Artigo breve
COVID-19 and COPD: how it impacted primary healthcare indicators and what can we learn from it
COVID-19 e DPOC: qual o impacto nos indicadores dos cuidados de saúde primários e o que podemos aprender com isso
1 Assistente de Medicina Geral e Familiar; USF Horizonte, ULS Matosinhos, Matosinhos, Portugal
2 Assistente Graduada de Medicina Geral e Familiar; Coordenadora GRESP/APMGF; USF Araceti, ULS Baixo Mondego, Arazede, Portugal
3 Assistente Graduado de Medicina Geral e Familiar; USF Santa Maria - Tomar, ULS Médio Tejo, Tomar, Portugal
4 Assistente Graduado de Medicina Geral e Familiar; Diretor de Internato Médico de Medicina Geral e Familiar; USF João Semana, ULS Região de Aveiro, Ovar, Portugal
5 Médico de Medicina Geral e Familiar; USF Cascais, ULS Lisboa Ocidental, Lisboa, Portugal
6 Assistente Graduado Sénior de Medicina Geral e Familiar; USF Restelo, ULS Lisboa Ocidental, Lisboa, Portugal
7 Assistente Graduado de Medicina Geral e Familiar; Professor Auxiliar Convidado de Medicina Geral e Familiar no Instituto de Ciências Biomédicas de Abel Salazar, da Universidade do Porto; Universidade do Porto, Porto, Portugal
8 Assistente de Medicina Geral e Familiar; Assistente Convidada de Medicina Geral e Familiar no Instituto de Ciências Biomédicas de Abel Salazar da Universidade do Porto; USF Bom Porto, ULS Santo António, Porto; ICBAS, Universidade do Porto, Porto, Portugal
9 Assistente de Medicina Geral e Familiar; Assistente Convidada na Escola de Medicina da Universidade do Minho; USF Gualtar, ULS Braga, Braga; Escola de Medicina, Universidade do Minho; ICVS, Universidade do Minho, Portugal
10 Assistente de Medicina Geral e Familiar; USF Mãe D’Água, ULA Amadora/Sintra, Lisboa, Portugal
11 Assistente de Medicina Geral e Familiar; USF Tondela, ULS Viseu - Dão Lafões, Tondela, Portugal
12 Assistente Convidado na Escola de Medicina da Universidade do Minho, Assistente de Medicina Geral e Familiar; USF Minho, ULS Braga, Portugal; ICVS/Escola de Medicina, Universidade do Minho, Braga, Portugal
13 Assistente de Medicina Geral e Familiar; Diretor de Internato Médico de Medicina Geral e Familiar; USF São Miguel-o-Anjo, ULS Médio Ave, Famalicão, Portugal
Abstract
Introduction:
The COVID-19 pandemic brought challenges and difficulties that impacted the healthcare system, namely the routine management and diagnosis of chronic obstructive pulmonary disease (COPD) at primary healthcare (PHC) units.
Objectives:
To reflect on the impact of the COVID-19 pandemic on COPD management at PHC.
Methods:
We analyzed the publicly available COPD indicators, considering monthly data between Dec/2018 and Feb/2020 (pre-pandemic), Mar/2020, and Jun/2021 (pandemic), and Jul/2021 and Sep/2022 (post-general population vaccination against COVID-19).
Results:
Before the pandemic, there was a growing number of COPD patients in PHC, which reversed after the beginning of the pandemic and remained until the end of 2020. A fast increase was observed during 2021, with a significant decrease in early 2022, coincident with the new pandemic peak. This indicator was stabilizing to values slightly lower than before the COVID-19 pandemic. The eligibility of COPD patients for priority COVID-19 vaccination could have led to an increased COPD codification in PHC. However, the proportion of patients with COPD and FEV1 in the previous three years decreased. The COPD and FEV1 indicators were rising after the last most significant peak of cases in Jan-Feb/2022 but in Sep/2022 were not yet reaching pre-pandemic values. In Sep/2021, 47.1% of PHC patients had a registry of at least one surveillance consultation. Only half of PHC patients (51.3%) had a registry one year later.
