data; prepared the manuscript and gave final approval of the version to be published. Lígia Passos, Leila Sobrinho, and Elaine Souza were responsible for the research, analysed the data and prepared the manuscript. All authors approved the final manuscript.