Conclusions:
The analysis of the COPD indicators confirmed the significant impact of COVID-19 on COPD management at PHC. The restrictions of patients’ visits and difficulty in conducting spirometry limited diagnostic opportunities; on the other hand, the pandemic increased population awareness of vaccination and respiratory diseases. Beyond this analysis’s primary objective, these results led us to become aware of the need to better identify, follow, and manage COPD patients.
Keywords: COPD; COPD management; Primary healthcare; COVID-19
Resumo
Introdução:
A pandemia COVID-19 trouxe desafios e dificuldades que impactaram o sistema de saúde, nomeadamente a gestão e o diagnóstico da doença pulmonar obstrutiva crónica (DPOC) nos cuidados de saúde primários (CSP).
Objetivos:
Refletir sobre o impacto da pandemia da COVID-19 na gestão da DPOC nos CSP.
Métodos:
Analisaram-se os indicadores de DPOC disponíveis publicamente entre Dez/2018 e Fev/2020 (pré-pandemia), Mar/2020 e Jun/2021 (pandemia) e Jul/2021 e Set/2022 (pós-vacinação da população geral contra a COVID-19).
Resultados:
Antes da pandemia verificava-se um número crescente de doentes com DPOC nos CSP, que se inverteu após o início da pandemia e se manteve até ao final de 2020. Observou-se um rápido aumento durante 2021, com diminuição significativa no início de 2022, coincidente com o novo pico da pandemia. Este indicador estava a estabilizar para valores ligeiramente inferiores aos anteriores à pandemia. A elegibilidade dos doentes com DPOC para vacinação prioritária contra a COVID-19 pode ter levado a um aumento da codificação da DPOC nos CSP. Contudo, a proporção de doentes com DPOC e FEV1 nos três anos anteriores diminuiu. Os indicadores de DPOC e FEV1 estavam a aumentar após o último pico mais significativo de casos em Jan-Fev/2022, mas em Set/2022 ainda não tinham atingido os valores pré-pandemia. Em Set/2021, 47,1% dos utentes tinham registo de pelo menos uma consulta de acompanhamento. Um ano depois apenas metade (51,3%) tinha um registo.
Conclusões:
A análise dos indicadores de DPOC permitiu confirmar o impacto significativo da COVID-19 na gestão da DPOC nos CSP. As restrições nas consultas e a dificuldade na realização da espirometria limitaram as oportunidades de diagnóstico; por outro lado, a pandemia aumentou a consciencialização da população sobre a vacinação e as doenças respiratórias. Para além do objetivo principal desta análise, os resultados permitem refletir sobre a necessidade de melhor identificar, acompanhar e gerir os doentes com DPOC.
Palavras-chave: DPOC; Gestão da DPOC; Cuidados de Saúde Primários; COVID-19
Chronic obstructive pulmonary disease (COPD) has a significant impact on morbidity and mortality. Considering the number of patients registered in the mainland Portugal primary healthcare (PHC) units, there has been a 152% increase in COPD diagnoses between 2011 and 2019, totalizing 137,774 registered patients in December 2019.1
PHC is the primary contact of patients with COPD and plays a critical role in their treatment and improving their quality of life. 2 PHC are essential for prevention, early diagnosis, follow-up, and, whenever necessary, referral of difficult-to-control COPD cases. 2-3 The evaluation of COPD patients’ follow-up on PHC is made by a set of relevant indicators to be recorded and monitored as they set opportunities to improve patient care.
The coronavirus disease 2019 (COVID-19) pandemic has brought challenges and difficulties that impact the healthcare system. Routine management and diagnosis of COPD have entirely changed in many settings, reducing regular face-to-face consultations to severe situations and limiting spirometry and pulmonary rehabilitation. 1,4
Aiming to reflect on the COVID-19 pandemic impact on COPD management at PHC, we analyzed the publicly available COPD indicators of the BI-CSP platform (a solution for clinical and health governance in primary healthcare, available at https://bicsp.min-saude.pt/), considering monthly data between Dec/2018 and Feb/2020 (pre-pandemic), between Mar/2020 and Jun/2021 (pandemic) and between Jul/2021 and Sep/2022 (post-general population vaccination against COVID-19). The National values of the following indicators were analyzed: proportion of patients with COPD with FEV1 evaluation in three years (BI-CSP indicator 2013.049.01); incidence of COPD (BI-CSP indicator MORB.241.01); proportion of elderly or chronic disease with flu vaccine (BI-CSP indicator 2013.030.01); proportion of COPD patients >6 months with flu vaccine (BI-CSP indicator 2021.439.01); and proportion of COPD patients aged 40 years or older with a COPD surveillance consultation registered in the last year (BI-CSP indicator 2021.436.01).
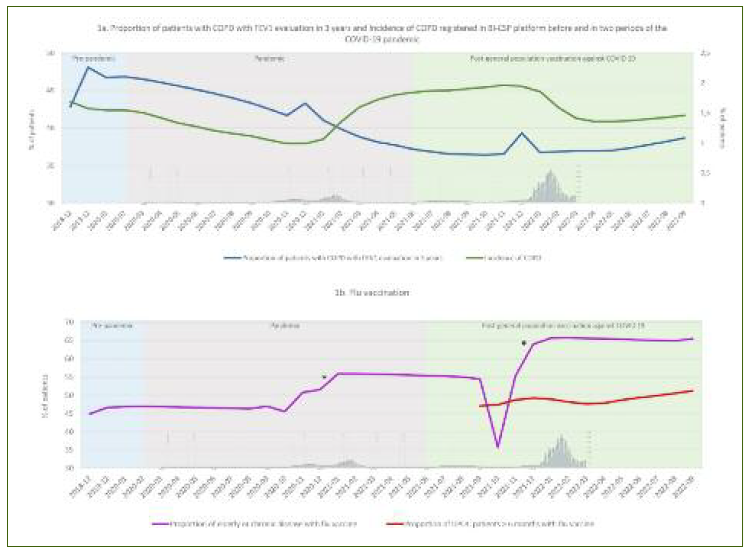
Figure 1 presents the PHC COPD indicators in the three periods and data from the Directorate General for Health (DGS) concerning COVID-19 incident cases between March 2020 and March 2022.
Before the pandemic, there was a growing trend in the proportion of PHC patients with COPD, which reversed after the beginning of the pandemic and remained until the end of 2020. A fast increase is observed during 2021, with a new significant decrease in early 2022, coincident with the new pandemic peak. This indicator was stabilizing to values slightly lower than before the COVID-19 pandemic in September 2022.
To some extent, the evolution of these indicators overlaps the pandemic waves, the infection control measures and lockdowns, and the vaccination periods. The variable diagnostic opportunities due to whether or not patients attended their consult caused by fear of seeking medical assistance or by consultations reductions, patients seeking assistance only in acute episodes and reduced prevalence of seasonal respiratory viruses, may explain the decrease in the number of incident COPD cases, similar to other countries.
The eligibility of COPD patients for priority COVID-19 vaccination may have driven an increase in the codification of this condition in PHC. However, the proportion of patients with COPD and FEV1 in the previous three years has decreased, possibly due to the difficulty in conducting spirometry. During the pandemic, the international recommendations were to restrict pulmonary function testing to selected cases only, limiting the number of regular pulmonary function tests and new diagnoses. 5 The COPD and FEV1 indicators have been increasing after the last most significant peak of cases in Jan-Feb/2022 but in September 2022 were not yet reaching pre-pandemic values.
Since Sep/2021, an indicator concerning the proportion of COPD patients aged 40 years or older with a COPD surveillance consultation registered in the last year is available. In Sep/2021, 47.1% of PHC patients had a registry of at least one surveillance consultation. One year later, in Sep/2022, although an increase of 8.8% was seen, only half of PHC patients (51.3%) had a registry, showing that still much is yet to be done.
The COVID-19 pandemic brought opportunities to reorganize and contemplate specific actions on lung diseases other than COVID-19. Given the disease characteristics, this pandemic led to an increased interest in respiratory illnesses, including COPD. 6 This increased awareness may influence some PHC indicators, namely, the flu vaccination coverage that showed a greater adherence in the last pandemic period (Figure 1b). Data for COPD patients have only been available since September 2020. Still, if it follows the curve of older patients, flu coverage is expected to grow and remain higher than observed before the pandemic. Accordingly, we can assume that the pandemic positively affected awareness among groups at higher risk, namely COPD patients.
The analysis of the COPD indicators of the BI-CSP platform allowed us to confirm the significant impact of the COVID-19 pandemic on COPD management at PHC. The restrictions of patients’ visits and difficulty in conducting spirometry limited diagnostic opportunities; on the other hand, the pandemic increased population awareness of vaccination and respiratory diseases. Beyond the primary objective of this analysis, these results lead us to identify the needs and barriers to COPD management in PHC. There is a need to identify and monitor COPD patients, and there must be available, equitable, accessible resources to achieve this goal. Although the BI-CSP platform allows for more detailed information for registered PHC professionals, this analysis was restricted by access to public data.
There are scarce data on the National prevalence of COPD in Portugal. Considering the 2013 study from Barbara et al. restricted to the Lisbon area, where 14.2% of the population aged ≥40 years old presented COPD, 7 we can assume that the 2022 prevalence of 2.28% among PHC registered patients aged ≥40 years old observed in the BI-CSP platform is highly underestimated. 8 There is undoubtedly a need to identify, follow, and manage Portuguese COPD patients. The availability of management data, contractualized indicators as existing in diabetes or hypertension, a COPD-specific computer system allowing patient surveillance, a structured, scheduled consultation not dependent on exacerbations occurrence, on-time access to spirometry, improvement COPD awareness and knowledge are some of the measures that we believe that would enhance PHC COPD management and health outcomes.
Authors contribution
All authors were involved in the conceptualization, draft version writing and in the final writing, revision and validation of the letter. All authors read and agreed with the final versions of the letter.
Declaration of interest
The authors have no interest to declare.
Funding
Medical writing assistance, supported financially by Boehringer Ingelheim Portugal, was provided by Prime Focus, during the preparation of this article.
References
1. Fundação Portuguesa do Pulmão. Observatório Nacional das Doenças Respiratórias [Internet]. Lisboa: Fundação Portuguesa do Pulmão; 2020. Available from: https://www.fundacaoportuguesadopulmao.org/ficheiros/ondr2020.pdf
[ Links ]
2. Vachon B, Giasson G, Gaboury I, Gaid D, De Tilly VN, Houle L, et al. Challenges and strategies for improving COPD primary care services in Quebec: results of the experience of the COMPAS+ quality improvement collaborative. Int J Chron Obstruct Pulmon Dis. 2022;17:259-72.
[ Links ]
3. World Health Organization. WHO package of essential noncommunicable (PEN) disease interventions for primary health care [homepage]. Geneva: WHO; 2020. Available from: https://www.who.int/publications/i/item/9789240009226
[ Links ]
4. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2023 report [homepage]. GOLD; 2023. Available from: https://goldcopd.org/2023-gold-report-2/
[ Links ]
5. Crimi C, Impellizzeri P, Campisi R, Nolasco S, Spanevello A, Crimi N. Practical considerations for spirometry during the COVID-19 outbreak: literature review and insights. Pulmonology. 2021;27(5):438-47.
[ Links ]
6. Barbosa MT, Morais-Almeida M, Sousa CS, Bousquet J. The 'Big Five' lung diseases in CoViD-19 pandemic: a Google trends analysis. Pulmonology. 2021;27(1):71-2.
[ Links ]
7. Bárbara C, Rodrigues F, Dias H, Cardoso J, Almeida J, Matos MJ, et al. Chronic obstructive pulmonary disease prevalence in Lisbon, Portugal: the burden of obstructive lung disease study. Rev Port Pneumol. 2013;19(3):96-105.
[ Links ]
8. Fundação Portuguesa do Pulmão. Observatório Nacional das Doenças Respiratórias 2022 [Internet]. Lisboa: Fundação Portuguesa do Pulmão; 2022. Available from: https://www.fundacaoportuguesadopulmao.org/ficheiros/ondr_2022.pdf
[ Links ]